Rafael Cerqueira Alves1; Francisco Assis de Andrade2; Jacqueline Provenzano3
DOI: 10.17545/eoftalmo/2018.0034
ABSTRACT
Pseudophakic cystoid macular edema (CME) is one of the possible causes of low visual acuity following cataract surgery. In this report, the authors describe the case of a patient with a history of recurrent uveitis and a confirmed diagnosis of reactive arthritis due to Chlamydia trachomatis. He developed cataract and was referred for surgery, which occurred without complications. However, on postoperative day 1, the patient presented with refractory uveitis. Despite topical and oral anti-inflammatory therapy, he developed extensive CME, which was confirmed on postoperative day 26 through optical coherence tomography and fluorescence retinography. Treatment with sub-Tenon’s injection of triamcinolone was proposed, and 12 days later, his condition improved. At the 3-month follow-up, no recurrence of macular edema was observed.
Keywords: Triamcinolone; Macular Edema; Uveitis; Chlamydia trachomatis.
RESUMO
O edema macular cistoide (EMC) pseudofácico é uma das possíveis causas de baixa acuidade visual após cirurgia de catarata. Neste relato, descreve-se o caso de paciente com história de uveíte de repetição com diagnóstico confirmado de artrite reativa por Chlamydia trachomatis, no qual desenvolveu catarata e foi encaminhado para facectomia. A cirurgia ocorreu sem intercorrências, porém o paciente apresentou reativação da uveíte no primeiro dia pós-operatório com membrana inflamatória. Mesmo com a terapia anti-inflamatória tópica e oral, desenvolveu extenso edema macular cistoide, confirmado no vigésimo sexto dia pós-operatório pela tomografia de coerência óptica e retinografia fluorescente. Proposto o tratamento com triancinolona sub-tenoniana, o quadro entrou em remissão 12 dias após. Com o controle de 3 meses não apresentava recidiva do edema macular.
Palavras-chave: Triancinolona; Edema Macular; Uveíte; Chlamydia trachomatis.
RESUMEN
El edema macular cistoide (EMC) pseudofáquico es una de las posibles causas de baja acuidad visual post cirugía de catarata. En este reporte, se describe el caso de un paciente con historia de uveítis de repetición con diagnóstico confirmado de artritis reactiva por Chlamydia trachomatis, en el cual desarrolló catarata y fue encaminado a cirurgía de catarata. La cirugía ocurrió sin complicaciones, sin embargo, el paciente presentó reactivación de la uveítis en el primer día del post operatorio con membrana inflamatoria. Aun con la terapia antiinflamatoria tópica y oral, desarrolló extenso edema macular cistoide, confirmado en el vigésimo sexto día postoperatorio por la tomografía de coherencia óptica y retinografía fluorescente. Se propuso el tratamiento con triamcinolona subtenoniana, y el cuadro entró en remisión 12 días después. Con el control de 3 meses no presentaba recidiva del edema macular.
Palabras-clave: Triamcinolona; Edema Macular; Uveítis; Chlamydia trachomatis.
INTRODUCTION
Complications from cataract surgery are occasionally inherent to uneventfully performed procedures1. Patients with pro-inflammatory eyes, such as in the present clinical case, are more predisposed to present complications2. Patients with a history of uveitis undergoing cataract surgery require special attention because the procedure can cause complications such as cystoid macular edema (CME)3,4.
Administration of topical and systemic corticosteroids is very common in clinical practice and can reduce eye inflammation and its complications. This was performed in the present case; however, oral corticosteroids can cause unwanted systemic effects5. An intensive perioperative regimen of topical corticosteroids was found to be statistically comparable to oral corticosteroids in preventing the recurrence of postoperative uveitis6.
Cases in which CME is present even following administration of both oral and topical corticosteroids7 require a more invasive therapy8, and the choice among the available options should consider good results and few adverse effects5,6,8,9,10,11. Sub-Tenon’s triamcinolone injection should be considered as both a prophylactic and a therapeutic option for CME because although intravitreal injection has a greater action, it is more likely to increase intraocular pressure, is more invasive, and has a risk of causing endophthalmitis8. In phakic patients, the treatment may change because the use of corticosteroids increases the incidence of early cataracts12.
METHODS
This case report describes a patient referred for cataract surgery with a history of reactive arthritis induced by Chlamydia trachomatis and recurring episodes of uveitis in both eyes. Surgery was performed uneventfully, but with reactivation of uveitis and CME that was refractory to the initial treatment. Sub-Tenon’s triamcinolone (0.2 mL, 40 mg/mL) was proposed as treatment.
CASE REPORT
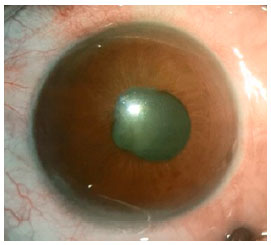
E.F.P.C., a 52-year-old man of mixed Caucasian and African ethnicity born in Rio de Janeiro was referred to us for right eye (RE) cataract surgery in July 2016. He had been diagnosed with reactive arthritis caused by Chlamydia trachomatis at 20 years of age and had a history of recurrent uveitis; he could not recollect the precise number of episodes. Topical treatment with corticosteroid eye drops and oral anti-inflammatory drugs, both steroidal and non-steroidal (NSAID), had been prescribed several times. The patient initiated the treatment on his own as soon as signs and symptoms developed; this was later confirmed by his ophthalmologist. His visual acuity (VA) by the Snellen chart with preoperative correction was 20/80 in the RE and 20/20 in the left eye. RE biomicroscopy revealed three posterior synechiae that reduced mydriasis to 4 mm, a 1+/4+ nuclear cataract, and a 3+/4+ subcapsular posterior cataract. The intraocular pressure (IOP) was 14 mmHg in both eyes. Ophthalmoscopy of this eye was unsatisfactory, so ocular ultrasonography (USG) was performed. USG results showed only partial detachment of the posterior vitreous and attached retina. The surgery and its possible complications were explained to the patient. The cataract surgery was performed uneventfully on August 25, 2016, and an intraocular lens (IOL) was implanted (Figure 1). The synechiae were mechanically released, and the iris was stretched to increase mydriasis. At the end of the surgery, hydrocortisone 100 mg was administered intravenously.
PRESCRIPTION
Ocular use: Moxifloxacin hydrochloride 5.45 mg/mL (Vigamox®) every 4 h for 15 days; ketorolac tromethamine 5 mg/mL (Cetrolac®) every 12 h for 30 days; dexamethasone 1.0 mg/mL (Maxidex®) every 2 h for 7 days, then every 4 h for 7 days, every 6 h for 5 days, every 8 h for 5 days, every 12 h for 5 days, and finally every 24 h for 3 days.
On the first day (D1) postoperatively (PO), the patient presented uncorrected VA counting fingers at 2 meters. Biomicroscopy revealed an inflammatory membrane in the pupillary region extending to the superior corneal endothelium, topical IOL, dysmorphic pupil, corneal edema 1+/4+, ocular hyperemia 2+/4+, Tyndall 4+/4+, flare 1+/4+, and IOP 14 mmHg. Oral prednisone 60 mg/day for 2 days was prescribed, and the dose was reduced thereafter by 10 mg every 5 days.
On the seventh day PO (D7), uncorrected VA was 20/200, Tyndall and flare 1+/4+, and IOP 12 mmHg.
On the twenty-first day PO (D21), the patient presented a corrected VA of 20/100-1, no inflammatory activity was observed on biomicroscopy (Figure 2), and IOP was 12 mmHg. Pupil dilation was performed and macular edema was observed. Cetrolac® was changed to every 8 h, complementary tests were scheduled, and triamcinolone was considered as a therapeutic option.

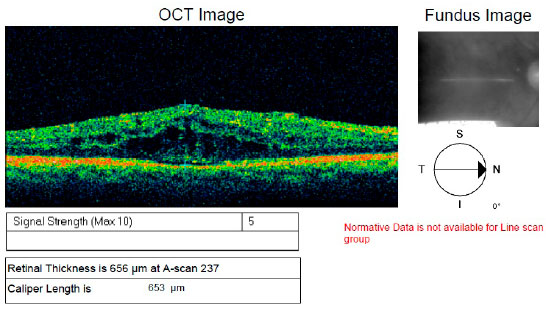
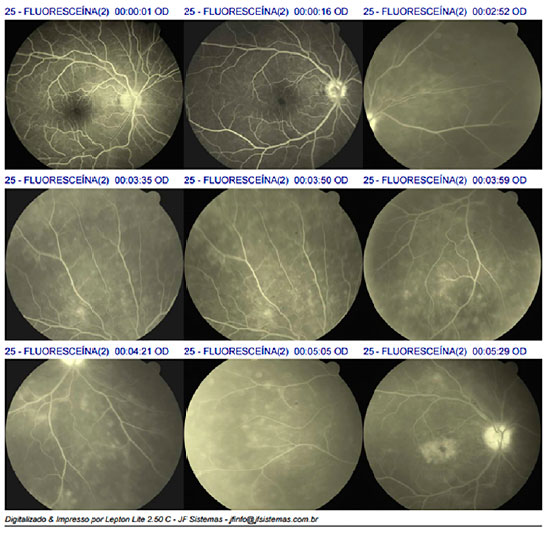
On D26 PO, retinal angiography with sodium fluorescein was performed (Figure 4), revealing a CME in a petaloid pattern. Optical coherence tomography (OCT-Stratus) was also performed and revealed a CME that was 659 µm thick (Figure 3). On the same day, a temporal-superior sub-Tenon’s injection of triamcinolone (0.2 mL at 40 mg/mL) was applied to the RE. Topical eye drops of brimonidine D-tartrate 0.2% with timolol maleate 0.5% (Combigan®) every 12 h were prescribed, as well as ciprofloxacin 3.5 mg/g with dexamethasone 1.0 mg/g (MaxifloxD®) every 6 h for 5 days.
On D27 PO, 1 day after the procedure, the patient presented with no complaints, biomicroscopy revealed no inflammatory activity, and IOP was 8 mmHg.
On D31 PO, 5 days after the procedure, corrected VA was 20/60+3 and IOP was 10 mmHg.
On D38 PO, 11 days after the procedure, corrected VA was 20/25-1 and IOP was 10 mmHg. OCT was performed, and the macula appeared with a central thickness of 217 µm (Figure 5). A hyperreflective membrane was observed on the internal surface of the retina, suggesting an epiretinal membrane.
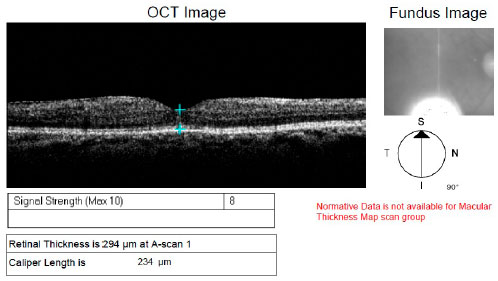
One month after triamcinolone application, vision, IOP, and macular appearance on OCT (Figure 6) were stable.
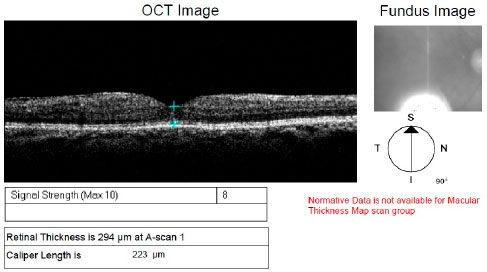
Three months after triamcinolone application, vision and IOP remained stable. The macular appearance on OCT (Figure 7) showed the presence of an epiretinal membrane. Surgical removal was not indicated as the patient had good vision.
RESULTS
After 21 days of treatment with the NSAID and topical and oral corticosteroids, ocular inflammation ceased, but there was no improvement in the satisfactory VA; therefore, CME was diagnosed. After posterior sub-Tenon’s administration of 0.2 mL triamcinolone (40 mg/mL), macular thickness was reduced from 659 to 217 µm in only 12 days, improving corrected VA from 20/100-1 to 20/25-1, which persisted after 3 months of follow-up.
DISCUSSION
Pseudophakic CME, also known as Irvine–Gass syndrome, is a possible cause of low VA after cataract surgery. Despite the advances in cataract surgery, with microincision and new phacoemulsification techniques, CME can occur even after uneventful surgeries1.
The pathogenesis of CME is still not well known, but there are several risk factors for its appearance, such as the preoperative use of prostaglandins, epiretinal membrane, history of retinal venous occlusion, ocular hypotonia, and vitreomacular traction3. Inflammatory mediators are involved in the increase in vascular permeability and transudation to the macular region1. Diabetics in particular require special attention3 because of the difficultly in distinguishing diabetic macular edema from CME13.
The incidence of CME increases when surgical complications occur3, such as posterior capsular rupture, vitreous loss, vitreous incarceration, residual fragments of vitreous cortex, iris trauma, IOL dislocation, iris fixation, anterior-chamber IOL, and early posterior capsulotomy1,2,6. In the present case, surgery was performed without immediate complications.
Diagnosis is essentially clinical, but it is supported especially by fluorescein angiography (the gold standard) and OCT to clarify doubtful cases. These tests are also essential during follow-up14.
Patients with a previous history of uveitis, such as in the present case, are at an increased risk of reactivation and of developing CME compared with patients with no reported ocular inflammation2,3,4. The latter must be controlled before surgery, postoperative follow-up must be stringent, and perioperative prophylaxis with sub-Tenon’s triamcinolone at the end of the surgical procedure must be considered5,6,15.
A combination of ketorolac tromethamine with topical corticosteroids is a noninvasive option for CME prophylaxis in patients undergoing cataract surgery7. However, in the present case, it was insufficient to prevent this inflammatory complication.
A small, uncontrolled, randomized clinical trial found an intensive perioperative scheme of topical corticosteroids to be statistically comparable to oral corticosteroids for preventing postoperative uveitis recurrence. However, the recurrence rate was greater6.
As alternatives to the anti-inflammatory treatment, more invasive procedures, such as the application of sub-Tenon’s and intravitreal triamcinolone, as well as intravitreal dexamethasone implants, can be considered7,8,9,12. Vascular endothelial growth factor inhibitors (anti-VEGF) are another option for a more invasive treatment of these cases of macular edema10.
There are several options for treating this complication. The most adequate strategy involves evaluating each patient and then selecting the method that provides the best response with the greatest safety. A more invasive treatment may be necessary to resolve some cases. The choice of using sub-Tenon’s triamcinolone in the present case was demonstrated to be safe and to provide a sustained resolution of the complication16.
REFERENCES
1. Yonekawa Y, Kim IK. Pseudophakic cystoid macular edema. Curr Opin Ophthalmol. 2012; 23(1):26-32.
2. Chu CJ, Johnston RL, Buscombe C, Sallam AB, Mohamed Q, Yang YC; United Kingdom Pseudophakic Macular Edema Study Group. Ophthalmology. 2016 Feb; 123(2):316-23. doi: 10.1016/j.ophtha.2015.10.001. Epub 2015 Dec 8.
3. Henderson BA, Kim JY, Ament CS, Ferrufino-Ponce ZK, Grabowska A, Cremers SL. Clinical pseudophakic cystoid macular edema. Risk factors for development and duration after treatment. J Cataract Refract Surg. 2007; 33(9):1550-8.
4. Belair ML, Kim SJ, Thorne JE, Dunn JP, Kedhar SR, Brown DM, et al. Incidence of cystoid macular edema after cataract surgery in patients with and without uveitis using optical coherence tomography. Am J Ophthalmol. 2009; 148(1):128-35.
5. Roesel M, Heinz C, Koch JM, Heiligenhaus A. Comparison of orbital floor triamcinolone acetonide and oral prednisolone for cataract surgery management in patients with non-infectious uveitis. Graefes Arch Clin Exp Ophthalmol. 2010; 248:715-20.
6. Mora P, Gonzales S, Ghirardini S, Rubino P, Orsoni JG, Gandolfi, Majo F, Guex-Crosier Y. Perioperative prophylaxis to prevent recurrence following cataract surgery in uveitic patients: a two-centre, prospective, randomized trial. Acta Ophthalmol 2016 Sep; 94(6):e390-4.
7. Yilmaz T, Cordero-Coma M, Gallagher MJ. Ketorolac therapy for the prevention of acute pseudophakic cystoid macular edema: a systematic review. Eye. 2012; 26(2):252-8.
8. Roesel M, Gutfleisch M, Heinz C, Heimes B, Zurek-Imhoff B, Heiligenhaus A. Intravitreal and orbital floor triamcinolone acetonide injections in noninfectious uveitis: a comparative study. Ophthalmic Res. 2009; 42(2):81-6. doi: 10.1159/000220600. Epub 2009 May 27.
9. Mylolas G, Georgopoulos M, Malamos O, Georgalas I, Koutsandrea C, Brouzas D, Sacu S, Perisanidis C, Schimidt-Erfurth U; Macula Study Group Vienna. Comparison os dexamethasone intravitreal implant with conventional triamcinolone in pacients with postoperative cystoid macular edema. Curr Eye Res. 2016 Sep; 9:1-5.
10. Izdebski B, Michaleweska Z, Dziegielewski K, Nawrocki J, Odrobina D. Treatment of cystoid macular edema with bevacizumab in course of Irvine-Gass syndrome. Klin Oczna. 2013; 115(1):61-4.
11. Chan NS, Ti SE, Chee SP. Decision-making and management of uveitic cataract. Indian J Ophthalmol. 2017 Dec; 65(12):1329-39. doi: 10.4103/ijo. IJO_740_17. Review.
12. Yan PS, Qian C, Wan GM, Wang WZ, Dong Y, Li FZ. Clinical effect of intravitreous injection of triamcinolone acetonide in treating cystoid macular edema. J Biol Regul Homeost Agents. 2016 Jan-Mar; 30(1):205-10.
13. Writing C, Baker CW, Almukhtar T, Bressler NM, Glassman AR, Grover S, et al. Macular edema after cataract surgery in eyes without preoperative central-involved diabetic macular edema. JAMA Ophthalmol. 2013; 131(7):870-9.
14. Kusbeci T, Eryigit L, Yavas G, Inan UU. Evaluation of cystoid macular edema using optical coherence tomography and fundus fluorescein angiography after uncomplicated phacoemulsification surgery. Curr Eye Res. 2012; 37(4):327-33.
15. Ram J, Gupta A, Kumar S, Kaushik S, Gupta N, Severia S. Phacoemulsification with intraocular lens implantation in patients with uveitis. J Cataract Refract Surg. 2010; 36(8):1283-8.
16. Leder HA, Jabs DA, Galor A, Dunn JP, Thorne JE. Periocular triamcinolone acetonide injections for cystoid macular edema complicating noninfections uveitis. Am J Ophthalmol. 2011 Sep; 152(3):441-8.e2. doi: 10.1016/j.ajo.2011.02.009. Epub 2011 Jun 8.

Funding: No specific financial support was available for this study
CEP Approval: Not applicable
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
August 27, 2018.
Accepted on:
October 3, 2018.