Davi Araf; Cinthia Mitie Araki dos Santos; Lara El Andere; Diego Del Bianco Dias Netto; Rodrigo Vuono de Brito; Thiciana Nader Bassitt
DOI: 10.17545/eOftalmo/2020.0012
ABSTRACT
We present a rare case of late postoperative complication following transconjunctival lower lid blepharoplasty performed for the removal of fat pads without skin resection. The young patient developed diplopia 30 days after the surgery owing to fibrosis involving the inferior oblique muscle. The patient responded well to corticosteroid therapy followed by surgical exploration with detachment of the local fibrotic tissue. The classic complications of transconjunctival lower lid blepharoplasty are discussed here, with emphasis on diplopia and its prevention. Diplopia following lower blepharoplasty is rare and mainly affects the inferior oblique muscle. The condition may be transient or permanent. Causes of transient diplopia include edema, hematoma, trauma with neuromuscular paresis, and muscle toxicity induced by local anesthesia. On the other hand, permanent diplopia results from direct trauma to the muscles or nerves. If the problem persists for >6 months, reparative surgery may be required.
Keywords: Diplopia; Inferior oblique muscle; Complication.
RESUMO
Apresentamos um caso raro de complicação cirúrgica tardia pós-blefaroplastia inferior transconjuntival para retirada de bolsas de gordura sem ressecção de pele, em que uma paciente jovem evoluiu com diplopia após 30 dias da cirurgia por fibrose envolvendo o músculo oblíquo inferior. O caso relatado mostrou boa resposta à corticoterapia seguida de exploração cirúrgica com liberação da fibrose local. Serão discutidas as complicações clássicas da blefaroplastia transconjuntival inferior com ênfase na diplopia e como evitá-la. A diplopia pós-blefaroplastia inferior é rara e acomete principalmente o músculo oblíquo inferior, e pode ser transitória ou permanente. As causas de diplopia transitória incluem edema, hematoma, traumatismo com paresia neuromuscular ou toxicidade muscular pelo anestésico local. Já a diplopia permanente resulta de trauma direto nos músculos ou nos nervos. Quando persiste mais que 6 meses pode demandar cirurgia reparadora.
Palavras-chave: Diplopia; Músculo oblíquo inferior; Complicação.
INTRODUCTION
The transconjunctival approach to orbital surgery was first described by Bourquet in 1924(1-4). The technique allows exposure of the orbital floor, maxilla, and extraocular muscles for several surgical procedures(4,5). In 1955, Tessier began using the transconjunctival incision for congenital malformations, post-traumatic deformities, and blepharoplasties(1-3,6-8). The first description of its use for aesthetic purposes dates back to the 1970s, during which Tomlinson and Baylis published on the topic(1,9). In 1991, Zarem and Resnick expanded the application of the transconjunctival approach to patients with fine lines and older patients with excess skin. These researchers stated that transconjunctival blepharoplasty had a lower rate of postoperative complications than the classical transcutaneous technique(1,2,6). The first laser-associated procedures were performed by Spandoni and Cain in 1988(10) and involved the resection of a thin strip of skin(11). These were combined with chemical procedures, laser resurfacing(11), or radiofrequency in addition to the classic indication for patients without skin flaccidity, who required only resection or repositioning of the palpebral pockets(1-5,7).
Transconjunctival lower lid blepharoplasty has numerous advantages over the transcutaneous technique, such as the reduced risk of retraction and ectropion. The former approach avoids the surgical manipulation of the retractor muscles of the lower eyelid and orbital septum, prevents the involvement of the anterior lamella when isolated, and provides ease of access to the middle third of the face. Besides, the technique reduces the surgical duration and offers the possibility of combining the procedure with other facial surgeries and skin treatments(2-5,10,12). The association of this technique with skin pinch and excision without detachment also offers the advantage of preserving the orbicularis oculi muscle and its innervation(2).
Studies have shown that this technique is superior to proper periorbital fat resection in addition to leaving the septum intact, which prevents eyelid retraction and xerophthalmia, offering lasting results(6). One of the main advantages of the transconjunctival approach when compared with the conventional technique is that the former causes neither denervation of the pretarsal portion of the orbicularis oculi muscle nor postoperative scarring(2,12). When only under-eye fat is excised without excess skin removal, there are practically no complications(6).
Known complications of transconjunctival lower lid blepharoplasty include hematomas, bruising below the orbital rim, prolonged edema, conjunctival chemosis, formation of pyogenic granuloma (mainly when the incision is sutured), and eyelid retraction (normally transient, lasting up to 4 months)(6). The risk of retrobulbar hemorrhage and amaurosis is low(9,10).
Diplopia after lower blepharoplasty may be transient or permanent and has several etiologies(13) including hemorrhage, edema, intramuscular cicatricial changes, muscle injury by surgical manipulation, and diffusion of local anesthetics such as bupivacaine(5,6,13,14).
CASE REPORT
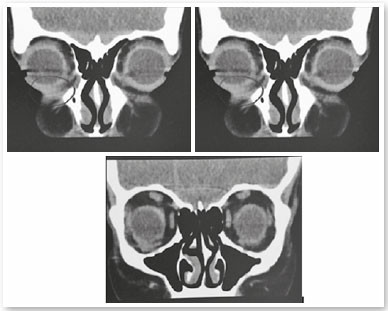
The patient, S.P.G., was a 35-year-old white female from São Paulo. She sought our service owing to the complaint of periorbital fat in her lower eyelids (Figure 1). External eye examination showed no other changes, and the patient denied any comorbidities. She underwent transconjunctival lower lid blepharoplasty in both eyes without any complications. After 30 days, the postoperative aesthetic aspect was satisfactory (Figure 2), but the patient reported restriction of movements in the right eye and mild diplopia in some positions of the gaze (Figure 3). Upon examination, slight restriction of right eye movements in sursumversion, deorsumversion, and abduction was observed, which was suggestive of the involvement of the inferior oblique muscle. After 2 months, restriction and diplopia persisted; thus, 2ml of a solution composed of triamcinolone 20mg/ml (Triancil®, Apsen Farmacêutica S.A. São Paulo – SP, Brazil) suspension for injection diluted in 2% xylocaine with a 1:1 vasoconstrictor was administered into the oblique muscle of the right lower eyelid. In the third postoperative month, the symptoms reduced and physical examination showed improvement of the restriction but also a decreased palpebral fissure during adduction, with a raised area in the central lower eyelid of the right eye. The hypothesis of fibrosis or residual fat was suggested (Figure 4). A new injection of triamcinolone at the same dosage was administered to the raised area. In the fifth postoperative month, the condition persisted; therefore, orbit computed tomography was requested, which showed densification of soft tissues and extraconal fat adjacent to the inferior oblique and inferior rectus muscles (Figures 5). In the sixth month, transconjunctival surgical exploration of the lower eyelid with fat excision close to the inferior oblique muscle and detachment of the surrounding local fibrotic tissue was indicated (Figure 6). Three weeks after the surgical exploration, the condition improved, but sporadic diplopia was observed (Figure 7). A new application of triamcinolone was then performed, leading to the complete elimination of muscle restriction and diplopia symptoms.






DISCUSSION
Injury to the inferior oblique muscle is infrequent; however, when it occurs, it can be quite debilitating(13). Transient diplopia following transconjunctival lower lid blepharoplasty is usually secondary to significant edema and ecchymosis(4). Prolonged diplopia may be a sign of injury to the extraocular muscle and may involve intramuscular hemorrhage caused by surgical handling or muscle transection(13). Studies suggest that transecting <50% of the muscle fibers does not result in permanent diplopia(13). Understanding the anatomy and using the precise techniques can avoid this type of injury(15).
The inferior oblique muscle originates from the anteromedial angle of the orbit, lateral and inferior to the lacrimal fossa, and gets inserted into the lateral sclera as a very short tendon of not more than 2mm. The muscle length is about 38mm(16). From its point of origin, it runs lateroposteriorly, penetrates the retractors of the lower eyelid in its middle third, envelops the globe in its final third, and facilitates the superomedial rotation of the eye(15).
The muscle emerges below and perpendicular to the inferior rectus, where it receives its innervation, a branch of the oculomotor nerve, and its blood supply(13). The most risky region for manipulation is 2mm lateral to the inferior rectus since injury in this area will often damage innervation and vascularization(13). Owing to the close association between the medial and central compartments, the inferior oblique muscle is susceptible to injuries(13).
Owing to the relatively upper incision in the conjunctiva of the lower eyelid and its tunneling below the lower fornice, the conjunctiva is subsequently separated from the capsulopalpebral fascia and the eyelid(15). This region is posterior to the lower lid orbital septum, and anterior tunneling should be performed to approach the fat located close to the inferior oblique muscle, both in the central and lateral thirds(13). Especially at the junction of the central third underlying the inferior rectus and Lockwood’s ligament, there is immense danger of transection of the inferior oblique muscle and injury to the nerve supply(15). The best approach to avoid this complication is to tunnel immediately anteriorly and then under the inferior tarsal muscle so that it is below the level of the inferior oblique muscle(15). It is possible to injure the medial inferior oblique muscle, but damage to this area is not as catastrophic as injury to the middle and lateral thirds(15).
Anterior to the retractor muscle of the lower eyelid is the orbital septum, which extends from the arcus marginalis of the lower orbital rim and gets inserted into the inferior tarsus(6). The septum acts as a barrier to the anterior prolapse of the structures and its weakening leads to the appearance of orbital fat that prolapses to the lower eyelid(6). There are three fat pads in the lower eyelid; the medial pad is separated from the central pad by the inferior oblique muscle located posterior to the transconjunctival surgical area, and the central pad is separated from the lateral pad by an extension of the retractor muscles of the lower eyelid(6,12).
The inferior oblique muscle can be severely injured during dissection, cauterization, or ligation of the medial and central fat pads(13). Muscle injury is diagnosed mainly by physical examination involving orthoptic measurements(13). Magnetic resonance imaging may reveal edema or scarring of the inferior oblique muscle(13). In partial injuries, symptoms usually resolve within 6 months of surgery(13). Complete injuries result in persistent strabismus, which necessitates surgery to repair the damage(13). Patients complain of diplopia in the ascending lateral gaze position and may even move their chins or heads in an attempt to alleviate the symptoms(13).
Identification of the orbital border, infraorbital foramen, and supraorbital fossa helps better locate the origin and course of the inferior oblique muscle, thereby facilitating fat resection during lower lid blepharoplasty and preventing muscle injury(13). The inferior oblique muscle is more vulnerable to injuries than the other longitudinally oriented extraocular muscles because of its transverse orientation(13).
Several surgical maneuvers have been proposed to minimize the occurrence of this muscle injury. One of them is to avoid very low transconjunctival incisions(13,15). Several authors have specified an incision 10mm below the corneal limbus on the side of the eyelid(13,15). Many surgeons have advocated the delineation of the muscle location at the beginning of the procedure, before fat resection(13). Finally, gentle traction of the fat pads before resection is recommended to confirm the lack of movement of the eye bulb(6,13,17).
Initial treatment of diplopia is conservative even in the case of iatrogenic trauma(18). Patients may make use of prisms temporarily if necessary(5,18).
Lower lid blepharoplasty, even when performed by trainee plastic surgeons, is a safe and reproducible procedure with a low rate of complications, provided it is executed correctly(1,10). However, even the most talented and experienced surgeons tend to face complications, which can be minimized by careful preoperative evaluation, adequate expectations, meticulous and individualized surgical judgment, thorough anatomical knowledge, and early recognition of adverse events followed by suitable treatments(3,13,18).
REFERENCES
1. Rezai, K. (2019). Transconjunctival lower lid blepharoplasty by radiofrequency surgery - Cosmetic Medicine. [online] Cosmetic Medicine. Available at: https://www.cosmeticmedicine-online.com/reviews/transconjunctival-lower-lid-blepharoplasty-radiofrequency-surgery/#literature [Accessed 1 Jul. 2019].
2. Ghabrial, R., Lisman, R., Kane, M., Milite, J. and Richards, R. (1998). Diplopia following Transconjunctival Blepharoplasty. Plastic and Reconstructive Surgery, 102(4), p.1219-1225.
3. Subramanian, N. (2008). Blepharoplasty. Indian Journal Plastic Surgery, 41(3), p.88-92.
4. González-Ulloa, M. (1983). An update on blepharoplasty. Aesthetic Plastic Surgery, 7(1), p.1-11.
5. Graf, R., Auerswald, A., Bernardes, A., Damasio, R., Araujo, L. and Graf, C. (2001). Blefaroplasia Inferior Transconjuntival. Revista da Sociedade Brasileira de Cirurgia Plástica, 16(2), p. 59-74.
6. Raus, P. (2017). Transconjunctival lower lid blepharoplasty made easy by everting the eyelid. International Journal of Ophthalmology & Eye Science, 5(5) p.313-315.
7. Chen WP. Cirurgia Plástica Oftalmológica, princípios e práticas. Shorr N, Perry, JD. Blefaroplastia inferior e a queda da parte medial da face. 2005. Revinter. Capítulo 11. p. 147-163.
8. Yachouh, J., Arnaud, D., Jammet, P. and Goudot, P. (2005). La blépharoplastie inférieure par voie conjonctivale. Revue de Stomatologie et de Chirurgie Maxillo-faciale, 106(6), p.344-348.
9. Branham, G. (2016). Lower eyelid blepharoplasty. Facial Plastic Surgery Clinics of North America, 24 (2), p. 129-138.
10. Segal, K., Patel, P., Levine, B., Lisman, R. and Lelli, G. (2015). The Effect of Transconjunctival Blepharoplasty on Margin Reflex Distance 2. Aesthetic Plastic Surgery, 40(1), p.13-18.
11. Bernardino, I. (2016). Blefaroplastia inferior transconjuntival associada à ressecção cutânea com preservação do músculo orbicular. Revista Brasileira de Cirurgia Plástica, 31(1): p.74-81.
12. Pack, S., Quereshy, F., Altay, M. and Baur, D. (2016). Transconjunctival Lower Blepharoplasty. Atlas of the Oral and Maxillofacial Surgery Clinics, 24(2), pp.147-151.
13. Mowlavi, A., Neumeister, M. and Wilhelmi, B. (2002). Lower Blepharoplasty Using Bony Anatomical Landmarks to Identify and Avoid Injury to the Inferior Oblique Muscle. Plastic and Reconstructive Surgery, 110(5), p.1318-1322.
14. Putterman, A. (2004). Acquired strabismus following cosmetic blepharoplasty. Plastic and Reconstructive Surgery, 113(3), p.1069-1070.
15. Frankel, J. (2003). Avoiding injury to the inferior oblique muscle during lower lid blepharoplasty. Plastic and Reconstructive Surgery, 112(7), p.1958-1959.
16. Souza-Dias C, Goldchmit M. Os Estrabismos. Função Motora. 2011. Cultura Médica. Capítulo 1. p. 3-13.
17. Maffi, T., Chang, S. and Friedland, J. (2011). Traditional lower blepharoplasty: is additional support necessary? A 30 year rewiew. Plastic and Reconstructive Surgery, 128, p. 265-273.
18. Lelli, G. and Lisman, R. (2010). Blepharoplasty Complications. Plastic and Reconstructive Surgery, 125(3), p.1007-1017.
AUTHOR’S INFORMATION



Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
May 19, 2020.
Accepted on:
July 6, 2020.