Juliana Gomes da Silva1; Ana Clara Oliveira Gomes2; André Luís Celestino Ferreira2; Bianca Ferreira dos Santos2; Heldery Soares de Alustau2; Helga Larissa Barbosa Tiburtino3; Felipe Emery Rabello1; Rodrigo Correia Tiburtino1; Francisco Petrucci Palitot1; Aganeide Castilho-Palitot1
DOI: 10.17545/eOftalmo/2021.0003
ABSTRACT
PURPOSES: In recent years, arboviruses have been very important in public health due to their high incidence. The global dissemination of its vectors promoted the expansion of the Chikungunya virus, as well as its ophthalmological effects. Carry out a bibliographic search about the main ocular manifestations in the patients affected by the Chikungunya virus.
METHODS: Integrative bibliographical review carried out through a systematic research of scientific articles indexed in the online databases PubMed, Medline, Scielo, Health Portal Based on Evidence and Lilacs.
RESULTS: 10 articles were selected, published between 2007 and 2018. The main ocular manifestations in patients affected by Chikunguya virus were retinitis, granulomatous or non-granulomatous uveitis, photophobia, onset of acute visual loss, conjunctivitis, episcleritis, optic neuritis, oculomotor paralysis and retrobulbar orbital pain.
CONCLUSION: Ocular effects related to the Chikungunya virus affect patients of different ages and may involve from the anterior to the posterior segment of the eye. Thus, it is necessary to develop further studies that analyze the connection between Chikungunya virus infection and the onset of ocular diseases.
Keywords: Chikungunya; Ophthalmology; Arboviruses.
RESUMO
OBJETIVOS: Nos últimos anos, as arboviroses têm tomado destaque na saúde pública devido sua alta incidência. A disseminação global de seus vetores promoveu a expansão do vírus da Chikungunya, assim como seus efeitos clínicos oftalmológicos. Objetivando fazer um levantamento bibliográfico acerca das principais manifestações oculares nos pacientes acometidos pelo vírus da Chikungunya, foi realizada uma revisão integrativa.
MÉTODOS: Revisão bibliográfica com busca sistemática de artigos científicos indexados nas bases de dados online PubMed, Medline, Scielo, Portal Saúde Baseada Em Evidências e Lilacs.
RESULTADOS: Foram selecionados dez artigos, publicados entre os anos de 2007 a 2018. As principais manifestações oculares em indivíduos com Chikungunya foram retinite, uveítes granulomatosas ou não granulomatosas, fotofobia, início de perda visual aguda, conjuntivite, episclerite, neurite óptica, paralisia oculomotora e dor orbital retrobulbar.
CONCLUSÃO: Alterações oculares relacionadas ao vírus da Chikungunya acometem pacientes de diferentes idades e podem envolver desde o segmento ocular anterior até o posterior. Assim, faz se necessário o desenvolvimento de mais estudos que analisem a relação da infecção pelo vírus da Chikungunya e o surgimento ou agravo de doenças oculares.
Palavras-chave: Chikungunya; Oftalmologia; Arboviroses.
INTRODUCTION
Arboviroses are diseases transmitted to humans by arthropods, such as mosquitoes and ticks. These vectors transmit arboviruses, which include a wide variety of ribonucleic acid (RNA) viruses, such as flaviviruses (genus Flavivirus, one of the three genera of the Flaviviridae family) and alphaviruses (genus Alphavirus, one of the two genera of the Togaviridae family). The dengue fever virus and the Zika virus (ZIKV) are both flaviviruses, whereas the chikungunya virus (CHIKV) is an alphavirus1,2.
Arbovirus vectors are infected by the ingestion of blood from a human or animal with viremia. The ingested viruses then multiply, reach the vector’s salivary glands, and are passed on during the vector’s next meal. After infection, the clinical picture of arboviroses is usually nonspecific and includes fever, headache, arthralgia, and rashes. The increasing incidence of arboviroses is mainly due to rapid urbanization, inadequate urban infrastructure, the increasing amount of waste in urban environment, overpopulation, climate change, and more frequent international travels3.
Chikungunya is an emerging disease, specifically transmitted by female mosquitoes of the genus Aedes, such as A. aegypti in the Americans and A. albopictus in Asians. The clinical manifestations usually start between 4 and 8 days postinfection; however, this period can range from 2 to 12 days. This disease was first described in 1955 by Robinson and Lumsden, following an outbreak in 1952 in the Makonde plateau, along the border between Tanzania and Mozambique. The name “chikungunya” came from this outbreak, which in the local language means “that which bends,” referring to the curved posture of the affected patients resulting from the pain caused by the disease. After this outbreak, CHIKV was identified in more than 60 countries in Asia, Africa, Europe, and the USA; recent reports on the large-scale outbreaks reveal the resurgence of the virus in various parts of the world1,2,4.
Chikungunya disease is usually self-limiting; however, recent outbreaks have possibly been more severe than the previous ones, with more systemic manifestations and even death. The symptoms of the disease are similar to other arboviruses, including fever, myalgia, headache, and most particularly disabling joint pain. Ophthalmological findings are rare in this disease; however, some studies have reported ocular manifestations associated with CHIKV, such as conjunctivitis, optic neuritis, papillitis, neuroretinitis, panuveitis, episcleritis, keratitis, anterior uveitis, and retinitis2,5,6.
Thus, the clinical management of chikungunya is of paramount importance to be aware of its possible effects as well as to correlate the findings presented in different populations. Therefore, this study aimed to conduct a bibliographic survey of the available literature and to describe the main ocular manifestations in individuals infected with CHIKV.
METHODS
A systematic search of the indexed scientific articles was conducted in PubMed, Medline, SciELO, Evidence-Based Health Portal, and Lilacs. The keywords used were “chikungunya AND ophthalmology,” “CHIKV AND ophthalmology,” and “arboviroses AND ophthalmology.” The present review was based on previously selected studies that met the following inclusion criteria: randomized controlled clinical trials, case reports, case series, and systematic reviews on ocular manifestations resulting from CHIKV infection. Studies that did not report ocular manifestations resulting from CHIKV infection or reported only ocular manifestations of other arboviruses were excluded. Accordingly, the titles and abstracts were identified and independently analyzed by four reviewers; those that met the eligibility criteria were selected. The studies selected by one reviewer were passed on to another reviewer for further analysis to achieve greater reliability among the selected articles. In case of disagreement, the other two reviewers were consulted for a final verdict of inclusion or exclusion of a particular article. All eligible articles were completely read and the contents of the studies were extracted, considering all relevant aspects of the article.
RESULTS AND DISCUSSION
Overall 497 articles were found during the initial search using the chosen descriptors. Of these, 356 were excluded after the initial analysis. Of the remaining 141, 112 did not meet the required inclusion criteria. Therefore, 29 articles were selected for title and abstract analyses and application of inclusion and exclusion criteria. Finally, 10 articles meeting all the required criteria were selected.
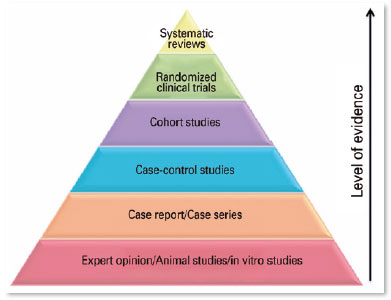
Of the 10 articles, five were bibliographic reviews, four were observational case studies, and one was a cohort study. Special attention was given to each study’s level of methodological importance, considering the pyramid of evidence, with case series and bibliographical reviews being placed at the base of the pyramid and representing 90% of the studies found. Only one7 was a cohort study, which was present at the top of the pyramid of evidence. This shows a deficiency with regard to the available scientific evidence on the proposed topic.
The year of publication was also analyzed, representing a time interval between 2007 and 2018, demonstrating a scarcity in the number of publications present, because this topic is somewhat innovative in the study of arboviruses and most of the reports are still emerging over time, due to a greater visibility and importance of the clinical findings in patients infected with CHIKV.
In the studies surveyed, the samples used usually had a small number of analyzed individuals. This may be a problem while analyzing the studies. In contrast, regarding the ocular alterations evaluated, all studies were satisfactorily well conducted, showing the pathological changes detected in the evaluated cases as well as the signs and symptoms resulting from these changes, in a methodological way. Table 1.
The analyzed studies showed that the pathophysiology of chikungunya is unclear. However, some studies in mice revealed the involvement of connective tissue, especially the epimysium, muscle tissue, joints, skin fibroblasts, and the central nervous system. Further, CHIKV was found in the biopsies of muscles, joints, and the dermis of the infected human patients. The natural cycle of the virus is human-mosquito-human. However, there is evidence of the existence of epizootic cycles that can preserve the virus in the interepidemic period. During epidemics, humans serve as reservoirs of CHIKV; during interepidemic periods, several vertebrates such as monkeys, rodents, and birds are implicated as the reservoirs. Vertical maternal–fetal transmission has been reported in pregnant women affected by chikungunya. CHIKV infects the human cornea and can be transmitted through corneal transplants1,8.
Generally, the clinical picture of arboviruses is nonspecific and in most cases includes fever, headache, arthralgia, and rashes. Certain signs often suggest a specific arbovirus, e.g., moderate fever and conjunctivitis for the ZIKV, leukopenia and thrombocytopenia for dengue, and severe arthralgia for CHIKV. Chikungunya can be a fatal disease and is generally characterized by the following symptoms: fever, headache, fatigue, nausea, vomiting, myalgia, rashes, joint pain, and general malaise. Further, infection by some emerging arboviruses such as chikungunya is accompanied by considerable eye involvement. Joint pain usually increases in the morning upon awakening and may persist for months and even years in some patients (published studies have reported variable proportions, from 5% to 60%), resulting in serious economic and social consequences for the individual as well as the affected communities. Deaths from this infection are rare (<1% infected individuals) and occur mainly in elderly patients1,3,4.
The cells attacked by CHIKV are mainly fibroblasts, epithelial cells, and lymphoid cells. Histologically, the synovial tissue of the infected individuals presents macrophages with viral material. Thus, at the ocular level CHIKV attacks fibroblasts from tissues such as the cornea, sclera, ciliary body, and oculomotor muscles, which may explain the ocular symptoms of this infection. The virus also affects the eye in myriad ways, ranging from conjunctivitis and retinitis to optic neuritis. During the initial stage of the disease, when systemic symptoms are being established, early ophthalmological manifestations include photophobia, conjunctival injection, and retro-orbital pain4,10.
Manifestations of CHIKV infection may involve the eye from the anterior up to the posterior segments. There are few publications on these manifestations; the most common symptoms reported are photophobia, retrobulbar orbital pain, and conjunctivitis, which may simulate other viral infections common during the initial stage of the disease. The main ocular manifestation is anterior uveitis that may be granulomatous or non-granulomatous and is often associated with pigmented brain precipitates and ocular hypertension. CHIKV anterior uveitis can be bilateral and resolves within weeks or months. Therefore, corneal donation is contraindicated in case of suspected chikungunya. Other symptoms commonly observed are blurred vision, fluctuation, epiphora, irritation, and diplopia, after a latent period from 1 month to 1 year (during the chronic phase)1,3,4,7,9,10.
Regarding the manifestations in the anterior ocular segment, CHIKV infection may lead to lagophthalmos and abducens nerve palsy and pigmented keratic precipitates with dendritic pattern on the endothelial epithelium of the cornea associated with corneal edema, thereby characterizing viral keratitis. Anterior uveitis, either granulomatous or non-granulomatous, is the most frequently reported complication and represents one third cases in the study7, which included 37 cases of CHIKV-related ocular complications. Other manifestations described in the anterior segment include scleritis, keratitis, cranial nerve palsy, nystagmus, and myositis1,3,4,9.
Other recurrent ocular manifestations described in one of the studies7 include optic neuritis, retrobulbar neuritis, and dendritic lesions. However, these manifestations can be derived from an immune process by the production of antibodies, rather than from a direct action of the viral infection. The same study showed that, when treated properly, these diseases presented a good prognosis. Therefore, early treatment and prevention of infection are measures that reduce the occurrence of the above mentioned complications and are required to avoid permanent functional impairment of vision7.
Manifestations in the posterior ocular segment are generally characterized by choroiditis, retinitis, neuroretinitis, and optic disc neuritis. Chikungunya retinitis may appear at the time of fever or only after several weeks or months of infection. The clinical features include mild vitreitis, hyperemic disc, retinal hemorrhages (due to the involvement of posterior-pole vessels), cotton-wool spots, multifocal retinitis (observed mainly in the periphery of the retina), retinal edema, and vascular impairment in the posterior pole1,2,4,9.
Early hypofluorescence with late hyperfluorescence was observed in fluorescein angiography images of patients with CHIKV, corresponding to areas with retinitis or vascular escape, and areas without capillary perfusion. Moreover, optical tomography may show hyperreflective areas that correspond to retinitis and hyporeflective areas that correspond to serous retinal detachment. Visual recovery of retinitis occurs between 10 and 12 weeks, presenting good results, with persistent pigment changes1,2,4,9.
Other findings in patients with chikungunya include bilateral external ophthalmoplegia, incongruent homonymous hemianopsia, occlusion of the central retinal artery, serous retinal detachment, multifocal choroiditis, and abducens nerve palsy. Some studies have reported that macular ischemia and optical disc alterations are responsible for the poor results observed in a minority of patients. In some cases of posterior uveitis, empirically treated with acyclovir (ineffective against RNA viruses), systemic steroids, and non-steroidal anti-inflammatory drugs in eye drops, a favorable outcome was experienced in less than 2 months1,9.
In view of this, a study in India with nine patients infected with CHIKV revealed that in addition to fever, headache, nausea, vomiting, chills, joint pain, and edema with varying intensity in the ankles, knees, and elbows, the patients also presented ophthalmological alterations. One patient presented nodular episcleritis, five had acute iridocyclitis, three had unilateral iridocyclitis, two had bilateral iridocyclitis with increased intraocular pressure ranging from 27 to 42 mmHg, and three presented retinitis. After treating their ophthalmic problems, the patients had a complete resolution of inflammation with the restoration of normal intraocular pressure. Thus, long-term sequelae of retinitis are unknown.
Chikungunya retinitis is similar to that of other infections; therefore, it is necessary to perform differential diagnosis, particularly for herpetic retinitis and cytomegalovirus retinitis, but these infections are more common in immunodeficient individuals and present more exuberant inflammation. However, a history of fever, joint pain, and rash before the onset of visual symptoms compatible with chikungunya is useful in diagnosis, particularly in endemic regions. Retinitis caused by the West Nile virus must also be ruled out1,2,4.
Optic neuropathy represents approximately 10% of the ocular involvement by CHIKV. The signs of optic neuropathy appear on average 1 month after the onset of the disease and patients complain of decreased visual acuity. Further, there may be a relationship between the onset of systemic manifestations and the onset of optic neuropathy3.
Chikungunya infection may also worsen the pre-existing cases of optic neuritis. According to studies, CHIKV infection can cause an acute onset of visual loss when associated with optic neuritis, and patients may also present ocular papillitis, retrobulbar neuritis, or neuroretinitis, but bilateral occurrence is rare. The optic tract may be involved in a small number of patients, with no evidence of optic chiasm involvement. The involvement of CHIKV in these ocular manifestations is not completely clarified. A small number of patients show evidence of direct effects of the infection, whereas most of them present a delayed immune response. Moreover, some characteristics indicate the possibility of an autoimmune mechanism being associated with the pathogenesis of the infection, such as less frequent occurrence of bilateral involvement, delayed onset of the response, and good response to corticosteroid therapy5,8.
Another possible ophthalmological manifestation of chikungunya is unilateral neuroretinitis, which was reported in a series of cases between 2014 and 2016. In that study, three patients infected with the virus underwent an ophthalmic evaluation, fundus examination, macular optical coherence tomography, and fluorescein angiography. All patients presented unilateral edema of the optic nerve and macular exudates in the affected eye. These findings are consistent with the diagnosis of unilateral neuroretinitis. The mechanism of unilateral or bilateral involvement observed in some patients is unclear; however, all patients in that study developed ocular manifestations several weeks after experiencing the acute phase of chikungunya, which corroborates other studies that demonstrated posterior segment manifestations appear several weeks after the acute phase of the disease. All patients had positive IgM, indicating that they had recent contact with the virus6.
Thus, based on the scientific evidence addressed, ocular changes resulting from CHIKV infection are extremely relevant, in view of the high frequency of patients presently affected. However, the pathogenicity mechanisms of CHIKV in ocular manifestations are not completely elucidated. It is possible to establish relationships between this infection and ophthalmic problems that affect certain patients. Some studies revealed that the virus can attenuate pre-existing ophthalmic diseases and may be related to the autoimmunity associated with CHIKV pathogenesis between manifestations.
CHIKV infection may affect the eye from the anterior to the posterior segments, with the following main manifestations: retinitis, granulomatous or non-granulomatous uveitis, photophobia, onset of acute visual loss, conjunctivitis, episcleritis, optic neuritis, oculomotor palsy, and retrobulbar orbital pain.
In face of the questions that still persist regarding the mechanisms of action of CHIKV in individuals and how the virus may be related to the reported ocular manifestations, greater efforts are required to conduct research that seeks to clarify these questions resulting in treatment measures that benefit patients. Furthermore, it is necessary to better educate the public about prophylaxis that interfere in the vector’s biological cycle, and ophthalmological monitoring by qualified professionals is important.
REFERENCES
1. Andrade GC, Ventura CV, Arruda Mello Filho PA, Maia M, Vianello S, Rodrigues EB. Arboviruses and the eye. Int J Retina Vitreous. 2017 Feb 1;3:4.
2. Mahendradas P, Ranganna SK, Shetty R, Balu R, Narayana KM, Babu RB, et al. Ocular manifestations associated with chikungunya. Ophthalmology. 2008;115(2):287-91.
3. Merle H, Donnio A, Jean-Charles A, Guyomarch J, Hage R, Najioullah F, et al. Ocular manifestations of emerging arboviruses: Dengue fever, Chikungunya, Zika virus, West Nile virus, and yellow fever. J Fr Ophthalmol. 2018;41(6):e235-e243.
4. Bechara CA, Restrepo CS. Manifestaciones Oculares de Infección del Virus del Chikunguña: Revisión de Literatura. Ver Soc Colomb Oftalmol. 2015;48(3):206-12.
5. Rose N, Anoop TM, John AP, Jabbar PK, George KC. Acute optic neuritis following infection with chikungunya virus in southern rural India. Int J Infect Dis. 2011;15(2):e147-50.
6. Davila PJ, Toledo A, Ulloa-Padilla J, Izquierdo NJ, Emanuelli A. Unilateral neuroretinitis as a lateonset manifestation of the chikungunya fever: a case series. Retin Cases Brief Rep. 2020; 14(1):44-8.
7. Lalitha P, Rathinam S, Banushree K, Maheshkumar S, Vijayakumar R, Sathe P. Ocular Involvement Associated With an Epidemic Outbreak of Chikunguya Virus Infection. Am J Ophthalmol. 2007 Oct;144(4):552-6.
8. Mittal A, Mittal S, Bharati MJ, Ramakrishnan R, Saravanan S, Sathe PS. Optic Neuritis Associated with Chikungunya Virus Infection in South India. Arch Ophthalmol. 2007;125(10):1381-6.
9. Mahendradas P, Avadhani K, Shetty R. Chikungunya and the eye: a review. J Ophthalmic Inflamm Infect. 2013;3(1):35.
10. Martínez-Pulgarín DF, Chowdhury FR, Villamil-Gomez WE, Rodriguez-Morales AJ, Blohm GM, Paniz-Mondolfi AE. Ophthalmologic aspects of chikungunya infection. Travel Med Infect Dis. 2016; 14(5):451-7.
AUTHOR’S INFORMATION








Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
June 2, 2020.
Accepted on:
October 16, 2020.