Livia Garcia Biselli1; Marcelo Vicente de Andrade Sobrinho2; André Luís Ayres da Fonsêca3; Laryssa Pereira Alves4; Carolina Peres Batalha5
DOI: 10.17545/eoftalmo/2019.0005
ABSTRACT
OBJECTIVE: To present a case of peripapillary retinal leukemic infiltration without retrobulbar involvement in a patient with T-cell acute lymphoblastic leukemia (T-ALL).
METHOD: Retrospective case report.
RESULTS: A 23-year-old patient diagnosed with T-ALL presented with reduced visual acuity during the course of the disease. Fundoscopy showed optic disk edema, without involvement of the retrobulbar portion of the optic nerve and central nervous system, as shown on nuclear magnetic resonance and cerebrospinal fluid cytology. The patient’s condition progressed unfavorably to papilledema and massive leukemic infiltration as a result of deteriorating clinical status and she consequently died.
CONCLUSION: This is a rare case of peripapillary leukemic infiltration without involvement of the retrobulbar portion (only one similar case was found in the literature). Papilledema facilitated the development of retinal infiltration. Early and adequate assessment is necessary to improve the outcome pertaining to visual prognosis.
Keywords: Leukemia; Leukemic Infiltration; Optic Nerve.
RESUMO
OBJETIVO: Apresentar um caso de infiltração leucêmica retiniana peripapilar sem acometimento retrobulbar em um paciente com leucemia linfoide aguda de células T (LLA-T).
MÉTODOS: Relato de caso retrospectivo.
RESULTADOS: Paciente de 23 anos com diagnóstico de LLA-T e redução da acuidade visual durante o curso da doença. O exame fundoscópico revelou edema de papila sem acometimento de porção retrobulbar do nervo óptico e sem acometimento de SNC evidenciados por RNM e citologia de líquor. O paciente evoluiu desfavoravelmente para papiledema e infiltração leucêmica maciça devido à piora de condições clínicas e foi a óbito.
CONCLUSÃO: Raro caso de infiltração leucêmica peripapilar sem acometimento retrobulbar (apenas um outro caso relatado na literatura). O papiledema facilitou a infiltração retiniana. A abordagem precoce e correta se faz necessária para melhor desfecho em relação ao prognóstico visual.
Palavras-chave: Leucemia; Infiltração Leucêmica; Nervo Óptico.
RESUMEN
OBJETIVO: Presentar un caso de infiltración leucémica retiniana peripapilar sin acometimento retrobulbar en un paciente con leucemia linfoide aguda de células T (LLA-T).
MÉTODOS: Descripción de caso retrospectivo.
RESULTADOS: Paciente de 23 años con diagnóstico de LLA-T y reducción de la agudeza visual durante el curso de la enfermedad. El examen fundoscópico reveló edema de papila sin acometimiento de porción retrobulbar del nervio óptico y sin acometimiento de SNC evidenciados por RNM y citología de líquido cefalorraquídeo. El paciente evolucionó desfavorablemente en papiledema e infiltración leucémica masiva debido al empeoramiento de condiciones clínicas y falleció.
CONCLUSIÓN: Caso raro de infiltración leucémica peripapilar sin acometimiento retrobulbar (sólo existe otro caso documentado en la literatura). El papiledema facilitó la infiltración retiniana. El tratamiento precoz y correcto se hace necesario para un mejor desenlace con relación al pronóstico visual.
Palabras-clave: Leucemia; Infiltración Leucémica; Nervio Óptico.
INTRODUCTION
Ocular involvement in leukemia is frequently observed by ophthalmologists and occurs as a result of direct leukemic infiltration or secondary ophthalmic involvement1. Direct leukemic infiltration has three forms of presentation: anterior uveitis, orbital infiltration, and neuro-ophthalmic signs that include optic nerve infiltration and papilledema. Secondary involvement results from hematological abnormalities related to leukemia, with vitreous hemorrhage or vascular occlusion as complications2.
Optic nerve involvement is recognized as a rarity among these patients. Additionally, the ocular cavity and optic nerve are considered pharmacological sanctuaries owing to the lack of satisfactory results with the use of systemic chemotherapy agents. Therefore, radiotherapy is often indicated for patients with optic disk involvement3, 4.
We described a case of peripapillary involvement due to T-cell acute lymphoblastic leukemia (T-ALL), without involvement of the retrobulbar portion, which progressed unfavorably.
CASE REPORT
A 23-year-old male patient diagnosed with T-ALL in November 2016 and undergoing chemotherapy presented with complaints of visual blurring in the left eye 6 months after the disease was diagnosed. He was referred to the ophthalmology department.
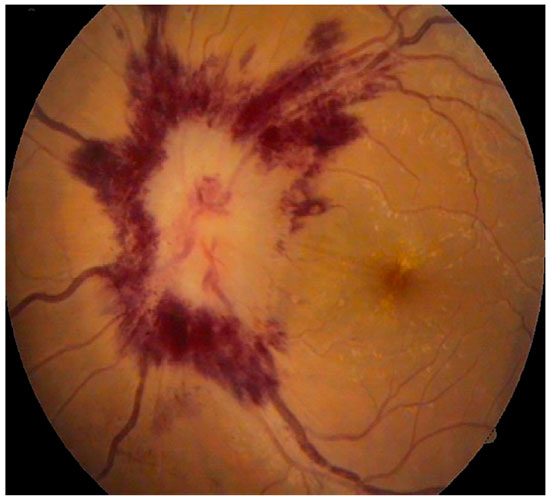
On initial ophthalmological examination, the patient’s best-corrected visual acuity in the Snellen chart was 20/20 in the right eye and 20/40 in the left eye; bilateral examination of the anterior segment showed no changes. Examination of the posterior segment showed slight blurring of the medial margins of the optic disk in the right eye and optic disk edema in the left eye (Figures 1 and 2).

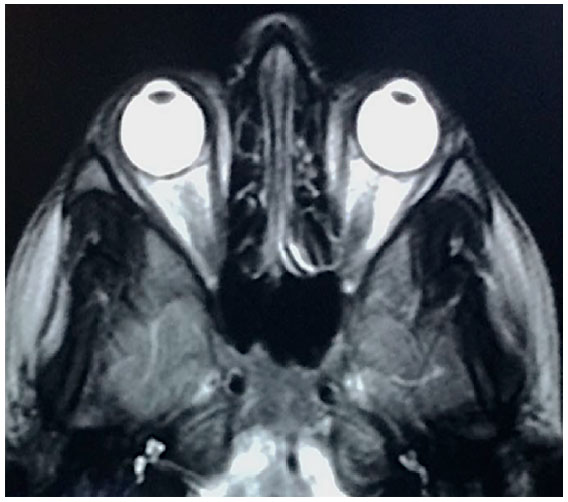
Complementary exams were performed, including NMR, which showed no involvement of the retrobulbar portion of the optic nerve (Figure 3), and CSF cytology showed no evidence of malignancy.
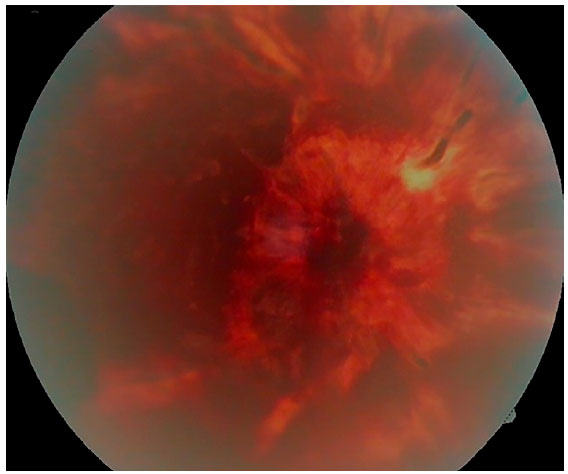
The patient underwent cycles of intrathecal chemotherapy with methotrexate in addition to corticosteroid pulse therapy. Ocular radiotherapy and complementary exams were subsequently requested (optical coherence tomography; fluorescein angiography was clinically contraindicated); however, the patient’s clinical status rapidly deteriorated with disease progression and the exams were not performed. The patient’s visual acuity worsened within a month: absence of light perception in the right eye and 20/60 in the left eye. Fundoscopy showed retinal detachment in the right eye and presence of massive leukemic infiltration, papilledema, and flame-shaped hemorrhages bilaterally (Figures 4, 5).
Ocular radiotherapy and follow-up NMR were not performed because the patient’s condition clinically deteriorated. He was later admitted to the intensive care unit and subsequently died.
DISCUSSION
Papilledema and acute leukemia are not commonly associated, and according to the literature, occurs in 13%–18% of patients. Direct involvement of the optic nerve is even more uncommon and is classified as an extension of the leukemia to the central nervous system through peripapillary involvement only, retrobulbar involvement, or secondary to intracranial hypertension5,6.
In the present case, the initial involvement was solely peripapillary, with no retrobulbar involvement observed. Only one similar case has been reported in the literature in 20167. Papilledema preceded leukemic infiltration, which was facilitated by changes in vascular permeability.
In such cases, an early assessment leads to improved chances of local disease remission and a better visual prognosis.
REFERENCES
1. Sharma T, Grewal J, Gupta S, Murray PI. Eye ophthalmic manifestations of acute leukaemias: the ophthalmologist’s role. Londres: Eye. 2004; 18:663- 672. doi:10.1038/sj.eye.6701308.
2. Reddy SC, Menon BS. A prospective study of ocular manifestations in childhood acute leukaemia. Acta Ophthalmol Scand. 1998; 76:700-703.
3. Nikaido H, Mishima H, Ono H, Choshi K, Dohy H. Leukemic involvement of the optic nerve. Am J Ophthalmol. 1988; 105:294-298.
4. Harma T, Grewal J, Gupta S, Murray PI. Ophthalmic manifestations of acute leukaemias: the ophthalmologist’s role. Londres: Eye. 2004; 18:663-672.
5. Shah P, Yohendran J, Lowe D, McCluskey P. Devastating bilateral optic nerve leukaemic infiltration. Clin Experiment Ophthalmol. 2012; 40(1):e114- e115.
6. Townsend JH, Dubovy SR, Pasol J, Lam BL. Transient optic perineuritis as the initial presentation of central nervous system involvement by pre-B cell lymphocytic leukemia. J Neuro Ophthalmol. 2013; 33(2):162-164.
7. Peripapillary retinal leukemic infiltration associated with papilledema in a T-ALL patient without cranial or optic nerve involvement.




Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: The authors have no potential conflicts of interest to disclose
Received on:
September 19, 2018.
Accepted on:
February 18, 2019.