Arnonn Afonso Agassi Martelli1; Daniel Traumann1; Licia Deon Weirich1; Cassio Tokuji Tsujiguchi1; Clodomir Salgueiro Cordeiro de Carvalho1; Marcos Solano Vale1; Camila Marinelli Martins2
DOI: 10.17545/eOftalmo/2024.0012
ABSTRACT
This study aimed to assess the prevalence of myopia in children and adolescents, focusing on patients treated at a specialized public-private hospital in the western region of Paraná, Brazil. This cross-sectional, retrospective, and analytical study evaluated the medical records of patients between January 2020 and December 2022. The study included patients aged 5-18 years who were consulted at the study site during the evaluation period. Among the patient population, 46% had myopia, with a predominance of females (57.65%), adolescents (56.44%), and were residents of the city of Cascavel (33.42%). Significant association between the year of diagnosis and age group (p<0.001) revealed an increase in diagnoses in 2020 (COVID-19 outbreak), especially among females. The identification of risk factors, such as sex, adolescents, and the year of diagnosis, highlights the need for preventive approaches and early and specific intervention strategies. There is an urgent need for initiatives that promote outdoor activities and preventive actions, especially during times of crisis, to reduce the prevalence of myopia and protect the eye health of these populations in future.
Keywords: Myopia; Epidemiology; Risk factors; Children; Adolescents.
RESUMO
O presente estudo aborda a prevalência de miopia em crianças e adolescentes, com foco em pacientes atendidos em um hospital especializado público-privado da região Oeste do Paraná. Avaliando prontuários de pacientes atendidos entre janeiro de 2020 e dezembro de 2022, este estudo transversal, retrospectivo e analítico, abrangeu pacientes de 5 a 18 anos consultados no local de estudo no período avaliado. Dos pacientes estudados, 46% apresentaram miopia, com predominância em pacientes do sexo feminino (57,65%), adolescentes (56,44%), e residentes do município Cascavel (33,42%). Uma associação significativa entre o ano do diagnóstico e a divisão etária (p<0,001) destacou um aumento de diagnósticos em 2020 (ano do início da pandemia da COVID-19), especialmente entre as pacientes do sexo feminino. A identificação de fatores de risco, como o sexo feminino, a adolescência e o ano de diagnóstico, destaca a necessidade de abordagens preventivas e estratégias de intervenção precoces e especificas. Ressalta-se a urgência de iniciativas que promovam atividades ao ar livre e ações preventivas, especialmente em períodos de crise, visando diminuir a prevalência da miopia e proteger a saúde ocular futura dessas populações.
Palavras-chave: Miopia; Epidemiologia; Fatores de risco; Crianças; Adolescentes.
INTRODUCTION
Myopia is a condition in which the refractive power of the eye exceeds its axial length. It is categorized into axial or refractive myopia. Axial myopia occurs when the length of the eyeball exceeds the refractive power, whereas refractive myopia occurs when the refractive power exceeds the axial length of the eye. In both conditions, the clinical symptom is low-distance vision1.
High myopia, generally defined as occurrence of − 6.00 diopters or more, has a higher risk of complications that lead to significant and often irreversible low vision, such as macular degeneration, retinal detachment, cataracts, and open-angle glaucoma2.
Myopia is a pathology that has increased considerably in a short time period. It is estimated that by 2050, there will be 1.4 billion people with myopia (22.9% of the world population) and 163 million people with high myopia (2.7% of the world population)3.
A study conducted at a school in a city in the northeast regions of the country showed a prevalence of 20.4% myopia in patients with an average age of 10.6 years4. However, there is a lack of studies showing the prevalence of myopia in other regions of the country.
According to a study conducted in Finland with 240 children who had difficulty seeing distant things and were followed up for 22 years showed that 32% of patients who were diagnosed between 8.8-12.8 years developed high myopia in adulthood5; hence, it is important to assess the onset of myopia.
Some risk factors well-established for the development or worsening of myopia include less time spent outdoors, and greatly engaging in activities that require close-up vision, such as excessive use of screens6. According to a previous study, the anthropometric indices such as older age, heavier weight, taller height, and higher body mass index were observed to be the risk factors for myopia. This study also evaluated low levels of vitamin D as a determinant of myopia, however, no relationship with this factor was noted7.
Another study revealed that female gender, adolescence, and parents with visual impairment are the risk factors for myopia8. However, male gender and the use of screens are associated with higher rates of myopia in children9.
The aim of this study was to analyze the characteristics of the child and adolescent population treated at a specialized hospital, determine the prevalence of myopia among them, and determine possible risk factors for this pathology.
METHODS
This is a cross-sectional, retrospective, and analytical study conducted between January 2020 and December 2022, based on the analysis of medical records at a public-private ophthalmic hospital in the west of Paraná. The study was approved by the ethics committee under approval opinion number 6.271.777/2023.
Patients aged 5-18 years who had consulted an ophthalmologist for symptoms related to vision or routine consultation with myopia reported in their medical records were included. Refractometric evaluations with and without pupil dilation were performed by an ophthalmologist or ophthalmology resident.
In the database analyzed, children were defined as patients aged 5-12 years, whereas adolescents were defined as those aged 13-18 years, who had ophthalmological consultations during the study period. Patients checked outside the proposed period span, those less than 5 years or more than 18 years of age, and those with return visits were excluded.
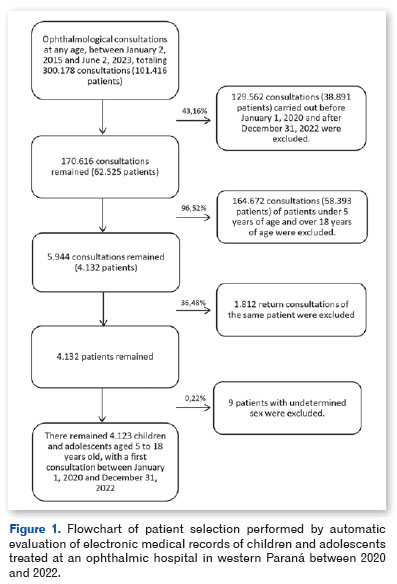
Data was collected by a retrospective analysis of electronic medical records using an automatic tool for extracting textual databases in the R environment10. For this purpose, various functions from the "tidyverse" package were used11. Functions from the "dplyr" package were used to manipulate the database12. The "striprtf" package was used to extract the texts from the patient records13. Figure 1 shows the flowchart of patient selection based on the inclusion and exclusion criteria.
For statistical analyses, we first conducted a descriptive analysis of the data, with estimates of the mean and standard deviation of age, simple and relative frequencies and 95% confidence intervals (CI) of the variables: municipality of origin, sex, age group according to the Instituto Brasileiro de Geografia e Estatística (IBGE) (5-9, 10-14, and 15-18 years), age group according to the WHO division into children and adolescents (children 5-12 years and adolescents 13-18 years), and year of consultation (2020, 2021, and 2022). Chi-square test was used to verify the association between these variables and the occurrence of myopia. Bar graphs, line graphs, and stacked bar graphs were created for better visual representation of the data. All analyses were performed using the R 4.1.0 environment10.
RESULTS
A total of 4,123 patients were analyzed. The overall prevalence of myopia among patients aged 5-18 years during the evaluation period was 45.96% (95% CI, 44.44-47.49). Most patients were from Cascavel, Paraná (33.39%), and the average age was 12.2 ± 3.9 years. Of the patients assessed, 57.65% were female and 56.44% were adolescents (Table 1).
Table 2 presents the factors associated with myopia. Among the female patients, 47.3% had myopia, whereas 44.11% of male patients had myopia. Regarding sex, females were 1.14 times more likely to have myopia than males (p=0.042) in all age groups evaluated, which showed a significant association of myopia and sex.
Among patients aged 5-9 years, 33.83% had myopia, the lowest rate among the three age groups evaluated. There was a significant association between age groups (p<0.001), with patients aged 10-14 years being 1.74 times more likely to have myopia, and those aged 15-18 being 2.38 times more likely to have myopia, compared to patients aged 5-9 years (Table 2).
Comparing children and adolescents, 36.33% of children had myopia, while 53.39% of adolescents had myopia, making them 2.01 times more likely to have myopia than children (p<0.001) (Table 2).
Figure 2 shows the prevalence of myopia in children, adolescents, and both groups together, for each year of the study. For both groups together, 2020 was the year with the highest rate of myopia diagnosis at the first appointment, with 71.2% of the total corresponding to adolescents.
Figure 3 shows the data regarding age, year of diagnosis and, sex of the participants. In 2020, 54% of female children and 52.2% of male children had myopia.
Significant results were obtained when comparing the age range of patients in all the years studied, revealing that adolescent patients are more likely to have myopia than children (Table 3). In this 3-year analysis, the likelihood of presenting with myopia did not change between males and females, with the prevalence of myopia remaining higher in females during the entire study period.
DISCUSSION
The study provides data about the prevalence of myopia from 2020 to 2022, and the most affected age group among the study population. The results show that in 2020, the year of the SARS COV-2 pandemic, highest prevalence of myopia in the study population was observed. One of the measures adopted to prevent the spread of COVID-19 was social reclusion, with the result that schools were closed and distance learning became the norm, through the use of cell phones and computers. In 2020, Brazilian schools remained closed for an average of 279 days14. This period coincides with the high prevalence rate of myopia, demonstrating a possible direct relationship between the lockdown, when people had to stay at home, and the increase in the number of myopic patients. Studies have shown that high screen time and low outdoor activity time are important factors resulting in the development of myopia15,16. There is also evidence that longer exposure to sunlight can prevent axial elongation of the eye17.
Regarding sex, female gender is a risk factor for developing myopia, which is also reported by other studies15,18.
When comparing the patients by age group, higher occurrence of myopia was found in adolescent patients, with other studies reporting a prevalence of myopia of up to 90% among adolescents19. This higher occurrence of myopia in adolescents may be a result of the use of electronic devices in childhood20-22 and/or late diagnosis of existing developed myopia, which increased the risk of complications of high myopia, such as severe irreversible visual impairment23. Therefore, myopia in children increases the prevalence of myopic adolescents, and the likelihood of developing high myopia, due to the longer time it takes to increase the anteroposterior length of the eyeball. Alternatively, earlier the myopia occurrence, higher will be its prevalence5,8.
Given the high prevalence of myopia observed in our study population, it is important to consider the impact of myopia and its complications on health systems, especially in terms of the costs of diagnosis, correction, and treatment. Studies conducted in the United States indicate that the annual cost of myopia treatment and diagnosis in people aged 12-54 years is more than $2 billion (taking into account direct and indirect medical costs, and losses in productivity)24,25. This demonstrates the need for promotion and prevention strategies and actions to improve eye health in children and adolescents.
In this study, data were collected from electronic medical records by searching key words and numbers, and that not all ophthalmological examinations were performed by the same professional. These factors may represent an important study limitation, given that medical records have not been standardized. Another limitation of this study is that it did not stratify the degree of myopia presented by the patients; therefore, it was not possible to analyze the severity of pathology in the affected population.
To conclude, this study revealed a significant prevalence of myopia in children and adolescents in a specific population in the west of Paraná. The association between the year of diagnosis, with a notable increase in 2020, suggests the influence of environmental factors, possibly related to the lockdown imposed during the SARSCOV-2 pandemic. In addition, the study found that females were more likely to develop myopia than males. Comparing age groups, adolescents had a higher prevalence of the disease. The identification of risk factors, such as female sex, adolescence, and the year of diagnosis, highlights the need for preventive approaches and early intervention strategies aimed at this population. There is an urgent need for initiatives that promote outdoor activities and preventive actions, especially during times of crisis, to reduce the prevalence of myopia and protect the future eye health of these populations.
ACKNOWLEDGMENTS
The authors express their gratitude to the institutional support of HOlhos Prime Ophthalmological Hospital for providing the necessary infrastructure for conducting this research.
REFERENCES
1. Alves MR, Polati M, Souza SJF. Refratometria Ocular e a Arte da Prescrição Médica. 7th ed. Guanabara Koogan; 2023.
2. Haarman AEG, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJM, Klaver CCW. The complications of myopia: A review and meta-analysis. Invest Opthalmol Vis Sci. 2020;61(4):49.
3. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42.
4. Yotsukura E, Torii H, Ozawa H, Hida RY, Shiraishi T, Corso Teixeira I, et al. Axial length and prevalence of myopia among schoolchildren in the equatorial region of Brazil. J Clin Med. 2020;10(1):115.
5. Pärssinen O, Kauppinen M. Risk factors for high myopia: a 22-year follow-up study from childhood to adulthood. Acta Ophthalmol. 2019;97(5):510-518.
6. Grzybowski A, Kanclerz P, Tsubota K, Lanca C, Saw SM. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 2020;20(1):27.
7. Aaraj S, Kausar A, Khan SA. Vitamin D deficiency: a risk factor for myopia in children: a cross sectional study in a tertiary care centre. J Pak Med Assoc. 2022;72(6):1075-1079.
8. Dragomirova M, Antonova A, Stoykova S, Mihova G, Grigorova D. Myopia in Bulgarian school children: prevalence, risk factors, and health care coverage. BMC Ophthalmol. 2022;22(1):248.
9. Matsumura S, Dannoue K, Kawakami M, Uemura K, Kameyama A, Takei A, et al. Prevalence of myopia and its associated factors among Japanese preschool children. Front Public Health. 2022 Jun 22;10:901480.
10. R Core Team. R: A language and environment for statistical computing [Internet]. R Foundation for Statistical Computing, Vienna, Austria. 2021 [cited 2023 Jul 13]. Available from: https://www.r-project.org/
11. Wickham H, Averick M, Bryan J, Chang W, McGowan L, François R, et al. Welcome to the Tidyverse. J Open Source Softw. 2019;4(43):1686.
12. Wickham H, François R, Henry L, Müller K, Vaughan D. dplyr: A Grammar of Data Manipulation. R package version 1.1.2 [Internet]. 2023 [cited 2023 Dec 19]. Available from: https://CRAN.R-project.org/package=dplyr
13. Mori K. striprtf: Extract Text from RTF File_. R package version 0.6.0 [Internet]. 2023 [cited 2023 Dec 19]. Available from: https://CRAN.R-project.org/package=striprtf
14. Escolar C, Educacional R. Pesquisa " Resposta Educacional à Pandemia de COVID-19 no Brasil " BRASIL Resumo O presente trabalho é uma reorganização dos dados gerais da pesquisa realizada pelo INEP agregada à coleta de dados do Censo Escolar da Educação Básica de 2020 , intitulada ". 2020;1-42.
15. Guo L, Yang J, Mai J, Du X, Guo Y, Li P, et al. Prevalence and associated factors of myopia among primary and middle school-aged students: a school-based study in Guangzhou. Eye (Lond). 2016;30(6):796-804.
16. French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren. Ophthalmology. 2013;120(10):2100-2108.
17. Stefano S, Lima LCF. A gênese da miopia à luz (solar) de novas evidências: redução do tempo gasto ao ar livre diretamente associado ao aumento da miopia. Acta MSM. 2022;9(4):115.
18. Lee SSY, Mackey DA. Prevalence and risk factors of myopia in young adults: Review of findings from the Raine study. Front Public Health. 2022 Apr 27;10:861044.
19. Cao K, Wan Y, Yusufu M, Wang N. Significance of outdoor time for myopia prevention: A systematic review and meta-analysis based on randomized controlled trials. Ophthalmic Res. 2020;63(2):97-105.
20. Mutti DO, Mulvihill SP, Orr DJ, Shorter PD, Hartwick ATE. The effect of refractive error on melanopsin-driven pupillary responses. Invest Opthalmol Vis Sci. 2020;61(12):22.
21. Enthoven CA, Tideman JWL, Polling JR, Yang-Huang J, Raat H, Klaver CCW. The impact of computer use on myopia development in childhood: The Generation R study. Prev Med. 2020 Mar;132:105988.
22. Guan H, Yu NN, Wang H, Boswell M, Shi Y, Rozelle S, et al. Impact of various types of near work and time spent outdoors at different times of day on visual acuity and refractive error among Chinese school-going children. PLoS One. 2019;14(4):e0215827.
23. Cunha RNP. Miopia na Infância. Arq Bras Oftalmol. 2000;63(3): 231-234.
24. Vitale S, Cotch MF, Sperduto R, Ellwein L. Costs of refractive correction of distance vision impairment in the United States, 1999-2002. Ophthalmology. 2006;113(12):2163-2170.
25. Rein DB, Zhang P, Wirth KE, Lee PP, Hoerger TJ, McCall N, et al. The economic burden of major adult visual disorders in the United States. Arch Ophthalmol. 2006;124(12):1754-60.
AUTHORS INFORMATIONS |
|
 |
» Arnonn Afonso Agassi Martelli https://orcid.org/0009-0007-3805-1291 https://lattes.cnpq.br/6620247004020126 |
 |
» Daniel Traumann https://orcid.org/0009-0005-8354-4621 https://lattes.cnpq.br/1555903851390196 |
 |
» Clodomir Salgueiro Cordeiro de Carvalho https://orcid.org/0009-0001-8140-6808 https://lattes.cnpq.br/4022756359303070 |
 |
» Camila Marinelli Martins https://orcid.org/0000-0002-6430-2687 https://lattes.cnpq.br/7794236796565015 |
 |
» Licia Deon Weirich https://orcid.org/0009-0005-1289-822X https://lattes.cnpq.br/6242614437743193 |
 |
» Cassio Tokuji Tsujiguchi https://orcid.org/0009-0004-0925-5269 https://lattes.cnpq.br/4482485020935477 |
 |
» Marcos Solano Vale https://orcid.org/0009-0007-1677-9003 https://lattes.cnpq.br/3530712950826131 |
Funding: Hospital Oftalmologico HOlhos Prime, Cascavel, PR, Brazil.
Project number and institution responsible for the opinion of the Research Ethics Committee: CAAE: 73696323.6.0000.0105/State University of Ponta Grossa-UEPG
Conflicts of interest: The authors declare that there are no conflicts of interest to declare
Received on:
January 19, 2024.
Accepted on:
June 14, 2024.