Alanderson Passos Fernandes Castro1; Camila Azevedo1; Carolina Ramos Mosena de Angeloni1; Wagner Naves1; Julliana Ferrari Campelo Libório de Santana2
DOI: 10.17545/eOftalmo/2022.0012
ABSTRACT
Paracoccidioidomycosis is a systemic mycosis of great epidemiological importance in Brazil and has a significant impact on rural workers, mainly in tropical and subtropical regions. The disease is transmitted via inhalation of spores and can cause severe systemic manifestations. Ocular involvement is uncommon, and the differential diagnosis includes a wide range of other diseases, which can make it difficult to identify the condition. Treatment is with systemic antifungal agents, but the disease has a relapsing course and progresses to fibrosis of the affected tissues. The present study aimed to report a case of eyelid lesion caused by paracoccidioidomycosis that was initially misdiagnosed as chalazion. The correct diagnosis was later confirmed using excisional biopsy.
Keywords: Fungal eye infections; Hordeolum; Differential diagnosis
RESUMO
A paracoccidioidomicose é uma micose sistêmica de grande importância epidemiológica no Brasil e possui grande impacto na população de trabalhadores rurais, principalmente de regiões tropicais e subtropicais. A doença geralmente é transmitida pela inalação de esporos e pode trazer graves manifestações sistêmicas. O acometimento ocular é incomum e as lesões fazem diagnóstico diferencial com uma ampla gama de outras patologias, o que pode dificultar a identificação da doença. O tratamento se dá com antifúngicos sistêmicos, porém a doença possui um caráter recidivante, cursando com fibrose de tecidos acometidos. O presente artigo busca relatar um caso de lesão palpebral por paracoccidioidomicose que foi inicialmente confundido com calázio, cujo diagnóstico correto foi dado posteriormente após biópsia excisional.
Palavras-chave: Infecções fúngicas oculares; Hordéolo; Diagnóstico diferencial
INTRODUCTION
Paracoccidioidomycosis was first described in Brazil by Adolf Lutz in 1908 and is the most prevalent systemic mycosis among immunocompetent patients in Brazil1-3. It is caused by a dimorphic fungus, Paracoccidioides brasiliensis, which occurs in the mycelium form (sporulating) at room temperature and in the form of yeast at 35°C-37°C, its parasitic form, and can be found in water, vegetation, and soil1,2,4,5. The rural worker population is the most commonly affected, and the disease is more prevalent in tropical and subtropical regions, especially in Colombia, Venezuela, Argentina, and Brazil. The latter has the largest endemic area of paracoccidioidomycosis in the world, especially in the midwest, southeast, and southern regions of the country1. The disease is associated with smoking and alcoholism, but it is not usually associated with immunosuppression like other systemic mycoses2.
The disease is caused by the inhalation of spores, which infect the respiratory tract and spread via the lymphatic (more common) or hematogenous routes1,6. However, the microorganism can also penetrate via the oral, pharyngeal, and intestinal mucosa and by inoculation into the skin, although this is much more uncommon4,5. This case report is about an eyelid lesion caused by paracoccidioidomycosis and includes a brief discussion on it.
CASE REPORT
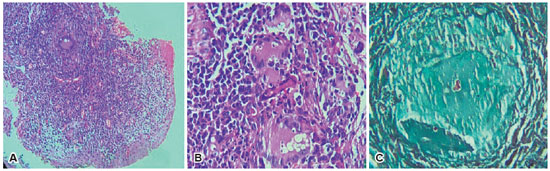
MDS, a 45-year-old man, a heavy machinery driver in the agricultural sector, visited the department with a history of a lesion in the lower eyelid of the left eye that was noted 1 month ago. The lesion had a granulomatous appearance, without secretion or bleeding, and the patient complained of a red eye associated with tearing and itching. He had a history of diabetes mellitus but was not on hypoglycemic drugs. He had been a smoker since the age of 12 and had quit smoking 1 year ago due to the onset of dyspnea on exertion, which had not been investigated. He denied other comorbidities or previous eye surgeries. After a consultation with an ophthalmologist, he was diagnosed with chalazion and started on gatifloxacin 0.3%, dexamethasone 0.1%, and ciprofloxacin ointment 3.5 mg/g with dexamethasone 1 mg/g. He returned to the department after a month because his condition did not improve and the lesion had progressed to an ulcerated, friable appearance. The excision of the lesion was then requested, and the material was sent for pathological examination. The following were the findings: pseudoepitheliomatous hyperplasia associated with a moderate chronic lymphoplasmacytic inflammatory infiltrate in the lamina propria, with several epithelioid granulomas permeated by multinucleated giant cells containing some yeast spherical structures with multiple buds in their cytoplasm, which were highlighted with Grocott special stain (Figure 1). Giemsa and Ziehl–Neelsen special stains were negative, which favored the diagnosis of paracoccidioidomycosis. The patient was then referred to the infectious diseases department for follow-up and treatment.
DISCUSSION
Paracoccidioidomycosis has a wide range of clinical manifestations and can be divided into acute and chronic forms. The acute form is more common in young people, has no sex preference, and affects the reticuloendothelial system, liver, and spleen. The chronic form, which is more common in adults aged 20-40 years, has a preference for men (approximately 10:1) and is associated with pulmonary and mucocutaneous manifestations in addition to those of the reticuloendothelial system, liver, and spleen1,4,7. It can affect any organ of the body but has a preference for the lungs, lymph nodes, and mucocutaneous region, with skin involvement being common in the chronic form; in addition, ocular involvement is rare and, when it occurs, is usually associated with systemic disease8. In the case described above, only ocular involvement was confirmed via biopsy. However, the patient had systemic complaints, such as dyspnea, which could be due to systemic infection by the fungus8. In a case series involving 439 patients with paracoccidioidomycosis, 67% of them had a skin lesion but only 2.5% had eyelid involvement7. The most affected areas are the eyelids (38%), like in the present case, and the conjunctiva (12%), and these are reported in 24% of the cases. The involvement of the retina and uvea has also been reported, although to a lesser extent, and, therefore, a complete ophthalmologic examination with funduscopy should always be performed in these patients8,9.
The disease may initially manifest as a hordeolum or blepharitis; other differential diagnoses are trachoma, sporotrichosis, lupus, tuberculosis, and syphilis. In more advanced stages, the skin lesion may be confused with a neoplasm (such as basal cell carcinoma and squamous cell carcinoma)3,4,7.9. The ocular manifestation begins as a granulomatous lesion, close to the eyelid edge, with subsequent growth and central ulceration and the appearance of fine hemorrhagic points at the bottom, as well as thickened and elevated edges. In this case, the patient did not respond well to the initial therapy for chalazion and presented the characteristic progress of palpebral paracoccidioidomycosis, which contributed to the clinical suspicion. Madarosis is often an early clinical finding, whereas destruction of eyelid layers and eyelid coloboma are later findings1-3,5,9,10. There may also be eyelid edema, tear duct destruction, hyperemia or conjunctival granuloma, secondary infection, and non-painful cervical, preauricular, or submandibular lymphadenopathy1,5,10. In addition, healed or inactive lesions can cause scarring changes in the eyelids (such as ectropion, entropion, and fusion of the eyelid with the globe). Thus, accurate diagnosis and early treatment prevent progression to blindness or mutilating lesions7.
The gold standard in diagnosis is the visualization of the fungus in the material collected from ulcers, secretions, crusts, or sputum via biopsy of the lesion or culture on Sabouraud agar, blood agar, or chocolate agar, with the visualization of its characteristic rudder’s wheel appearance1.3-5. The fungus can be visualized using hematoxylin–eosin staining, but periodic acid Schiff and Grocott stains are extremely useful for differentiating it from other granulomatous diseases, such as tuberculosis and sarcoidosis. In tissue samples, numerous giant cells are observed, some containing fungi, which are large, oval, or round, double-walled, and 5–15 µ in diameter. In addition, there may be areas of abscess with polymorphonuclear reaction and focal areas with necrotic and caseous centers in the periphery of giant cells, macrophages, lymphocytes, fibroblasts, and collagen1.
Treatment involves the use of sulfamide and imidazole derivatives and amphotericin B3,6,9. The most popular drug in Brazil is trimethoprim-sulfamethxaozole, started at a dose of 2.4 g/480 mg for 6 months, followed by a maintenance dose of 1.6 g/320 mg for 2–3 years. Itraconazole at a dose of 100 mg/day for 1 year and ketoconazole at 200–40 mg/day for 1 year are the other options, with amphotericin B reserved for cases of resistance1,2. Although treatment is effective, the disease has a chronic relapsing course and the cure involves fibrosis of the affected tissues, which may require surgical correction of scarring changes7,9. Mortality in severe conditions varies between 2% and 23%, reaching 30% in patients with AIDS. The most common cause of death is respiratory complications due to pulmonary fibrosis and chronic diseases of the lower airways (bronchitis, chronic obstructive pulmonary disease, and emphysema)1.
Despite being uncommon, paracoccidioidomycosis should be considered in the list of differential diagnoses of palpebral granulomatous lesions, mainly depending on the epidemiological profile and risk factors of the evaluated patient. Thus, in view of its potentially serious systemic implications, as well as its locoregional sequelae, early diagnosis and treatment can lower morbidity and mortality of the affected individuals.
REFERENCES
1. Odashiro AN, Odashiro PRP, Fernandes PI, Leite LVO, Odashiro M, Maloney S, et al. Eyelid and conjunctival paracoccidioidomycosis simulating carcinoma. Int Ophthalmol. 2011;31(1):63-7.
2. Cruz AAV, Zenha F, Silva JT, Martinez R. Eyelid involvement in paracoccidioidomycosis. Ophthal Plast Reconstr Surg. 2004; 20(3):212-6.
3. Biasi TB, Ruthner FG, Kronbauer FL. Paracoccidioidomicose da região ocular: relato de dois Ocular paracoccidioidomycosis : report of two cases. An Bras Dermatol. 2004;79(1):69-78.
4. Burnier SV, Sant’Anna AE. Palpebral paracoccidioidomycosis. Mycopathologia. 1997;140(1):29-33.
5. Silva MRBM, Mendes RP, Lastória JC, Barraviera B, Marques SA, Kamegasawa A. Paracoccidioidomycosis: Study of six cases with ocular involvement. Mycopathologia. 1988;102(2):87-96.
6. Cunha BSA, Grecca LS, Chahud F, Cruz AAV. Disseminated Conjunctival Paracoccidioidomycosis. Ophthal Plast Reconstr Surg. 2021;37(4):E153.
7. Ferraz E, Cella W, Rocha E, Caldato R. Paracoccidioidomicose primária de pálpebra e conjunctiva. Arq Bras Oftalmol. 2001; 64(3):259-61.
8. Rassi TNO, Passos RRB, Kumagai KM, Soranz Filho JE, Freitas JAH. Paracoccidioidomicose crônica multifocal tendo como primeira manifestação o envolvimento palpebral: relato de caso. Arq Bras Oftalmol. 2009;72(6):822-5.
9. Rocha GJNM, Nossa LMB, Pinto MR, Marback RL. Paracoccidioidomicose palpebral: relato de três casos. Arq Bras Oftalmol. 2002;65(5):575-8.
10. Belfort Jr R, Fischman O, Camargo ZP, Almada A. Paracoccidioidomycosis with palpebral and conjunctival involvement. Mycopathologia 1975;56(1):21-4.
AUTHOR’S INFORMATION



Funding: No specific financial support was available for this study
Conflict of interest: None of the authors have any potential conflict of interest to disclose
Received on:
July 11, 2022.
Accepted on:
August 7, 2022.