Bárbara Ribeiro1; Helio de Andrade2; Jivago Queiroz3; João Guilherme Vieira4; Murilo Rodrigues5; Silvia A. Rodrigues6
DOI: 10.17545/eoftalmo/2019.0004
ABSTRACT
Studies on ophthalmic complications due to dengue fever have increased in recent years, following the outbreaks of the disease in various regions of Brazil. Among the ocular manifestations related to the disease, it is important to highlight optic neuritis associated with ophthalmoplegia from dengue infection. The objective of this study was to report an atypical case of post-viral optic neuritis secondary to dengue fever in an 18-year-old woman with a history of characteristic acute febrile syndrome with visual turbidity, ophthalmoplegia, and hyperemia and edema of the optic disc 10 days after the onset of symptoms; the prognosis was good and the signs and symptoms disappeared after 3 months of treatment. The methodology involved analysis of the case and a subsequent discussion based on a literature review on the subject.
Keywords: Dengue/Complications; Optic Neuritis/etiology; Eye Infections, Viral; Case Reports.
RESUMO
Nos últimos anos as complicações oftálmicas advindas da dengue passaram a ser mais estudadas devido ao surto existente em diversas regiões do Brasil. Dentre as manifestações oculares relacionadas a tal doença é relevante destacar a neurite óptica associada à oftalmoplegia por dengue. O objetivo deste estudo foi relatar um caso atípico de neurite óptica pós-viral secundária à dengue em uma mulher de 18 anos com história de síndrome febril aguda característica, apresentando turvação visual, oftalmoplegia, hiperemia e edema do disco óptico 10 dias após o início dos sintomas, evoluindo com bom prognóstico e desaparecimento dos sinais e sintomas após três meses de tratamento. A metodologia englobou a análise do caso e consequente discussão pautada em uma revisão de literatura sobre o tema abordado.
Palavras-chave: Dengue/Complicações; Neurite Óptica/etiologia; Infecções Oculares Virais; Relatos de Casos.
RESUMEN
En los últimos años, las complicaciones oftálmicas derivadas del dengue pasaron a ser más estudiadas debido al brote existente en distintas regiones de Brasil. Entre las manifestaciones oculares relacionadas a dicha enfermedad, es relevante destacar la neuritis óptica asociada a la oftalmoplejía por dengue. El objetivo de este estudio fue describir un caso atípico de neuritis óptica post-viral secundaria al dengue en una mujer de 18 años con historia de síndrome febril agudo característico, presentando turbiedad visual, oftalmoplejía, hiperemia y edema del disco óptico 10 días después del inicio de los síntomas, evolucionando con buen pronóstico y con la desaparición de las señales y síntomas después de tres meses de tratamiento. La metodología englobó el análisis del caso y consecuente discusión pautada en una revisión de literatura sobre el tema abordado.
Palabras-clave: Dengue/Complicaciones; Neuritis Óptica/etiología; Infecciones Virales del Ojo; Informes de Casos.
INTRODUCTION
Dengue fever is a viral disease transmitted by Aedes aegypti and Aedes albopictus, and is geographically distributed in more than 100 tropical and subtropical countries. In Brazil, dengue epidemics are commonplace, making it a public health concern, and even more so because of the several associated problems and complications caused by the disease. Optic neuritis is one of the main ocular manifestations that can occur1,2.
Dengue is the most prevalent form of flavivirus infection in humans, with the number of annual cases exceeding 100 million worldwide. According to the World Health Organization (WHO), 25,000 fatal cases are reported annually. The incidence exceeds 500,000 cases annually in Brazil, and continues to increase despite environmental controls3,4.
A diagnosis of suspected dengue infection is generally made through clinical history; however, it can be confirmed with laboratory tests depending on the time of presentation. Frequently used tests include polymerase chain reaction (PCR) and immunoglobulin M (IgM) or immunoglobulin G (IgG) enzyme immunoassays2,5.
In recent years, ocular complications caused by dengue infection have been observed to be occurring at an increasing frequency by ophthalmologists. However, only a few isolated case reports have been published, and these cases show ocular complications to transitory thrombocytopenia and the resulting hemorrhagic diathesis. Cases with neuro-ophthalmologic manifestations have also been reported. The course of the ocular manifestations was not well-detailed, since it is necessary to describe the case, the spectrum of manifestations, the prognosis, and the treatment of these new, emerging complications1,6,7,8.
Ophthalmoplegia is a type of muscular paralysis caused by neurological involvement and characterized by weakening of the extra-ocular muscles, making movement difficult and potentially leading to paralysis of these muscles. It manifests through atypical presentations with nervous system involvement, including myeloneuropathy, headache, Guillain–Barré syndrome, flaccid paralysis, and neuropathy3,10.
The prognosis of ophthalmologic complications related with dengue infection is favorable. Almost all patients are either asymptomatic or exhibit improved visual acuity and complete resolution of the ophthalmologic complaints. Neurological complications from dengue, although rare, may be the result of direct central nervous system (CNS) involvement1,4,11.
CASE DETAILS
The patient was AENA, an 18-year-old female student, single of mixed race, born and residing in Itapetinga, State of Bahia, Brazil, with a history of acute febrile syndrome, a characteristic of dengue fever, that persisted for 10 days, with visual cloudiness in both eyes (OU). Ophthalmologic exam (April 7, 2016) revealed symmetrical Hirschberg reflexes, black, centered, reactive, isochoric, and symmetrical pupils; direct and consensual photo-motor reflexes were preserved.
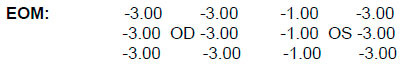
Visual acuity (without correction): OU: 20/20. Biomicroscopy: without changes. Intraocular pressure: 14 mmHg OU at 09:00h. Fundoscopy: clear media, optic disc with edema and exudation, tortuous and dilated vessels, attached retina 360°, macula with normal reflex OU, as shown in the retinography results (Figure 1).
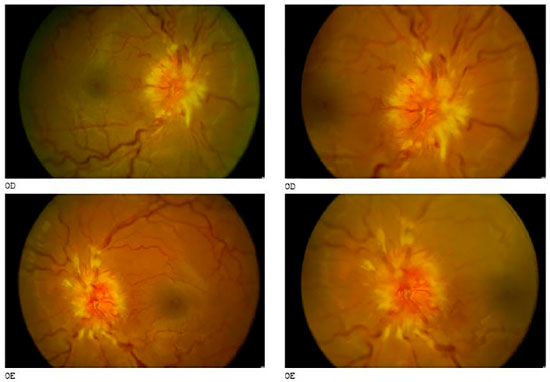
The fluorescein angiography showed intense papillary leakage since the initial phases in both eyes (Figure 2).
The laboratory tests were only positive for IgG dengue antibodies. In the MRI of the orbits, an enlargement of the sheath that covers the optic nerve was observed, associated with flattening of the posterior portion of the sclera.
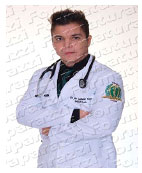
After intravenous treatment with methylprednisolone 250 mg every 6 h for 3 days, followed by oral prednisone 1 mg/kg/day for 15 days with tapering of 10 mg every 5 days, there was a bilateral improvement in the ophthalmoplegia and visual cloudiness. The edema of the optic disc improved gradually, returning to normal at 3 months after the start of the clinical symptoms (Figure 3).
DISCUSSION
Dengue infection is a global public health concern with increasing prevalence every year. The ophthalmologic manifestations related to dengue vary from retro-ocular pain and subconjunctival hemorrhages to optic neuropathy, although the neuro-ophthalmologic manifestation is rare2.
Since the beginning of the new millennium, there has been an increase in the number of reports describing a myriad of ocular signs and symptoms associated with dengue infection6. The precise physiopathological mechanism of the ophthalmologic complications of dengue infection is not well understood; however, several studies mention the possibility of an immune-mediated process as the probable mechanism8. In the present case, the ocular manifestations were detected through clinical evaluation and diagnostic tests.
The primary symptom observed was febrile syndrome, a characteristic of dengue fever, associated with visual cloudiness in both eyes. In the laboratory examination, test results for dengue IgG were positive. This can be explained by the fact that the patient underwent examination at a later stage of infection (10 days after the clinical onset). Moreover, the IgG blood test often identifies a past infection4.
Dengue was diagnosed on the basis of clinical findings correlated with positive dengue serology results, PCR, or both. It is known that patients experiencing dengue symptoms for less than 5 days with a positive PCR but negative IgG serology findings are considered to have a primary dengue infection. Alternatively, patients experiencing dengue symptoms for more than 5 days who have a positive IgG serology finding are classified as having a secondary dengue infection7.
The pathological process of development of ophthalmologic complications of dengue is complex, and the clinical manifestations vary. Ophthalmologic complications are commonly observed in young adults. Despite good recovery of vision and resolution of clinical signs in most patients, general practitioners and primary care physicians should be alert as there are isolated reports of patients with ophthalmologic complications from dengue with poor visual acuity that is refractory to treatment2,3,6.
Because neuro-ophthalmologic manifestations are not a typical symptom of dengue, they are commonly not associated with it. However, studies show that optic neuritis may result from these manifestations, as many patients test positive for dengue without any other symptom that might indicate neuritis or any other condition. In the case reported, we observed that optic neuritis was a result of dengue infection12.
The edema of the optic disc gradually improved, returning to normal within 3 months following the onset of clinical presentation. It is emphasized that the prognosis is usually good, with spontaneous resolution. The use of steroids to treat the visual changes is controversial and there is no specific treatment for dengue infection. Commonly, only nonsteroidal analgesics and antipyretics are prescribed6,9,10. In this case, the treatment option chosen was intravenous methylprednisolone and oral prednisone with tapering, which led to bilateral improvement of the optic disc edema, ophthalmoplegia, and visual cloudiness. Some authors did not report any evidence of in vivo effectiveness of the use of antiviral agents, vascular permeability reduction drugs, or corticosteroids for the treatment of dengue infection. Malta et al10. reported in their study that intravenous administration of 1 g methylprednisolone for 20 min (single dose) reduces mortality in cases of dengue infection7,10.
It is not possible to verify whether the steroids administered had an influence on the outcome of the treatment, as there are no studies that specifically address this point7.
Case reports have described patients with severe vision loss or bilateral involvement who were treated with systemic steroids and occasionally with immunoglobulins. The prognosis of ophthalmologic complications related with dengue infection is favorable; almost all patients are either asymptomatic or exhibit improved visual acuity and complete recovery from the ophthalmologic complications caused by dengue infection3,5,7.
Dengue is usually a self-limited infection. Recovery from the infection with one serotype provides lifetime immunity against that particular serotype; however, this confers only partial and temporary immunity against subsequent infection with other serotypes. Sequential infections with other serotypes may increase the risk of occurrence of more serious systemic diseases, such as dengue hemorrhagic fever or dengue shock syndrome, which can be fatal; hence, proper care is essential in view of the risks inherent to this pathology4,10.
The dengue epidemic in Brazil and this clinical case report, when evaluated together, indicate the urgent need to determine whether patients with ophthalmologic changes should be assessed by ophthalmologists9.
In the present case, symptoms of bilateral visual cloudiness associated with ophthalmoplegia and signs of optic neuritis that manifested 10 days after the onset of infection were observed. Spontaneous recovery of vision could occur; however, in refractory cases, the use of corticosteroids is a treatment option1,6,8.
It should be noted that studies in Brazil have not reported the occurrence of bilateral ophthalmoplegia following dengue viral infection; however, in other countries, there are studies reporting bilateral ophthalmoplegia following chikungunya infection, another viral disease that has ocular manifestations. Inter-nuclear ophthalmoplegia is a rare, notable, and not an often-reported finding that occurs in isolation, without the involvement of any other cranial nerve or long-tract nerve signals, owing to the unique position of the medial longitudinal fasciculus within the brain stem3,9,10.
Owing to the increased incidence of dengue fever in Brazil, this case indicates the importance of conducting an investigational ophthalmologic examination and highlights the importance of its inclusion in the protocol to detect ophthalmologic and CNS changes, which if treated in time, have a prognosis of successful treatment1,6.
It is important for clinicians in countries where dengue fever is common to investigate the association between the dengue infection and ophthalmologic conditions. Although the prognosis is good, there are reports of patients who developed related central scotoma that persisted for months6,12.
REFERENCES
1. Aragão RE, Barreira IM, Lima LN, Rabelo LP, Pereira FA. Neurite óptica bilateral após infecção viral por Dengue: relato de casos. Arq Bras Oftalmol. 2010; 73(2):175-178.
2. Boo YL, Lim SY, Chin PW,Hoo FK. Bilateral optic neuritis with maculopathy: A rare manifestation of dengue fever. Malays Fam Physician. 2017; 12(1):32- 34.
3. Bonilha L, Fernandes YB, Mattos JP, Borges WA, Borges G. Bilateral internuclear ophthalmoplegia and clivus fracture following head injury: case report. Arq Neuro-Psiquiatr 2002; 60(3A):636-638.
4. Yip VC, Sanjay S, Koh YT. Ophthalmic complications of dengue fever: a systematic review. Ophthalmol Ther. 2012; 1(1):2.
5. Chan DP, Teoh SC, Tan CS, Nah GK, Rajagopalan R, Prabhakaragupta M, Chee CK, Tock H, Kong Y. Ophthalmic complications of dengue. Emerg Dis. 2006; 12(2):285-289.
6. Lim WK, Mathur R, Koh A, Yeoh R, Chee SP. Ocular manifestations of dengue fever. Ophthalmology. 2004; 111(11):2057-2064.
7. Verdolin LD, Borner AR, Mussi H, Gismondi RA, Schau B, Ramos RC. A rabdomiólise está associada à febre dengue em um paciente lúpico. Rev Bras Reumatol. 2014; 54(4):318-321.
8. Premaratna R, Jayasinghe KG, Liyanaarachchi EW, Weerasinghe OM, Pathmeswaran A, Silva HJ. Effect of a single dose of methyl prednisolone as rescue medication for patients who develop hypotensive dengue shock syndrome during the febrile phase: a retrospective observational study. Int J Infect Dis. 2011; 15:433-434.
9. Padmamalini M, Avadhani K, Shetty R. Chikungunya and the eye: a review. J Ophthalmic Inflamm Infect. 2013; 3(1):35.
10. Malta JM, Vargas A, Leite PL, Percio J, Coelho G, Ferraro A, Cordeiro T, Dias J, Saad E. Síndrome de Guillain-Barré e outras manifestações neurológicas possivelmente relacionadas à infecção pelo vírus Zika em municípios da Bahia – 2015. Epidemiol Serv Saude. 2017; 26(1):9-18.
11. Figueiredo LTM. The recent arbovirus disease epidemic in Brazil. Rev Soc Bras Med Trop. 2015; 48(3):233-234.
12. Ferreira MLB, Cavalcanti CG, Coelho CA, Mesquita SD. Manifestações neurológicas de dengue: estudo de 41 casos. Arq Neuro-Psiquiatr. 2005 jun; 63(2B):488-493.





Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: The authors have no potential conflicts of interest to disclose
Received on:
October 6, 2018.
Accepted on:
December 11, 2018.