Matheus Schwengber Gasparini; João Jorge Nassaralla Neto; Vicente Hidalgo Rodrigues Fernandes; Arthur Pinheiro Favarato; Luísa Grave Gross; Jessica Blanc Leite Oliveira; Andréa Mara Simões Torigoe
DOI: 10.17545/eOftalmo/2022.0004
ABSTRACT
Acute retinal artery occlusion is a classic cause of sudden monocular painless reduction of visual acuity. It is a type of stroke, sharing risk factors and etiologic mechanisms with acute cerebral ischemia. The ophthalmologist has an essential role in the diagnosis of this entity, through physical exams and complementary propaedeutics. In this article, we report a case of branch retinal artery occlusion affecting the inferior half of retina in the right eye of a 79-year-old woman without known comorbidities. Current treatments of acute ischemia still have low effectiveness. However, fast and accurate diagnosis enables the establishment of secondary prevention methods in order to avoid new potentially fatal ischemic and cardiovascular events.
Keywords: Retinal artery; Retinal artery occlusion; Stroke; Ophthalmology; Neurology.
RESUMO
A oclusão arterial retiniana aguda é uma causa clássica de redução monocular súbita e indolor da acuidade visual. É um tipo de acidente vascular encefálico que tem fatores de risco e mecanismos etiológicos em comum com a isquemia cerebral aguda. O oftalmologista tem um papel essencial no diagnóstico desta patologia, através de exames físicos e propedêutica complementar. Neste artigo, relatamos um caso de oclusão de um ramo da artéria retiniana afetando a hemirretina no olho direito de uma mulher de 79 anos sem comorbidades conhecidas. Os tratamentos atuais da isquemia aguda ainda apresentam baixa eficácia. No entanto, o diagnóstico rápido e preciso permite o estabelecimento de métodos de prevenção secundária, a fim de evitar novos eventos isquêmicos e cardiovasculares potencialmente fatais.
Palavras-chave: Artéria retiniana; Oclusão da artéria retiniana; Acidente vascular cerebral; Oftalmologia; Neurologia.
INTRODUCTION
Acute retinal artery occlusion is a type of stroke. This definition is relatively unknown by clinicians and ophthalmologists. Therefore, it is important that this association is disclosed, so that appropriate preventive measures are taken. In this article, we report a case of branch retinal artery occlusion affecting the inferior half of retina in the right eye of a 79-year-old woman without known comorbidities. Moreover, there is a discussion based on the literature on the topic.
CASE REPORT
A 79-year-old woman arrived at the ophthalmology emergency service reporting a sudden onset of a black spot in the upper visual hemi campus of the right eye four days previous to the visit. She denied pain, ocular hyperemia, floaters or photopsia, as well as any symptoms in the contralateral eye. She reported, simultaneously with visual manifestations, onset of dizziness and malaise, with spontaneous resolution after a few minutes, and denied dysarthria, aphasia, paresis, hypoesthesia, headache, syncope or reduced level of consciousness. She reported slight improvement of the visual symptoms, but persistence of scotoma.
Regarding previous pathological history, she denied systemic comorbidities, allergy, acute myocardial infarction or stroke. She did not use any medication continuously. She underwent a hysterectomy procedure 28 years ago due to uterine leiomyomatosis, as well as phacoemulsification with intraocular lens implantation in both eyes, one year ago.
Through ophthalmological examination, she presented corrected visual acuity of 0.5 in the right eye and 0.6 in the left eye. Biomicroscopy showed a senile corneal arch, well-placed intraocular lenses and the absence of rubeosis iridis. Intraocular pressure, measured by Goldmann applanation tonometry, was normal in both eyes. Hirschberg test showed centered reflex. Examination also showed preserved extrinsic ocular mobility, symmetrical, isochoric and normally reactive pupils, as well as absence of nystagmus. After obtaining pharmacological mydriasis, a fundus biomicroscopy was performed, drawing attention to the presence of a retinal pallor area along the inferior temporal arch in the right eye. After the clinical examination, the main diagnostic hypothesis was branch retinal artery occlusion affecting the inferior half of retina in the right eye.
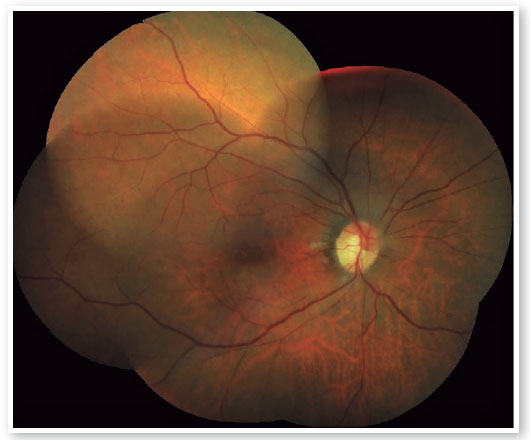
Retinography showed pallor of the inferior retina, embolus lodged in the first inferior branch of the central retinal artery and optic disc with pallor and mild edema in its inferior sector (Figure 1).

Optical coherence tomography (OCT) of the right eye was performed on the same day and demonstrated disorganization of the internal retinal layers in the inferior macular region and intraretinal edema in the region of the nerve fiber layer. Other findings consisted of foveal depression without changes and preserved sensorineural retina in the superior macular region.
Computerized perimetry showed a superior altitudinal defect in the right eye, an area corresponding to the inferior half of retina (Figure 2).
After the complementary ophthalmological tests, the patient was referred to the Emergency Room of the same hospital in order to undergo neurological evaluation. Upon physical examination, no other neurological changes were observed. Cranial angiotomography showed diffuse microangiopathy and moderate atheromatosis, with no evidence of acute injuries. The diagnosis, therefore, was ischemic stroke of probable atherothrombotic origin. The patient was discharged with a prescription for acetylsalicylic acid and simvastatin, monitoring of risk factors in a primary care unit and return for follow-up in the ophthalmology sector.
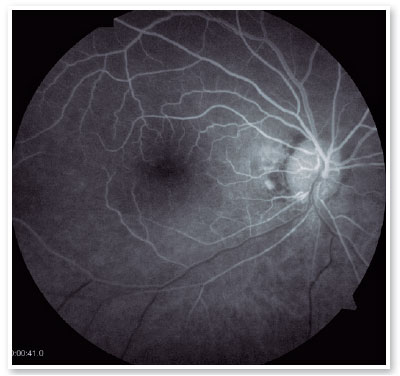
In subsequent consultations, the patient maintained the visual symptoms and did not present any new complaints. Retinographies of the subacute phase showed recovery of the retinal color, diffuse arterial narrowing in the inferior hemiretina and inferior optic disc pallor (Figure 3). OCT demonstrated atrophy of the corresponding inner retinal layers. Two months after the acute picture, fluorescein angiography was performed, with the following results: delayed filling of the central retinal inferior hemiartery, peripapillary hypofluorescence secondary to a blocking effect, late peripapillary hyperfluorescence due to window defect associated with peripapillary pigment atrophy (Figure 4).
After 3 months of follow-up, she was discharged from the ophthalmological sector, with recommendation of immediate return in case of new visual manifestations.
DISCUSSION
The central retinal artery originates from the ophthalmic artery, a branch of the internal carotid artery, and divides into four branches, which supply the inner layers of the retina. Occlusion of one or more vessels in this circulation leads to retinal ischemia. In turn, the ciliary arteries from the choriocapillaris circulation, in which the central retinal artery does not participate, irrigate the outer layers of the retina1.
Acute retinal arterial occlusion, an entity that includes central retinal artery occlusion (CRAO), branch retinal artery occlusion (BRAO) and ophthalmic artery occlusion (OAO), is a classic cause of sudden and painless monocular vision loss2. This condition characterizes a medical emergency, not just an ophthalmological one. The American Heart Association (AHA) and the American Stroke Association (ASA) consider acute retinal arterial occlusion to be a form of stroke, containing risk factors and etiological mechanisms similar to acute cerebral ischemia3.
The most common cause of retinal arterial occlusion is thromboembolic disease originating in the carotid artery, aortic arch or heart4. The source of the embolus, however, remains unknown in 60% of patients5. Giant cell arteritis, a systemic vasculitis, is a rare condition, but one that should always be considered in patients over 50 years of age in which retinal embolism is not observed4.
It is estimated that over 90% of patients with CRAO have cardiovascular risk factors, such as hypertension, diabetes mellitus, coronary artery disease, smoking, obesity and dyslipidemia6. Therefore, individuals with low cardiovascular risk should go under investigation for other conditions possibly associated, such as blood hypercoagulability, sickle cell anemia, illicit injectable drug, cocaine use and myeloproliferative disease7.
The classic clinical presentation of occlusion of the central retinal artery or one of its branches is the sudden onset of painless monocular vision loss. Objectively, visual acuity varies widely: it hardly changes in some patients, especially in those with BRAO. However, in case of macular involvement, it may decrease to “counting fingers” vision or less; in these cases, dyschromatopsia is usually present8. Impaired central vision also causes a relative afferent pupillary defect (RAPD) in the affected eye.
Characteristic fundoscopic findings include ischemic retinal edema - evidenced by a retinal pallor zone, “box carrying” of flow in retinal arterioles, arteriolar narrowing and unchanged optic disc9,10. In some cases, one can visualize the embolus lodged in the central retinal artery or in one of its branches. In addition, in cases of CRAO, a cherry-red spot at the macula is noted, which consists of a red fovea due to the underlying choroidal circulation, contrasting with diffuse retinal whitening. More proximal occlusions, affecting the ophthalmic artery, are characterized by the absence of this macular finding, since the choroidal circulation is also compromised, and by the presence of papillary edema.
It is noteworthy that the aforementioned fundoscopic findings may not be present in the first hours, making the diagnosis of acute retinal occlusion in the hyperacute phase challenging11. When in doubt, it is recommended to use complementary exams. Optical coherence tomography (OCT) shows edema of the inner layers of the retina in the acute phase, which become atrophic in the late phase12. Optical coherence tomography angiography (OCTA) and fluorescein angiography, in turn, analyze retinal perfusion11.
As for prognosis, CRAO and OAO are classically associated with severe reduction in visual acuity and loss of visual field. BRAO, in turn, tends to cause a less significant deficit, with the majority of patients maintaining visual acuity greater than or equal to 20/40, although there are also cases of “counting fingers” vision.
The final visual prognosis is variable and depends mainly on the duration of arterial occlusion. A study carried out in non-human primates demonstrated that CRAO for less than 100 minutes did not cause detectable retinal damage, while an ischemia greater than 240 minutes caused an irreversible deficit13,14. This suggests a short time to prevent permanent damage, similar to cerebral ischemia. Other prognostic factors include the type of embolus and, in the case of CRAO, the presence of a patent cilioretinal artery15.
A possible ophthalmological complication is the development of ocular neovascularization, which occurs after two weeks of the ischemic event and is significantly more common in CRAO than in BRAO. Consequently, there is a risk of neovascular glaucoma, vitreous hemorrhage and retinal detachment, with worsening visual loss16.
Acute retinal arterial occlusion is associated with an increased risk of acute coronary syndrome17,18. There was also a higher risk of preceding, concomitant or subsequent cerebral ischemia, especially in the first week after the retinal event18. Evidence of cerebral ischemia is frequent on diffusion sequence magnetic resonance imaging (MRI-DWI), even if the patient does not present clinical findings5.
These data support the statement that acute retinal arterial occlusion constitutes a medical emergency, whose early management prevents potentially fatal complications. Going against the grain of evidence, many doctors, including retina specialists, do not refer these patients to a detailed clinical evaluation at specialized emergency centers19.
Several therapeutic options have been evaluated, such as vasodilator medications, carbogen inhalation, intravenous administration of acetazolamide and mannitol, eye massage and anterior chamber paracentesis. However, none of these measures has proved beneficial to the point of altering the natural history of the disease. Thus, treatment of acute retinal arterial occlusion is mainly based on the control of risk factors and the prevention of subsequent ischemic events4.
There is optimism among specialists regarding future use of intravenous or intra-arterial thrombolytic drugs in the hyperacute phase, similarly to other forms of stroke. However, there is still no solid evidence to support a clear benefit from such practice, with recent studies showing conflicting data. Therefore, pharmacological thrombolysis remains restricted to a minority of selected cases20.
It is essential that every ophthalmologist knows how to readily recognize a case of acute retinal arterial occlusion. Furthermore, it is important to recognize this condition as a medical emergency in order to carry out the necessary neurological tests. Thus, measures to prevent subsequent ischemic events can be taken, decreasing the risk of new potentially fatal ischemic events.
REFERENCES
1. Kur J, Newman EA, Chan-Ling T. Cellular and physiological mechanisms underlying blood flow regulation in the retina and choroid in health and disease. Prog Retin Eye Res. 2012;31(6):377-406.
2. Dattilo M, Newman NJ, Biousse V. Acute retinal arterial ischemia. Ann Eye Sci. 2018 Jun;3:28.
3. Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJB, Culebras A, Elkind MSV, George MG, Hamdan AD, Higashida RT, Hoh BL, Janis LS, Kase CS, Kleindorfer DO, Lee JM, Moseley ME, Peterson ED, Turan TN, Valderrama AL, Vinters HV, American Heart Association Stroke Council, Council on Cardiovascular Surgery and Anesthesia, Council on Cardiovascular Radiology and Intervention, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Prevention, Council on Peripheral Vascular Disease, Council on Nutrition, Physical Activity and Metabolism. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44(7):2064-89.
4. Sharma RA, Dattilo M, Newman NJ, Biousse V. Treatment of Nonarteritic Acute Central Retinal Artery Occlusion. Asia Pac J Ophthalmol (Phila). 2018;7(4):235-41.
5. Lee J, Kim SW, Lee SC, Kwon OW, Kim YD, Byeon SH. Co-occurrence of acute retinal artery occlusion and acute ischemic stroke: diffusion-weighted magnetic resonance imaging study. Am J Ophthalmol. 2014;157(6):1231-8.
6. Callizo J, Feltgen N, Pantenburg S, Wolf A, Neubauer AS, Jurklies B, Watcher R, Schmoor C, Schumacher M, Junker B, Pielen A, European Assessment Group for Lysis in the Eye. Cardiovascular risk factors in central retinal artery occlusion: results of a prospective and standardized medical examination. Ophtalmology. 2015;122(9):1881-8.
7. Greven CM, Slusher MM, Weaver RG. Retinal arterial occlusions in young adults. Am J Ophtalmol. 1995;120(6):776-83.
8. Hayreh SS, Zimmerman MB. Central retinal artery occlusion: visual outcome. Am J Ophtalmol. 2005;140(3):376-91.
9. Biousse V, Newman N. Retinal and optical nerve ischemia. Continuum (Minneap Minn). 2014;20(4 Neuro-ophthalmology): 838-56.
10. Hayreh SS, Zimmerman MB. Fundus changes in central retinal artery occlusion. Retina. 2007;27(3):276-89.
11. Varma DD, Cugati S, Lee AW, Chen CS. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond). 2013;27(6):688-97.
12. Shinoda K, Yamada K, Matsumoto CS, Kimoto K, Nakatsuka K. Changes in retinal thickness are correlated with alterations of electroretinogram in eyes with central retinal artery occlusion. Graefes Arch Clin Exp Ophthalmol. 2008;246(7):949-54.
13. Hayreh SS, Zimmerman MB, Kimura A, Sanon A. Central retinal artery occlusion. Retinal survival time. Exp Eye Res. 2004; 78(3):723-36
14. Hayreh SS, Jonas JB. Optic disk and retinal fiber layer damage after transient central retinal artery occlusion: an experimental study in rhesus monkeys. Am J Ophthalmol. 2000;129(6):786-95.
15. Hayreh SS. Ocular vascular occlusive disorders: natural history of visual outcome. Prog Retin Eye Res. 2014 Jul;41:1-25.
16. Rudkin AK, Lee AW, Chen CS. Ocular neovascularization following central retinal artery occlusion: prevalence and timing of onset. Eur J Ophtalmol. 2010;20(6):1042-6.
17. Chang YS, Chu CC, Weng SF, Chang C, Wang JJ, Jan RL. The risk of acute coronary syndrome after retinal artery occlusion: a population-based cohort study. Br J Ophthalmol. 2015;99(2):227-31.
18. Park SJ, Choi NK, Yang BR, Park KH, Lee J, Jung SY. et al. Risk and risk periods for stroke and acute myocardial infarction in patients with central retinal artery occlusion. Ophthalmology. 2015;122(11):2336.e2-2343.e2.
19. Biousse V. Acute retinal arterial ischemia: an emergency often ignored. Am J Ophthalmol. 2014;157(6):1119-21.
20. Plant GT, Landau K. Thrombolysis for central retinal artery occlusion. J Neurol Neurosurg Psychiatry. 2005;76(2):160-1.
AUTHOR’S INFORMATION





Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
June 24, 2021.
Accepted on:
June 1, 2022.