Ana Tereza Ramos Moreira
DOI: 10.17545/e-oftalmo.cbo/2015.6
ABSTRACT
INTRODUCTION: minocycline hydrochloride used to treat acne vulgaris has been associated with the development of pseudotumor cerebri in children and adolescents. Ophthamologic alterations, including papilledema, diplopia, and changes in ocular motility, have been reported.
METHODS: case description based on a review of hospital records and ophthalmology records, including surgical treatment of strabismus.
RESULTS: spontaneous regression of all signs and symptoms except for diplopia and convergent strabismus, which required surgical correction of the ocular deviation.
CONCLUSION: the use of minocycline hydrochloride to treat acne vulgaris should be a last resort, when no other therapeutic option is viable.
Keywords: Pseudotumor Cerebri
RESUMO
INTRODUÇÃO: Cloridrato de minociclina utilizado para tratamento de acné vulgar tem sido associado ao desenvolvimento de pseudotumor cerebral em crianças e adolescentes. Alterações oftalmológicas como papiledema, diplopia e alteração da motilidade extrínseca ocular têm sido relatadas.
MÉTODO: Descrição de caso baseada em revisão de prontuário relacionado a internamento hospitalar e revisão de prontuário oftalmológico incluindo tratamento cirúrgico do estrabismo.
RESULTADO: Regressão espontânea de todos os sinais e sintomas, exceto da diplopia e estrabismo convergente, necessitando correção cirúrgica do desvio ocular.
CONCLUSÃO: Uso de cloridrato de minociclina para o tratamento da acne vulgar deve ser de exceção, quando nenhuma outra opção terapêutica for viável.
Palavras-chave: Pseudotumor cerebral. Hipertensão intracraniana idiopática. Minociclina. Paresia. Cirurgia estrabismo.
INTRODUCTION
Idiopathic intracranial hypertension (NT), also known as pseudotumor Cerebri (PTC), is an increase in cerebrospinal fluid pressure above 20cmH20 in non-obese patients and above 25cmH20 in obese patients. Its cause is unknown. There is no evidence of obstructions within the ventricular system nor are there any alterations in neuroimaging exams. It is more common in obese women of childbearing age.
There is some controversy over the cause of intracranial hypertension. Some argue that all forms of intracranial hypertension, whether idiopathic or secondary, are caused by the venous hypertension or occlusion of venous sinuses.1 However, other authors believe that the alterations occurring in the venous sinuses, including venous hypertension, are secondary to intracranial hypertension itself. King et al. 2 found that if the fluid pressure is reduced, venous hypertension disappears.
Idiopathic intracranial hypertension symptoms include headaches, pulsatile tinnitus, changes in vision, and temporary loss of vision. Diplopia may occur as a result of sixth nerve palsy and papilledema, advanced stages of which can lead to loss of vision.
Many cases of intracranial hypertension are idiopathic; however, the literature describes numerous cases of pseudotumor cerebri associated with the use of antibiotics, including minocycline, doxycycline, and tetracycline. 3,4,5,6,7,8,9,10,11,12,13
Minocycline hydrochloride is an antibiotic from the tetracycline group of antibiotics. It is a semi-synthetic derivative of this group. Like all tetracyclines, its mechanism of action is largely bacteriostatic and is believed to act as a protein synthesis inhibitor. It exhibits antibacterial activity against a wide variety of gram-positive and gram-negative organisms.14
METHODS
This case description was based on a review of the patient's hospital records and past ophthalmology records obtained by the author during the patient's period of treatment.
[Remark 1 ]
CLINICAL CASES
A female patient, 15 years of age, born in the Brazilian city of Curitiba, sought urgent care in the Eye Hospital of Paraná (Hospital de Olhos) on August 7, 2013 with complaints of diplopia and convergent strabismus. From an ophthalmic examination, convergent strabismus in the right eye and papilledema in both eyes were detected. Patient reported 7 days of strong, throbbing frontal headache, fever, phono and photophobia, fatigue, and malaise.
Patient was sent to the neurological unit as intracranial hypertension was suspected. She reported using 100 mg/day of minocycline hydrochloride for 90 days for the treatment of acne vulgaris. She was instructed to cease the use of medication and was then admitted to the hospital to test for intracranial hypertension.
The neurological exam was positive for unilateral (right side) sixth nerve palsy and papilledema. Pupils were equal and reactive to light.
Following were the test results:
Axial CT : Normal
Cerebral MRI: Normal
Lumbar puncture: Clear cerebrospinal fluid (CSF), with no bacteria or fungi. Pressure was 55 cmH20.
Doctors began orally administering 250 mg acetazolamide every 8 hours and pulse therapy for 5 days.
Ophthalmology exam described in the patient's medical records from August 9, 2013 reported persistence of convergent strabismus in the right eye (RE) and left eye (LE) fixation. Hypofunction (-3) of the right lateral rectus (RLR) muscle and hyperfunction (+2) of the right medial rectus (RMR) muscle.
Visual Acuity (VA) with no alterations.
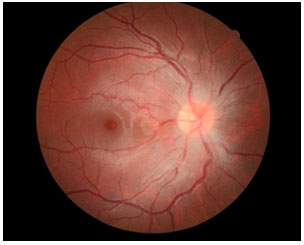
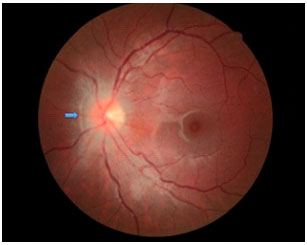
Fundus photographs of both eyes showed poorly defined borders of the papilla, peripapillary hemorrhage, and normal macula.
Normal intraocular pressure in both eyes.
Serology was negative for systemic lupus erythematosus.
After being released from the hospital, the patient saw another ophthalmologist for a second opinion. The following were the exam results:
Horizontal diplopia.
RE static refraction: -2.75 -1.00 at 5° 20/20 VA. [Remark 2]
LE static refraction: -3.00 -0.25 at 180° 20/20 VA.
Fundus photography - Optical papilledema +/++++ in both eyes.
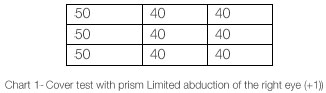
Convergent strabismus (Fig. 1) of 40 40 prism diopters. (Chart 1)

The passive duction test was negative.
After 22 days, fundus photography was used on both eyes and revealed regression of papilledema (Figures 2 and 3).
Automated perimetry showed increased blind spot in each eye.
Thirty days after the onset of symptoms, patient experienced resolution of papilledema in both eyes with 20/20 corrected visual acuity (Snellen); however, she still presented with unchanged ocular motility.
On May 13, 2014, medial rectus recession was performed on both eyes, in addition to recession of the lateral rectus muscle in the right eye; orthotropia occurred immediately and was still present at the patient's last consultation (Figure 4).

DISCUSSION
Cases of PTC in children and adolescents caused by minocycline and tetracycline when used for the treatment of acne vulgaris have been described in the literature since the 1970s, though their pathogenesis remains unclear.4,5,6,7,8,9,10,11,12
Quinn, Singer, and Buncic 11, retrospectively analyzed 153 patients with PTC. They described six patients whose etiology and pathology was associated with the use of tetracyclines (tetracycline in two cases and minocycline in the other four). Of these six patients, five were female and only one of the females was obese. In the largest study of PTC cases associated with minocycline use, which involved twelve cases, six patients were not obese; nine patients (75%) experienced PTC symptoms by the eighth week of treatment.3
A systematic review was performed in 2012 to evaluate the efficacy and safety of minocycline use for acne vulgaris. This review concluded that minocycline is an effective treatment for moderate to severe inflammatory acne vulgaris, but there is still a lack of evidence suggesting that it is better than other, more commonly used therapies. The evidence suggests that minocycline is associated with more severe side effects than doxycycline. Unlike the other tetracyclines, minocycline is associated with lupus erythematosus, though the risk is low: 8.8 cases per 100,000 people are reported per year. The risk of autoimmune reactions increases with prolonged use of minocycline.12
The patient in this case report was tested for systemic lupus erythematosus; however, the possibility was disregarded after the negative results of the serological tests. She was not obese and her PTC symptoms began during the twelfth week of minocycline use (100 mg/day). This is the recommended dose as per the literature for the treatment of acne vulgaris.11
Cranial nerve palsy/paralysis is described in detail in the literature as being associated with minocycline use; cranial nerve VI (the abducens nerve) is the one most commonly affected.3,11,13
In performed literature review, no description of surgical correction of strabismus was found, which suggests that all cases resulted in spontaneous resolution. In this case, 30 days after suspending antibiotic use and initiating PTC treatment with acetazolamide, the patient experienced complete resolution of papilledema with normal visual acuity. However, her diplopia and convergent strabismus persisted and required surgical intervention to resolve.
The patient was embarrassed by the strabismus and became socially isolated. She stopped attending school during the preoperative period.
In this case, it was concluded that not all of the adverse effects of minocycline result in spontaneous resolution and some of them may also have psychological consequences for the patient.
It is recommended for this drug to be prescribed for the treatment of acne vulgaris only when other therapeutic options are not feasible. It is also important to mention the need for consultations and follow-ups with neuro-ophthalmologists for early diagnosis and treatment of any possible side effects that may result from minocycline use.
REFERENCES
1 Karahalios DG, Rekate HL, Khayata MH, Apostolides PJ. Elevated intracranial venous pressure as a universal mechanism in pseudotumor cerebri of varying etiologies. Neurology. 1996:46:198-202. http://dx.doi.org/10.1212/WNL.46.1.198.
2 King JO, Mitchell PJ, Thomson KR, Tress BM. Manometry combined with cervical puncture in idiopathic intracranial hypertension. Neurology. 2002;58:26-30. http://dx.doi.org/10.1212/WNL.58.1.26.
3 Chiu AM, Chuenkongkaew WL, Cornblath WT, et al. Minocycline treatment and pseudotumor cerebri syndrome. Am J Ophthalmol. 1998;126(1):116—121. http://dx.doi.org/10.1016/S0002-9394(98)00063-4.
4 Mochizuki K, Takahashi T, Kano M, Terajima K, Hori N. Pseudotumor cerebri induced by minocycline therapy for acne vulgaris. Jpn J Ophthalmol. 2002;46(6):668-672. http://dx.doi.org/10.1016/S0021-5155(02)00550-6.
5 Monaco F, Agnetti V, Mutani R. Benign intracranial hypertension after minocycline therapy. Eur Neurol. 1978;17(1):48-49. http://dx.doi.org/10.1159/000114921
6 Giles CL, Soble AR. Intracranial hypertension and tetracycline therapy. Am J Ophthalmol. 1971 ;72:981-982. http://dx.doi.org/10.1016/0002-9394(71)91703-X.
7 Stuart BH, Litt IF. Tetracycline-associated intracranial hypertension in an adolescent: a complication of systemic acne therapy. J Pediatr. 1978;92:679-680. http://dx.doi.org/10.1016/S0022-3476(78)80326-6.
8 Walters B, Gubbay S. Tetracycline and benign intracranial hypertension: report of 5 cases. BMJ. 1981 ;282:19-20. http://dx.doi.org/10.1136/bmi.282.6257.19.
9 Pearson MG, Littlewood SM, Bowden AN. Tetracycline and benign intracranial hypertension. BMJ. 1981 ;282:568-569. http://dx.doi.org/10.1136/bmi.282.6263.568-c.
10 Pierog SH, Al-Salihi FL, Cinotti C. Pseudotumor cerebri: a complication of tetracycline treatment for acne. J Adolesc Health Care. 1986;7:139-140. http://dx.doi.org/10.1016/S0197-0070(86)80010-9.
11 Quinn AG, Singer SB, Buncic JR. Pediatric tetracycline-induced pseudotumor cerebri. J AAPOS. 1999;3(1):53-57. http://dx.doi.org/10.1016/S1091-8531(99)70095-9.
12 Garner SE, Eady A, Bennett C, Newton JN, Thomas K, Popescu CM. Minocycline for acne vulgaris: efficacy and safety. 2012 Aug 15. In: The Cochrane Database of Systematic Reviews [Internet], Hoboken (NJ): John Wiley & Sons, Ltd. c1999 - . http://dx.doi.org/10.1002/14651858.CD002086.pub2. Record No.: CD002086.
13 Bababeygy S, Repka MX, Subramanian PS. Minocycline-associated pseudotumor cerebri with severe papilledema. J Ophthalmol. 2009. http://dx.doi.org/10.1155/2009/203583.
14 Lucia R, Oliveira-Filho RM, editors. Farmacologia Integrada. 2a ed. Rio de Janeiro: Revinter; c2004. 678 p.
15 Prieto-Diaz J, Souza-Dias C. Estrabismo. 2a ed. Barcelona: Roca; 1986. 440p.


Comentários
The case study, which is very well documented and presented, is both interesting and important; it is the first report of a case of cranial nerve paralysis associated with the use of minocycline hydrochloride, and no spontaneous resolution was observed.
As described, adult-onset strabismus (in this case study, onset in adolescence) results in functional changes to binocular vision (diplopia), which causes significant esthetic changes and psychological consequences (shame and low seh-esteem). If unresolved, strabismus can lead to personality changes in adulthood. In this case study, the patient even quit school because of complications from strabismus.
Because strabismus may not result in spontaneous resolution, and therefore, may lead to other consequences, it is important for medical professionals who prescribe minocycline hydrochloride to be aware of this report to better evaluate the risks and benefits of its
In this case, the patient experienced a considerably good outcome, owing to early and adequate intervention. Surgery was not needed. It is important to note that, when strabismus onset occurs after childhood, a detailed investigation of the medical history of the patient and the use of medications by the patients must be performed. Other medications, such as simvastatin and ciprofloxacin, have also been reported as the potential causes of strabismus.
Dr. Tomás S. Mendonça
Head of the Strabismus Division, Ophthalmology Department, Federal University of São Paulo Medical School (UNIFESP)
Financial source: no outside sources
Conflict of Interests: the authors declare no conflicts of interest.
Ethical Committee Approval Number / Parecer
Received on:
December 24, 2014.
Accepted on:
January 30, 2015.