Celso Marcelo Cunha1; Gilmar Jorge de Oliveira Júnior2; Giovanna Marchezine3; Miguel José Calix Netto4; Jessica Teixeira Cunha3; Julia Schmidt Dal Berto4; Matheus Bitencourt Novaes3
DOI: 10.17545/eOftalmo/2022.0020
ABSTRACT
PURPOSE: It was proposed in this study to develop a new formula based on corneal keratometry and axial length of ocular globe to estimate the objective refraction or estimated spherical power.
METHODS: Retrospective and cross-sectional study in which were selected medical records from 150 myopic patients, consecutive, attended at the Oftalmocenter Santa Rosa, Cuiabá, MT, between 2017 and 2019. Collected from these records were the age, sex, visual acuity, cycloplegic refraction, and the results from corneal topography and optic biometric. It was applied the multiple linear regression test to determine the possible models for the development of proposed formula.
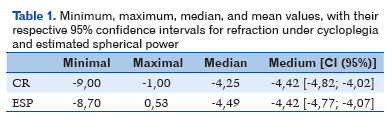
RESULTS: Among the 150 medical records, 100 right eyes had all criteria and were included in this study. The mean age of population studied was 17 ± 6.2 years, of which 49 were males. The average and the SD of myopia, astigmatism, K1, K2 and axial length were -4.42 ± 2.06 D, 0.57 ± 0.86 D; 44.14 ± 1.09 D, 44.97 ± 1.38 D, e 25.00 ± 1.19 mm, respectively. The formula was: estimated spherical power = 63.7584 – 1.6647 x axial length - 0.6018 x K1. The coefficient of adjusted determination between the objective refraction with cycloplegia and estimated spherical power was 0.75.
CONCLUSION: The formula demonstrated to possess high level of agreement with refraction in this population. The formula may be studied in subjective refraction in patients with irregular astigmatism and this hypothesis must be confirmed in subsequent studies in the population with keratoconus.
Keywords: Ocular refraction; Astigmatism; Visual acuity; Keratoconus; Keratometry.
RESUMO
OBJETIVO: Propôs-se desenvolver uma fórmula baseada na ceratometria corneana e diâmetro anteroposterior do globo ocular para estimar a refração esférica objetiva, ou poder esférico estimado.
MÉTODOS: Estudo retrospectivo, transversal e observacional, selecionou prontuários de 150 pacientes míopes, consecutivos, atendidos no Oftalmocenter Santa Rosa – Cuiabá – MT, entre o período de 2017 a 2019. Coletou-se dados da idade, sexo, acuidade visual, refração com cicloplegia, e resultados da ceratometria e diâmetro anteroposterior. Utilizou-se a regressão linear múltipla para determinar os possíveis modelos.
RESULTADOS: Dos 150 prontuários, 100 olhos direitos continham todos os critérios de inclusão. A idade média foi de 17 ± 6,2 anos, sendo 49 do sexo masculino. A média e o DP da miopia, astigmatismo, K1, K2 e diâmetro anteroposterior foram de -4,42 ± 2,06 D, 0,57 ± 0,86 DC, 44,14 ± 1,09, 44,9 7 ±1,38 D, e 25,00 ± 1,19 mm, respectivamente. A fórmula deduzida foi: poder esférico estimado = 63,7584 - 1,6647 x diâmetro anteroposterior - 0,6018 x K1. O coeficiente de determinação ajustado entre a refração objetiva e a poder esférico estimado foi de 0,75.
CONCLUSÃO: A fórmula apontou alto índice de concordância com a refração dessa população. A fórmula deduzida deverá ser estudada na refração subjetiva dos pacientes com astigmatismo irregular, devendo-se sua eficácia ser comprovada em estudos subsequentes nesta população.
Palavras-chave: Refração ocular; Astigmatismo; Acuidade visual; Ceratocone; Ceratometria.
INTRODUCTION
Finding the best refraction in irregular astigmatism (IA) is one of the greatest challenges in refractometry. Keratoconus is a bilateral, progressive, noninflammatory corneal disease and the most frequent cause of IA(1). IA can lead to extreme technical difficulty in objective refraction owing to the classic scissor reflexes in retinoscopy and to the poor reproducibility of the results of autorefractors, which has resulted in subjective refraction in long-term cases(2). The use of the Gasset rule was proposed decades ago, considering only the minimum and maximum keratometry values (K1 and K2) to suggest the initial subjective spherical and cylindrical refraction(3).
In determining ocular spherical power, the following three factors are important: the anterior corneal curvature, the lens power, and the axial length of the eyeball (AL)(4). In patients with keratoconus, the natural tendency to find myopic spherical refraction is primarily attributable to an increased corneal curvature(2).
In this perspective, the present study aimed to retrospectively analyze medical records of patients with myopia, in order to obtain data and develop a new formula for estimating spherical power that takes the keratometry values and AL into consideration.
METHODS
This cross-sectional, retrospective, observational study selected 150 medical records of patients from Oftalmocenter Santa Rosa, an ophthalmological clinic in Cuiabá, Brazil. The patients selected were all diagnosed with myopia and underwent the eye exams related to this study sequentially between January 2017 and December 2019.
Patients of both sexes were included, with static refraction between −9.00 and −1.00 spherical diopters (D), and topographically regular corneas according to the criteria standardized in 1994 by Maeda and Klyce(5). Patients both with and without astigmatism were included; however, when this condition was present, it should be between 0.25 and 3.00 cylindrical diopters (D). Patients younger than 10 years or older than 35 years, those with incomplete data, with eye anomalies, who had previous eye surgery, those with any mental deficit or genetic syndromes, or who did not cooperate in the examinations were excluded.
Age, sex, visual acuity, cycloplegic refraction (CR), minimum and maximum topographic keratometry values (K1 and K2), and AL (right eye only) were collected for the records that met all the inclusion criteria and did not meet any of the exclusion criteria.
Statistical analyses were performed using SPSS statistical software, version 22.0 (IBM Corporation, Armonk, New York, USA) and Excel 2016 (part of Office 2016; Microsoft Corporation, Redmond, Washington, USA). The data were described through graphs, tables, and descriptive statistics.
To develop the proposed formula, multiple linear regression was used to determine the possible models(6), with the joint significance of the explanatory variables being verified by the F test, and the individual significance for each variable of the model by the t test. Subsequently, after determining the models, the assumptions were verified using the Kolmogorov-Smirnov (normality), Breusch-Pagan (homogeneity), and Durbin-Watson (independence) tests, all using a significance level of 5%.
After developing the formula (obtained through a regression model), the myopic values found in the CR were compared with the values estimated by the proposed formula.
This study was approved by the Ethics and Research Committee of Centro Universitário de Várzea Grande (UNIVAG), Várzea Grande, State of Mato Grosso, Brazil, under the Certificate of Presentation for Ethical Appraisal (CAAE) No. 40989720.2.0000.5692, meeting all the ethical requirements set forth by Resolution No. 466/2012 of the Brazilian National Health Council.
RESULTS
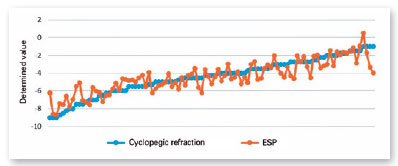
One hundred medical records met the selection criteria. The mean age of the population studied was 17 ± 6.2 years, ranging from 10 to 35 years, and with 49 (49%) males. The mean and standard deviation of myopia were −4.42 ± 2.06 D, ranging from −1 to −9 D; for astigmatism, 0.57 ± 0.86 D, ranging from 0 to 3.25 CD. K1 had a mean ± SD of 44.14 ± 1.09 D (range, 43-47.7 D), and K2 had 44.97 ± 1.38 D (range, 43-48.9 D). Finally, the mean ± SD for AL were 25.00 ± 1.19 mm (range, 22.26-27.92 mm).
The deduced formula for the best approximation of RUC for the estimated spherical power (ESP) was:
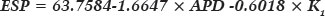
where an adjusted coefficient of determination was obtained (adjusted R2 = 0.7543).
The values determined for CR and those estimated for all participants using the ESP formula are shown in Figure 1, and their descriptive statistics are shown in Table 1.
DISCUSSION
One of the origins of the classic phrase of the great masters of refractometry, “ocular refraction is an art,” is refraction in irregular astigmatisms. Some patients with keratoconus have high myopic and astigmatic powers and cannot tolerate the prolonged use of contact lenses; thus, glasses are an essential alternative during part of the day to allow these patients to perform daily activities(7). K1 and AL values have been used as means to quickly estimate a spherical power to initiate subjective refraction in these cases. These values can be obtained by corneal keratometry and low-cost ultrasonic biometry, and they could help in difficult cases of refraction. The initial values of astigmatism that may exist in cases of IA should be addressed according to the appropriate literature.
In recent decades, studies have emerged demonstrating good results with the use of wavefront devices to provide objective refraction in these cases; however, these studies were not randomized or double-blind, and the high cost of this technology prevents its use in routine approaches in ophthalmological offices in Brazil(8,9).
Several studies have correlated biometric data with ocular refraction. Corneal curvature has a low correlation with this measurement. The greatest correlation is typically identified between AL and ocular refraction(10,11). Therefore, it can be expected that the Gasset formula, previously proposed for estimating the spherical power in IAs, is not very reproducible for this purpose. Another study used AL in the past to estimate the ESP; in one study, a formula was developed for a population aged 0.5-33 years with congenital glaucoma, but with a mean of 11.06 years, which indicates a large number of patients younger than 10 years. In this age group, the lens has greater power, which leads to greater myopic powers, in addition to eyes with a high AL due to the characteristic buphthalmos(12). The diagnosis of keratoconus is usually at an older mean age than in the present study. The age of the population selected for this study sought to represent the age group related to the diagnosis of keratoconus. Therefore, the population aged under 10 years may have undercorrected ESP values.
Lens power is another important biometric measurement that could help to refine the formula; however, its measurement is performed with greater precision by optical biometry, which allows the lens power to be estimated using the Bennett formula (or the formula adapted by Rozema(13,14)), provided data on the depth of the anterior chamber, lens thickness, corneal keratometry, AL, and refraction are known. Owing to the fact that the present study did not propose to determine the ocular refraction beforehand, performing this calculation was unfeasible.
The formula obtained in this study helps to find the best initial objective refraction in patients with mild ocular medium opacities that do not allow correct retinoscopy, and for whom the autorefractor does not provide reliable results.
This study has some limitations, such as not having used the formula in irregular corneas (this will be Phase Two of this study) and not having selected only corneal curvatures of >46 D, which are commonly found in the population with keratoconus.
With this new formula, a high rate of agreement with CR was found in this population. The use of the formula obtained may simplify the initiation of subjective refraction in patients with mild ocular medium opacities. In the future, it may also be possible to reduce the subjective refraction time in patients with highly irregular astigmatism. New randomized and blinded studies in the population with keratoconus may confirm these claims.
REFERENCES
1. Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293-322.
2. Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol. 1986;101(3):267-73.
3. Gasset AR. Simplified refracting technique in keratoconus. Ann Ophthalmol. 1975;7(1):117-21.
4. Holzchuh N. Córnea. In: Schor P, Uras R, Veitzman S. Ótica, refração e visão subnormal. Rio de Janeiro: Cultura Médica; Guanabara Koogan, 2008. p. 115-8.
5. Maeda N, Klyce SD, Smolek MK, Thompson HW. Automated keratoconus screening with corneal topography analysis. Invest Ophthalmol Vis Sci. 1994;35(6):2749-57.
6. Draper NR, Smith H. Applied regression analysis. 3 ed. Wiley-Interscience, 1998.
7. Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT, et al. Baseline Findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci. 1998;39(13):2537-46.
8. Ambrósio R Jr, Caldas DL, Silva RS, Pimentel LN, Valbon BF. Impacto da análise do ‘wavefront’ na refratometria de pacientes com ceratocone. Rev Bras Oftalmol. 2011;70(1):16-22.
9. Jinabhai A, O´donnell C, Radhakrishnan H. A Comparison between Subjective Refraction and Aberrometry-Derived Refraction in Keratoconus Patients and Control Subjects. Curr Eye Res. 2010; 35(8):703-14.
10. Jones Ll, Mitchell GL, Mutti DO, Hayes JR, Moeschberger ML, Zadnik K. Comparison of Ocular Component Growth Curves among Refractive Error Groups in Children. Invest Ophthalmol Vis Sci. 2005;46(7):2317-27.
11. Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44(4):1492-1500.
12. Carani JCE, Betinjane AJ, Carvalho CA. Método (fórmula) para avaliação da refração ocular no glaucoma congênito. Arq Bras Oftalmol. 1994;57(2):137-40.
13. Bennett AG. A method of determining the equivalent powers of the eye and its crystalline lens without resort to phakometry. Ophthalmic Physiol Opt. 1988;8(1):53-9.
14. Rozema JJ, Atchison DA, Tassignon MJ. Comparing Methods to Estimate the Human Lens Power. Investig Ophthalmol Vis Sci. 2011;52(11):7937-42.
AUTHOR’S INFORMATION




Funding: No specific financial support was available for this study
Approved by the following research ethics committee: Centro universitário da Várzea Grande – UNIVAG (CAAE: 40989720.2.0000.5692).
Conflict of interest: None of the authors have any potential conflict of interest to disclose
Received on:
August 7, 2022.
Accepted on:
October 12, 2022.