Vinicius C. Falcão; Tiago A. Carvalho; Fernanda B. Nonato Federici; Márcio A. N. Costa
DOI: 10.17545/eOftalmo/2020.0004
ABSTRACT
Photodynamic therapy is an important treatment for choroidal hemangioma treatment. Here, we present the case of a patient with choroidal hemangioma who responded to initial treatments, such as anti-VEGF and argon laser photocoagulation, leading to the consideration of photodynamic therapy that achieved a satisfactory result in a short time. At the time of writing this report, the patient had been followed-up for >1 year without recurrence. We present examination and comparisons for the identification of superior results and techniques.
Keywords: Retina; Photochemotherapy; Choroid; Hemangioma.
RESUMO
A terapia fotodinâmica é um método terapêutico de grande valia no tratamento do hemangioma de coroide. Neste trabalho, apresentamos um caso de hemangioma de coroide que não obteve resultado inicial com outros tratamento como o anti-VEGF e a fotocoagulação com laser de argônio optando-se assim pela realização da terapia fotodinâmica, obtendo-se um resultado satisfatório em pouco tempo. O paciente continua em acompanhamento sem recidiva em mais de um ano e os estudos e comparações são feitas em busca de melhores resultados e técnicas.
Palavras-chave: Retina; Fotoquimioterapia; Coróide; Hemangioma.
INTRODUCTION
Circumscribed choroidal hemangioma is a benign, uncommon vascular tumor of the choroid. In general, it is orange-red in color, of very limited retroequatorial location, rounded, and not very prominent(1).
The treatment of circumscribed choroidal hemangioma is reserved for the symptomatic forms that generally involve complications and macular exudates(1). Photodynamic therapy (PDT) has emerged as an effective alternative to radiation therapy and argon laser photocoagulation(2).
Light activation of verteporfin causes the release of free radicals that induce irreversible damage to the vascular endothelium. This reaction causes activation and adhesion of the platelets, resulting in thrombosis of the vascular structures. The main limitation of PDT is related to the inflammatory reaction secondary to vascular thrombosis of the choroid that can sometimes lead to persistent subretinal fluid and the need to perform the procedure again(2).
Here, we describe the case of a patient with circumscribed choroidal hemangioma who did not respond well to anti-VEGF and argon laser treatment, with PDT being proposed as a better treatment.
CASE REPORT
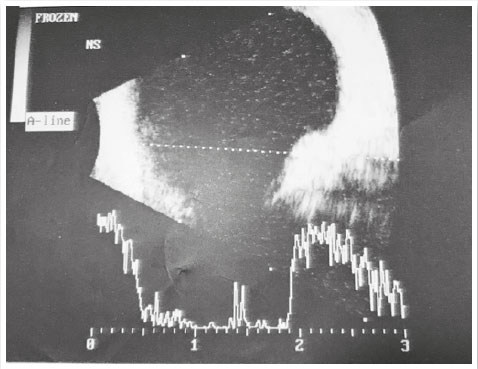
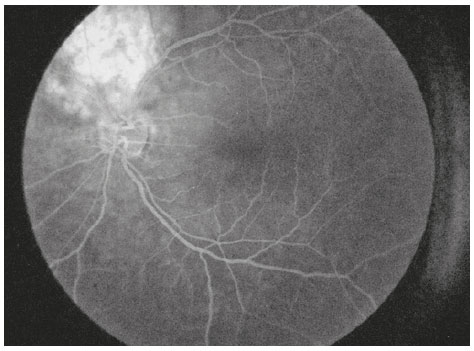
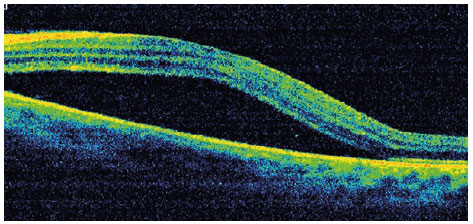
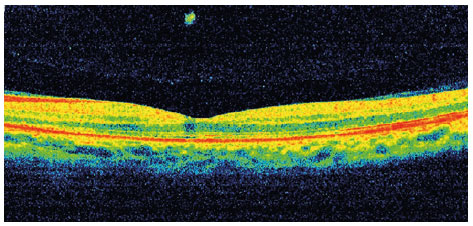
A 40-year-old male aircraft pilot visited a healthcare institution complaining of low visual acuity for 7 days in the OS. He denied any history of eye disorders. Visual acuity was 20/20 OD and 20/40 OS. No changes were observed in past examinations of biomicroscopy and OD fundoscopy. In the OS, an optical disc of normal dimensions was observed; we also observed an elevated, orange lesion in the superior temporal arch along with macular edema (Figure 1). Additional exams were performed, and an ultrasonography scan demonstrated an elevated dome-shaped lesion in the eyeball wall at the 10 o’ clock meridian, of high reflectivity and homogeneity (AP: 10.7mm, height: 4.3mm) (Figure 2). Angiography evidenced a hyperfluorescent lesion above the disc (Figure 3), while OCT showed elevation of the choroid with serous detachment of the macula. Seven days following the first appointment, he exhibited worsening of (corrected) visual acuity to 20/70 OS and the serous detachment in the macular area (Figure 4). These results enabled the diagnosis of choroidal hemangioma, and argon laser and intraocular application of anti-VEGF were selected for treatment, without any improvement of the condition. Thus, photodynamic therapy was performed. After 30 days of treatment, the patient returned with a 20/20 visual acuity OS. Fundoscopy revealed a lower lesion (height: 3.0mm upon US) along with serous detachment. The OCT showed no evidence of subretinal fluid in the macular area, with preserved retinal layers (Figure 5).

DISCUSSION
Recently, unlike laser photocoagulation, PDT has shown high selectivity for subretinal vascular structures, creating intraluminal thrombosis linked to the specific vascular endothelium and anatomically sparing retinal layers(3-6).
A case report on two patients with circumscribed choroidal hemangioma(6) demonstrated not only total regression of the tumor following PDT, but also significant improvements in the central and peripheral visual acuity because of subretinal fluid resorption and macular edema resolution. After 9 months and 1 year of follow-up, these patients showed no recurrence on clinical examination or in imaging studies. Functional improvements were maintained in these patients although there was involvement of the fovea, given the pathology and PDT.
Another case study reported a mean visual improvement of three lines at the 1-year follow-up. Visual improvement was observed in patients with subfoveal tumors. Thereafter, very promising cases of extra-foveal location have been presented by other groups(5,7-9).
In 2009(10), the first three cases of choroidal hemangioma treated with the administration of intravitreal anti-VEGF injections were reported. The first patient was treated only with an intravitreal injection of bevacizumab; after recurrence, argon laser photocoagulation was performed. The other two patients received intravitreal injections of bevacizumab combined with PDT as the primary treatment. The last patient demonstrated complete resolution of the subfoveal edema within 1 month of therapy, while the first patient showed complete resolution of edema after the final laser photocoagulation session. In another case(11), PDT was used, and after the persistence of cystoid and subfoveal macular edema, intravitreal injection of bevacizumab was administered. The authors noticed rapid regression of the edema after two weeks of the procedure. All the patients were given combined treatment of intravitreal bevacizumab injections and PDT, while one patient was administered argon laser photocoagulation treatment.
A recent study has compared a double dose and the standard dose of PDT; the study reported that both these doses were effective in promoting subretinal fluid resorption; however, the double dose was more effective in promoting tumor regression. Moreover, the 1-year rate of complete reabsorption of the subretinal fluid was higher in the double-dose group as compared to that in the standard-dose group (80% vs. 57%), while the recurrence rate was lower in the double-dose group (0% vs. 28.6%). Although the objective of the treatment was not to flatten the tumor completely, we believe that a double dose of verteporfin is more effective for regression of the tumor, promotion of subretinal fluid resorption, and prevention of recurrence(12).
These results may be related to more selective laser uptake via an increase in the verteporfin dose, although a prospective comparative study is necessary to assess the relative efficacy and therapeutic mechanisms of double-dose and single-dose PDT using the age-related pattern and the protocol of macular degeneration in the treatment of circumscribed choroidal hemangioma(12).
In the present case, we first administered local treatment with argon laser and intravitreal injection of anti-VEGF; these treatments did not demonstrate any visual or anatomical improvement. Thus, treatment with isolated PDT without anti-VEGF was proposed, and 30 days after the procedure, the lesion was completely resolved, with no sign of subfoveal edema and significantly improved visual acuity.
Favorable functional and anatomical results have been observed with PDT that is a minimally invasive and effective treatment method of treating intraocular hemangiomas. The results suggest that PDT can be considered a gold standard treatment for treating patients with symptomatic choroidal hemangiomas. A better understanding of the photodynamic effects and their long-term results are necessary and are currently being examined(6).
REFERENCES
1. Bazin L, Gambrelle J. [Combined treatment with photodynamic therapy and intravitreal dexamethasone implant (Ozurdex(®)) for circumscribed choroidal hemangioma]. J Fr Ophtalmol. 2012; 35(10):798-802.
2. Gambrelle J, Graswill C, Mauget Fa¨ysse M, Kodjikian L, Cochener B, Grange JD. Traitement des hémangiomes choroïdiens circonscrits par photothérapie dynamique: revue de la littérature. J Fr Ophtalmol. 2010;33:497-504.
3. Chan LW, Hsieh YT. Photodynamic therapy for choroidal hemangioma unresponsive to ranibizumab. Optom Vis Sci. 2014;91(9):e226-9.
4. Schmidt-Erfurth U, Hasan T, Gragoudas E, Michaud N, Flotte TJ, Birngruber R. Vascular targeting in photodynamic occlusion of subretinal vessels. Ophthalmology. 1994;101:1953Y61.
5. Michels S, Michels R, Simader C, Schmidt-Erfurth U. Verteporfin therapy for choroidal hemangioma: a long-term follow-up. Retina. 2005;25(6):697-703
6. Barbazetto I, Schmidt-Erfurth U. Photodynamic therapy of choroidal hemangioma: two case reports. Graefes Arch Clin Exp Ophthalmol. 2000;238(3):214-21.
7. Schmidt-Erfurth U, Michels S, Kusserow C, et al. Photodynamic therapy for symptomatic choroidal hemangioma. Ophthalmology. 2002;109:2284–94.
8. Porrini G, Giovannini A, Amato G, et al. Photodynamic therapy of circumscribed choroidal hemangioma. Ophthalmology. 2003; 110:674-80.
9. Jurklies B, Anastassiou G, Ortmans S, et al. Photodynamic therapy using verteporfin in circumscribed choroidal haemangioma. Br J Ophthalmol. 2003;87:84-9.
10. Sagong M, Lee J, Chang W. Application of intravitreal bevacizumab for circumscribed choroidal hemangioma. Korean J Ophthalmol. 2009;23:127Y31.
11. Hsu CC, Yang CS, Peng CH, Lee FL, Lee SM. Combination photodynamic therapy and intravitreal bevacizumab used to treat circumscribed choroidal hemangioma. J Chin Med Assoc. 2011;74:473Y7.
12. Lee JH, Lee CS, Lee SC. Efficacy of double dose photodynamic therapy for circumscribed choroidal hemangioma. Retina. 2019; 39(2):392-7.
AUTHOR’S INFORMATION




Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
October 8, 2019.
Accepted on:
January 27, 2020.