Leonardo E. Ariello; Mário L. R. Monteiro
DOI: 10.17545/eOftalmo/2024.0002
Este artigo pertence à Edição Especial Edição especial Neuro
Optic neuritis (ON) is an acute inflammatory disease of the optic nerve. ON can occur in isolation or in association with other demyelinating diseases of the central nervous system (CNS), such as neuromyelitis optica (NMO), myelin oligodendrocyte glycoprotein antibody disease (MOGAD), and, more commonly, multiple sclerosis (MS). Currently, the diagnosis of ON involves assessing clinical data and conducting complementary examinations, including magnetic resonance imaging (MRI)1. Herein, we describe the role and importance of MRI in diagnosing ON and differentiating it from other demyelinating CNS diseases.
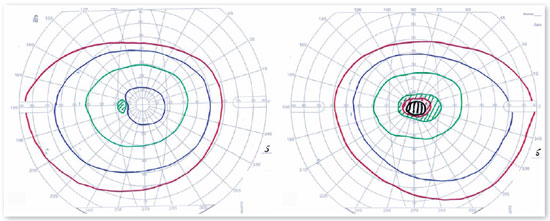
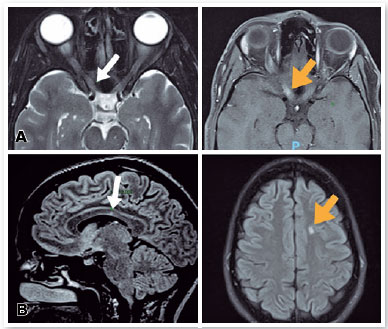
ON typically affects young adult women. Visual acuity loss is usually pronounced and progressive over days, with the nadir between 20/40 and counting fingers. Periocular pain that worsens with eye movement and precedes vision loss is reported in 90% of cases. Pupils are isochoric, but the affected eye exhibits an afferent defect. The fundus of the eye may show papillary edema; however, this symptom can also occur in retrobulbar neuritis. Perimetry typically reveals a central or cecocentral scotoma, as shown in Figure 1, in which a patient with ON exhibited a visual acuity of counting fingers in the right eye. Serological tests usually yield normal results, while cerebrospinal fluid analysis may indicate a slight increase in cellularity and the presence of oligoclonal bands in patients with MS. Orbital MRI typically reveals hyperintensity on T2 sequence in the orbital and prechiasmal portions of the optic nerve with contrast enhancement (Figure 2A, right). Brain MRI aids in identifying T2 hyperintense lesions in juxtacortical areas, with hyperintense foci at the callosal–septal junction (Figure 2B). In the example shown in Figure 2, ON was diagnosed in the right eye and signs of multifocal demyelinating disease were observed. A 5-day course of high-dose intravenous methylprednisolone pulse therapy (1 g/day) resulted in significant improvement, elevating the visual acuity of the right eye to 20/25.
Currently, the diagnosis of ON involves the evaluation of clinical and complementary examination data2. Among these examinations, MRI plays a central role. This imaging modality exhibits 95% sensitivity in detecting inflammatory processes in the optic nerve3. Furthermore, a comprehensive assessment of the distribution, extent, and appearance of inflammatory processes in the optic nerve and orbit contributes to the differential diagnosis of ON.
Bilateral involvement of the optic nerves is more common in NMO and MOGAD than in MS. Lesions affecting the optic chiasm and tract are more commonly observed in NMO. Longitudinally extensive neuritis, involving >50% of the optic nerve, is more frequently observed in NMO and MOGAD. Perineural involvement of the optic nerve, also known as perineuritis, is more commonly observed in MOGAD4,5.
In conclusion, advances in imaging techniques, particularly MRI, have become essential for evaluating ON. The high sensitivity of this modality not only facilitates the diagnosis of ON but also enables effective differentiation from other demyelinating diseases resulting in better prognosis and treatment.
REFERENCES
1. Bennett JL. Optic Neuritis. Continuum (Minneap Minn). 2019; 25(5):1236-1264.
2. Petzold A, Fraser CL, Abegg M, Alroughani R, Alroughani D, Alvarenga R, et al. Diagnosis and classification of optic neuritis. Lancet Neurol. 2022;21(12):1120-1134.
3. Kupersmith MJ, Alban T, Zeiffer B, Lefton D. Contrast-enhanced MRI in acute optic neuritis: relationship to visual performance. Brain. 2002 Apr;125(Pt 4):812-822.
4. Ramanathan S, Prelog K, Barnes EH, Tantsis EM, Reddel SW, Henderson APD, et al. Radiological differentiation of optic neuritis with myelin oligodendrocyte glycoprotein antibodies, aquaporin-4 antibodies, and multiple sclerosis. Mult Scler. 2016;22(4):470-482.
5. Akaishi T, Sato DK, Nakashima I, Takeshita T, Takahashi T, Doi H, et al. MRI and retinal abnormalities in isolated optic neuritis with myelin oligodendrocyte glycoprotein and aquaporin-4 antibodies: a comparative study. J Neurol Neurosurg Psychiatry. 2016;87(4):446-448.
AUTHORS INFORMATIONS |
|
 |
» Mario Luiz Ribeiro Monteiro https://orcid.org/0000-0002-7281-2791 http://lattes.cnpq.br/283589747518026 |
 |
» Leonardo Eleuterio Ariello https://orcid.org/0000-0002-7031-2419 http://lattes.cnpq.br/1417602536827866 |
Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
October 17, 2023.
Accepted on:
October 30, 2023.