Pedro Henrique Ogata Kodama; João Victor Mendes de Oliveira; Gabriela Mousse de Carvalho; Rodrigo Jorge
DOI: 10.17545/eOftalmo/2023.0050
ABSTRACT
Combined hamartoma of the retina and retinal pigment epithelium is a rare, benign, congenital tumor. In addition to the retina and retinal pigment epithelium, it affects the glial tissue and retinal vessels. This tumor is usually unilateral and is commonly diagnosed in young children with strabismus and low visual acuity. The lesion can be confused with malignant tumors such as choroidal melanoma and retinoblastoma. This case report presents the follow-up of a 10-year-old girl with combined hamartoma of the retina and retinal pigment epithelium in the right eye.
Keywords: Retina; Retinal pigment epithelium; Retinal neoplasms; Hamartoma; Tomography optical coherence.
RESUMO
O hamartoma combinado de retina e epitélio pigmentar da retina é um tumor congênito raro e benigno. É uma mistura de retina, epitélio pigmentar da retina, tecido glial e vasos retinianos. É geralmente unilateral e é comumente diagnosticado em crianças pequenas associado a estrabismo e baixa acuidade visual. A lesão tumoral pode ser confundida com tumores malignos, como melanoma de coroide e retinoblastoma. Este relato tem o objetivo de apresentar o acompanhamento de uma paciente de 10 anos com hamartoma combinado de retina e epitélio pigmentar da retina no olho direito.
Palavras-chave: Retina; Epitélio pigmentado da retina; Neoplasias da retina; Hamartoma; Tomografia de coerência óptica.
INTRODUCTION
The term combined hamartoma of the retina and retinal pigment epithelium (CHR-RPE) was coined by Gass in 1973. The lesion was described as pigmented, raised with vascular tortuosity and retinal and RPE malformations. CHR-RPE was also divided into two subcategories depending on optic nerve involvement. These subcategories had a crucial histopathological difference. The combined hamartoma involving the optic nerve exhibited hypertrophy of the RPE, the presence of peripheral retinal capillaries, and greater retinal disorganization1. CHR-RPE is considered a congenital, benign, rare tumor affecting the retina, RPE, glial tissue, and retinal vessels2,3. The tumor is usually asymptomatic and unilateral and is common in young children with strabismus and low visual acuity (VA). Diagnosis of CHR-RPE is important, as this lesion can be clinically confused with malignant tumors such as retinoblastoma and choroidal melanoma1,4,5. Optical coherence tomography (OCT) and fluorescein angiography can aid in the clinical diagnosis of CHR-RPE.
CASE REPORT
A healthy 10-year-old girl was referred for the first ophthalmological assessment in 2020 as she complained of exotropia in the right eye (RE), noticed by the mother 4 months ago.
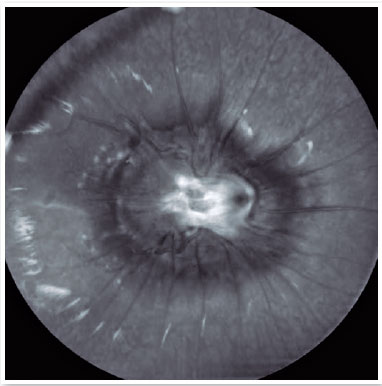
During the ophthalmological evaluation, in addition to ocular deviation, the girl presented VA OD of hand movement and 1.0 in the left eye (LE). No changes in intraocular pressure or biomicroscopy were noticed in both eyes. Fundoscopy revealed a grayish, elevated lesion with vascular tortuosity and covered by glial tissue in the RE. The lesion extended to the macula and affected the optic nerve (Figures 1 and 2).

OCT revealed a hyper-reflective lesion in the inner retina that affected the retinal full thickness (Figure 3). It presented morphological disorganization involving all retinal layers, including the inner nuclear layer, outer plexiform, ellipsoid zone, retinal pigment epithelium (RPE), and Bruch's membrane.
Fluorescein angiography displayed, in the early phase, a hypofluorescence area in the hyperpigmentation region and, in the late phase, vascular filling-induced extravasation with signs of neovascularization (Figure 4). Both examinations helped in CHR-RPE diagnosis.
The patient is being followed up with regular retinal examinations, and during 2 years of follow-up, the lesion remained stable without any complications.
DISCUSSION
CHR-RPE is a congenital, benign, rare tumor and is usually diagnosed in children with leukocoria, low VA, or strabismus1-3. This tumor involves retinal layers, retinal vessels, and glial tissue. This lesion has malignant tumors, such as choroidal melanoma and retinoblastoma, as differential diagnoses.
CHR-RPE can be found alone or associated with some systemic conditions, such as, mainly, neurofibromatosis type II6. However, some studies have reported the associations between CHR-RPE and neurofibromatosis type I, brachio-oculofacial syndrome, and Gorlin-Goltz syndrome7.
Painless low VA is the main symptom of this tumor and is apparently related to its location2. Tumors involving the optic nerve, papillomacular bundle, or fovea tend to have worse VA. Other causes leading to visual loss are epiretinal membrane (ERM) formation and subsequent traction, in addition to retinal folds, macular holes, intraretinal exudation, subretinal fluid, and choroidal neovascularization8.
Complementary examinations aid in the clinical diagnosis of CHR-RPE. On OCT, the tumor appears as a hyper-reflective mass, with increased thickness and posterior shading, associated with retinal folds and disorganization of all retinal layers8-10. Another finding is the "shark tooth" sign, which refers to small hyper-reflective triangles in the outer retina located at the hamartoma edge10. Fluorescein angiography can possibly present vascular tortuosity in addition to a central hypofluorescence area associated with extravasation of contrast11.
CHR-RPE management involves ophthalmological follow-up with complementary examinations, treatment of amblyopia in children, and specific treatment in cases of complications, such as tractional retinal detachment, ERM, choroidal neovascularization, and vitreous hemorrhage3.
The patient is being followed up by the ocular oncology department with an ophthalmological evaluation and complementary examinations every 6 months. In the 2 years of follow-up, the patient has maintained VA and the lesion has remained stable, with no complications. This case report indicates the importance of follow-up in a specialized service as well as the correct diagnosis of CHR-RPE in the presence of other differentials with malignant tumors, which prevents misdiagnosis.
REFERENCES
1. Gass JD. An unusual hamartoma of the pigment epithelium and retina simulating choroidal melanoma and retinoblastoma. Trans Am Ophthalmol Soc. 1973;71:171-183; discussions 184-5.
2. Schachat AP, Shields JA, Fine SL, Sanborn GE, Weingeist TA, Valenzuela, RE, et al. Combined hamartomas of the retina and retinal pigment epithelium. Ophthalmology. 1984;91(12):1609-15.
3. Bowling B, Kanski JJ. Kanski's clinical ophthalmology: a systematic approach. 8. ed. Edinburgh: Elsevier, 2016.
4. Machemer R. [PRIMARY RETINAL PIGMENT EPITHELIAL HYPERPLASIA]. Albrecht Von Graefes Arch Ophthalmol. 1964 Jul 20;167:284-95.German.
5. Vogel MH, Zimmerman LE, Gass JD. Proliferation of the juxtapapillary retinal pigment epithelium simulating malignant melanoma. Doc Ophthalmol. 1969;26:461-81.
6. Landau K. The Role of Neuro-Ophthalmologists in the Care of Patients With Neurofibromatosis Type 2. J Neuroophthalmol. 2020 Sep;40 Suppl 1:S51-S56.
7. Shields CL, Thangappan A, Hartzell K, Valente P, Pirondini C, Shields JA. Combined hamartoma of the retina and retinal pigment epithelium in 77 consecutive patients visual outcome based on macular versus extramacular tumor location. Ophthalmology. 2008;115(12):2246-2252.e3.
8. Arepalli S, Pellegrini M, Ferenczy SR, Shields CL. Combined hamartoma of the retina and retinal pigment epithelium: findings on enhanced depth imaging optical coherence tomography in eight eyes. Retina. 2014;34(11):2202-7.
9. Shields CL, Mashayekhi A, Dai VV, Materin MA, Shields JA. Optical coherence tomographic findings of combined hamartoma of the retina and retinal pigment epithelium in 11 patients. Arch Ophthalmol. 2005;123(12):1746-50.
10. Arrigo A, Corbelli E, Aragona E, Manitto MP, Martina E, Bandello F, et al. Optical coherence tomography and optical coherence tomography angiography evaluation of combined hamartoma of the retina and retinal pigment epithelium. Retina. 2019;39(5):1009-1015.
11. Scupola A, Grimaldi G, Sammarco MG, Sasso P, Marullo M, Blasi MA. Multimodal imaging evaluation of combined hamartoma of the retina and retinal pigment epithelium. Eur J Ophthalmol. 2020;30(3):595-599.
| AUTHORS INFORMATION |
|
 |
» Pedro Henrique Ogata Kodama https://orcid.org/0000-0001-6718-6864 http://lattes.cnpq.br/9122925352054805 |
 |
» João Victor Mendes de Oliveira https://orcid.org/0000-0002-9433-9819 http://lattes.cnpq.br/3922079295284178 |
 |
» Gabriela Mousse de Carvalho https://orcid.org/0009-0003-8289-7690 http://lattes.cnpq.br/872629445484118 |
 |
» Rodrigo Jorge https://orcid.org/0000-0002-2652-0720 http://lattes.cnpq.br/4045374522226547 |
Funding: No specific financial support was available for this study.
Approved by the following research ethics committee: Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto (CAAE: 71521623.9.0000.5440).
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
October 3, 2023.
Accepted on:
October 22, 2023.