Helena P Filipe1; Karl C Golnik2; Heather G Mack3
DOI: 10.17545/eoftalmo/2018.0007
ABSTRACT
This narrative review focuses on the conceptual learning cycle and covers the key practical aspects of reflecting on personal career development, deciding on the most appropriate learning experiences to undertake and self-assessment to successfully fill learning gaps. We a) describe the rationale behind the systematic learning cycle, b) explain a practical model of conducting an effective continuing professional development (CPD) plan under the physician perspective, c) summarize methods of gap analysis and needs assessment, learning methodologies, and assessment strategies suited to the physician educational practice. We conclude by expressing our own views on the topic within the broad frame of the CPD stakeholders' multiple perspectives.
Keywords: Continuing Medical Education; Assessment; Learning.
RESUMO
Esta revisão narrativa centra-se no conceito do ciclo de aprendizagem e aborda os principais aspectos práticos sobre o desenvolvimento da carreira profissional sugerindo as experiências de aprendizagem mais apropriadas para conduzir e autoavaliar com sucesso o preenchimento das lacunas de aprendizagem identificadas na prática clínica. No artigo apresentamos: a) a descrição do racional subjacente ao ciclo sistemático de aprendizagem, b) a explicação de um modelo prático para a condução de um plano de desenvolvimento profissional contínuo (DPC) sob a perspectiva do médico especialista, c) um resumo dos métodos analíticos de lacunas na prática clínica e da avaliação de necessidades, de metodologias de aprendizagem e de estratégias de avaliação mais apropriadas em educação médica contínua e desenvolvimento profissional. Concluímos expressando os nossos pontos de vista sobre o assunto no contexto das múltiplas perspectivas das várias partes interessadas no DPC.
Palavras-chave: Educação Médica Continuada; Avaliação; Aprendizagem.
RESUMEN
Esta revisión narrativa se centra en el concepto del ciclo de aprendizaje y aborda los principales aspectos prácticos sobre el desarrollo de la carrera profesional sugiriendo las experiencias de aprendizaje más apropiadas para conducir y autoevaluar con éxito el llenado de las lagunas de aprendizaje identificadas en la práctica clínica. En el artículo presentamos: a) la descripción del racional subyacente al ciclo sistemático de aprendizaje, b) la explicación de un modelo práctico para la conducción de un plan de desarrollo profesional continuo (DPC) desde la perspectiva del médico especialista, c) un resumen de los resultados métodos analíticos de lagunas en la práctica clínica y de la evaluación de necesidades, de metodologías de aprendizaje y de estrategias de evaluación más apropiadas en educación médica continua y desarrollo profesional. Concluimos expresando nuestros puntos de vista sobre el tema en el contexto de las múltiples perspectivas de las distintas partes interesadas en el DPC.
Palabras-clave: Educación Médica Continua; Evaluación; Aprendizaje.
INTRODUCTION
In times of medical knowledge explosion and rapid obsolescence, greater society scrutiny, increasing public demands on the medical profession, and heavy professional workload in complex healthcare systems, gauging the effectiveness of learning events has become central in continuing professional development (CPD). The learning cycle underpins undertaking CPD and attending CPD learning events. Demonstration of outcomes is key after participating in CPD activities. In this paper, we review the methods enabling the physician to achieve improved outcomes from CPD learning events, including 1) conducting a needs assessment based on learning gaps identified in practice, 2) creating effective goals and objectives to guide the personal learning plan, 3) matching the appropriate learning formats to bridge the desired outcomes and the learning needs previously identified, and 4) assessing the outcomes derived from the undertaken learning activities. These should effectively underpin on the personal development plan, which is anchored on the following three cyclic professional questions: What will I learn? How will I learn? and How well have I learned? This subject has been reviewed in general, but in this article, we focus on the needs of the learner rather than the CPD educator and extrapolate from a wider medical literature because there is minimal ophthalmology-specific literature. We use the term CPD throughout as the process of continuing education that is individualized for each ophthalmologist and aims to develop all the clinical and nonclinical competencies required by practicing ophthalmologists.
LEARNING CYCLE
CPD can be considered as a part of the continuum of medical education, arguably the most important phase, as it lasts the duration of one's professional career. After completing medical school and training in ophthalmology, CPD learners are adult learners and are expected to be proficient in reflection and self-directed lifelong learning, although this may not always be the case. CPD learners are expected to follow the principles of adult learning and be driven by 1) the need to know, 2) the learner's self-concept, 3) the role of the learners' experiences, 4) the readiness to learn, 5) the orientation to learning, and 6) motivation.6
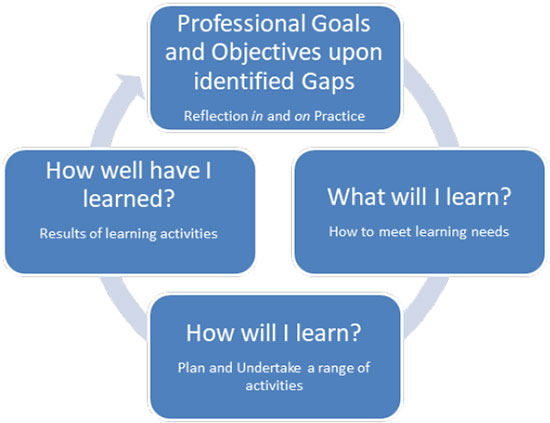
Adult learners follow the learning cycle (Figure 1). The learning cycle begins with setting individual goals derived from reflecting upon one's own current practice from which gaps can be identified, leading into a learning needs assessment going on with planning on how to meet learning needs. Appropriate CPD activities, either in format or in content, are then undertaken, and the outcomes from these activities should be assessed. A further cycle begins after reviewing the outcomes in relation to goals, and thus, repeated learning cycles occur during a professional career.
In the ophthalmic practice, physicians' goals should meet one's own healthcare organization, and systems needs and major stakeholders influence the goals of CPD. Medical regulators and professional ophthalmology societies, including the Conselho Federal de Medicina and the Brazilian Council of Ophthalmology, set standards for competent practicing ophthalmologists.
1) Conducting a needs assessment
In this step, physicians reflect upon their current practice compared with the ideal practice, identify the gaps, and perceive learning needs. Learning needs may as well be misperceived when the gap is not clearly recognized by the physician or even unperceived and become only apparent by external evaluation. Emerging learning needs associated with new techniques and concepts urge the physician to activate the personal development plan.
A needs assessment relies on the self-question What will I learn? Information can be obtained by selfassessment or from external sources of data. As mentioned above, self-assessment can be either an individualized process of self-reflection or via self-administered tests such as those provided by the American Academy of Ophthalmology and Internet sites such as Medscape. Unfortunately, reflective self-assessment by medical students and physicians is known to be inaccurate, with overinflated and underinflated assessments being common. The phenomenon of the most unaware individuals having the most overinflated self-assessment is recognized as the Kruger-Dunning effect. Medical students tend to begin with overinflated self-assessments, with gradual lowering to underassessment throughout their medical student years, and there is some evidence showing that medical school may worsen rather than improve the ability to self-assess by reflective practice.10
In this context, it is important to have external sources of information, and some of these are recorded in Table 1. There are limited data on the most effective sources of external data in conducting a needs assessment. Parboosingh surveyed CPD participants on their opinion of data sources most likely to change practice and found surgical audit and post hoc review of management of groups of patients to be judged as the most effective. In contrast, taking standardized tests and traditional continuing medical education (CME) activities were judged to be ineffective in changing practice and by implication in informing a needs analysis.
External sources of data are important in conducting a gap analysis, but not all data can be objectified. In addition, constantly emerging new information and computer-generated huge banks of data prompt the physician to continuously probe the environment and process, manage, and apply in practice new knowledge in accordance to customized needs. Physicians need to have an eye on the future and be prepared to undertake learning needs assessment relating to new technologies for diagnosis, new medications, innovative treatments, and regulatory changes, which may impact patient care.
Ophthalmologists should record needs analyses, as well as the results of their learning activities. A self-reflective portfolio is useful as it allows recording of needs analysis and subsequent learning activities. Reflection on results, analysis of one's learning style, and information about patient outcomes and health system needs can all be recorded in an individually designed portfolio. Concerns have been raised regarding the unintended use of documentation of reflective suboptimal performance, insecurities, or poor patient outcomes for legal purposes. The Academy of Medical Royal Colleges has thus written guidance on physicians' entering reflective notes into their individual e-portfolios.
2) Creating goals and objectives
In this stage, adult learners ideally plan and create a strategy and seek resources to achieve their learning goals. Rosenblum and Darkenwald found that participation in course planning by nurse supervisors did not improve learning outcomes. A recent study of rheumatologists undertaking self-assessment tests on Medscape demonstrated improved outcomes for those whose personalized program activities were geared by their tests' outcomes when compared with those following a self-directed learning plan disregarding that guidance.
We believe that by clearly defining their goals and objectives, physicians will assess more effectively the outcomes generated by undertaking learning experiences. Setting goals help to define the purpose to undertake a particular CPD program. Furthermore, defining objectives that are specific, measurable, attainable in realistic conditions, relevant to practice, and time-framed is tied to a more efficient outcome assessment with a rewarding sense of achievement, professional progression, and job satisfaction. The characteristics of learning objectives can be translated into the acronym SMART (specific, measurable, attainable, relevant, and time-framed). When recording the personal development plan in the self-reflective portfolio to demonstrate professional engagement and accountability, the physician should clearly document the individual goal and objectives leading to undertake a specific CPD program.
3) Matching delivery formats
In this stage, physicians act to undertake activities, which they have selected as most appropriate to fill their learning gaps. This requires understanding of the effectiveness of various CPD activities and the use of strategies to optimize learning and has been referenced in the American Accreditation Council for CME criterion 5 for CME activities.
Several studies demonstrate that traditional CME lectures can be ineffective learning experiences. Furthermore, Legaré et al. demonstrated that the vast majority of offered CPD activities do not target higher orders of thinking and instead focus on low levels of learning, as facts. Using the modified taxonomy of Bloom, it was shown that the offered activities are most often at level 1, rather than levels 5-7, where analysis and creation of new learnings occurs. These activities would not be expected to be capable of generating new competencies in ophthalmologists who undertake them.
While practicing, formal and unplanned learning experiences occur and should be valued. International bodies such as UEMS (Union Européenne des Medecins Spécialistes/European Union of Medical Specialists) through the EACCME (European Accreditation Council for Continuing Medical Education) have recognized learning through examining, peer reviewing, teaching, and e-learning as eligible for CPD activities. Healthcare systems technology (electronic health record) enables retrieval and analysis of patient data to inform shared decision-making with the patient. Available clinical data work as rich digital libraries always ready to provide directed information to be processed and applied.23
On the other hand, to substantiate facilitation of new learning for the practicing physician and justify formal CPD programs as effective learning experiences, increasing requirements have been set. The growing clinical workload and funding challenges have created an emphasis to develop cost-effective CPD programs. This demands CPD educators, who form the most diverse faculty group of all medical education stages, to have augmented teaching skills in applying the elements of the learning cycle.
The most effective CME learning experience is probably the clinical audit and feedback on professional behavior and patient outcomes. A Cochrane review found that audit and feedback are most effective when health professionals are not performing well to start out with; the person responsible for the audit and feedback is a supervisor or a colleague; it is provided more than once; it is given both verbally and in writing; and it includes clear targets and an action plan. The Cochrane review authors concluded that it is uncertain whether audit and feedback increase effectiveness when combined with other interventions.24 There is evidence indicating that CPD activities are most effective when they are undertaken over multiple occasions, with interactivity, and in different formats.9
Ophthalmologists often may not have the resources to undertake surgical audit of their practice. Instead, they must use available learning experiences to their best advantage, which typically involve planning and reflecting on learning. Table 2 lists typical CPD learning experiences and self-questions, which the ophthalmologist can ask prior to and during the learning experience, as well as recognized techniques, which participants may ask of educators to improve the quality of teaching.
4) Assessing effectively
The closing phase of the learning cycle is to assess the professional practice outcomes of having undertaken a specific learning experience. What behavior change does the physician recognize to have brought change in practice with consequent improved patient outcomes? What impact on the organization's performance does the physician identify as associated? Undertaking a learning experience can be justified by a self-confidence boost to practice an ongoing technique. New learning will be consolidated by reinforcement (practice) and dissemination (sharing with peers and coworkers) in further opportunities to be found in practice. By participating in interactive and longitudinal programs with feedback, physicians can build meaningful knowledge and skills to effectively translate into practice.9, 24
Don Moore has proposed a pyramidal framework for the assessment of continuing education, beginning with event participation (level 1) and concluding with assessment of community health outcomes (level 7) (Figure 2).

For accuracy and transparency purposes, physicians' self-assessment should be complemented with assessment of external evidence. The ideal outcomes for assessing CPD effectiveness are Moore's levels 6 and 7 relating to individual patient and society health outcomes. However, this relationship is difficult to demonstrate, and these levels are still seldom used in broad practice. Probably, the most pragmatic method of demonstrating the effectiveness of CPD activities is by observing performance change in practice. In ophthalmology, this strategy has been pursued at the postgraduate level by making use of either direct or video observation procedural skills and behavior. To our best knowledge, evidence on the use of such strategy in CPD is scarce though it is considered in ACGME criterion 30 as the best practice CME design to optimize technical and procedural skills of learners.
DISCUSSION AND CONCLUSION
After postgraduate training, and as a practicing specialist, medical education continues as a personalized CPD, targeting the individual's learning needs and aspirations while meeting the workplace and the regional community healthcare needs, within the necessary skills and attributes of the contemporary ophthalmologist. CPD learners are time-poor and need to optimize their time spent on CPD activities. Time is best spent according to the adult learning cycle, by systematically undertaking a gap analysis and needs assessment, deliberate planning for learning experiences to be undertaken, and assessing the effect of CPD activities on professional practice change. The learning cycle is anchored in the following three sequential questions: What will I learn? How will I learn? and How well have I learned? We can infer a dynamic framework in which going back in the cycle to rethink a more suited option within each step is possible to effectively progress and close the loop to start a new cycle.
Part of the ancient hidden social contract of medical profession is that physicians should maintain selfawareness of their knowledge and skill needs and address these by their lifelong learning commitment. We are confident that by recognizing this as an ongoing continuous process, physicians can, for example, demonstrate that medical profession effectiveness relies on continuing education and professional development. Society representatives, regulators, policymakers, employers, and administrators in leading positions should embrace leadership in promoting physician CPD, as essential to guarantee and improve the healthcare of communities.
REFERENCES
1. Filipe HP, Mack HG, Mayorga EP, Golnik KC, eds. ICO Guide to Effective CPD/CME [cited 2018 Mar 23]. Available from: www.icoph.org/ICO-CPD-CME.html
2. Filipe HP, Silva ED, Stulting AA, Golnik KC. Continuing professional development: Best practices. Middle East Afr J Ophthalmol 2014;21(2):134-41.
3. Frank JR, Snell L, Sherbino J, eds. CanMEDS 2015 Physician. Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
4. Nothnagle M, Anandarajah G, Goldman RE, Reis S. Struggling to be self-directed: residents' paradoxical beliefs about learning. Acad Med. 2011;86(12):1539-44.
5. Sockalingam S, Soklaridis S, Yufe S, Rawkins S, Harris I, Tekian A, et al. Incorporating Lifelong Learning From Residency to Practice: A Qualitative Study Exploring Psychiatry Learners' Needs and Motivations. J Contin Educ Health Prof. 2017;37(2):90-7. DOI: 10.1097/CEH.0000000000000156
6. Knowles MS, Holton EF III, Swanson RA. The Adult Learner. The Definitive Classic in Adult Education and Human Resource Development. 7th ed. Amsterdam: Elsevier; 2011.
7. Taylor DCM, Hamdy H. Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach. 2013;35(11):e1561-e1572. DOI: https://doi.org/10.3109/0142159X.2013.828153
8. University of Toronto, Faculty of Medicine, Continuing Professional Development. Quick Tips: Methods of Assessing Learning Needs. Ontario: University of Toronto; 2016.
9. Marinopoulos SS, Dorman T, Ratanawongsa N, Wilson LM, Ashar BH, Magaziner JL, et al. Effectiveness of continuing medical education. Evid Rep Technol Assess (Full Rep). 2007;(149):1-69.
10. Dunning D. Chapter five The Dunning-Kruger Effect: On Being Ignorant of One's Own Ignorance. Adv Exp Soc Psychol. 2011;44:247-96.
11. Parboosingh J. Role of self-assessment in identification of learning needs. J Contin Educ Health Prof. 1998;18(4):213-9.
12. Campbell C, Silver I, Sherbino J, Cate OT, Holmboe ES. Competency-based continuing professional development. Med Teach. 2010;32(8):657-62. DOI: 10.3109/0142159X.2010.500708
13. Nagler A, Andolsek K, Padmore JS. The unintended consequences of portfolios in graduate medical education. Acad Med. 2009;84(11):1522-6. DOI: 10.1097/ACM.0b013e3181bb2636
14. Academy of Medical Royal Colleges (AoMRC). New guidance on e-Portfolio reflective notes; 2016 [cited 2018 Mar 23]. Available from: https://www.themdu.com/guidance-and-advice/latest-updates-and-advice/new-guidance-on-e-portfolio-reflective-notes.
15. Rosenblum S, Darkenwald GG. Effects of Adult Learner Participation in Course Planning on Achievement and Satisfaction. Adult Educ Q (Am Assoc Adult Contin Educ). 1983;33(3):147-53.
16. Mehta N, Geissel K, Rhodes E, Salinas G. Comparative effectiveness in CME: evaluation of personalized and self-directed learning models. J Contin Educ Health Prof. 2015;35 Suppl 1: S24-6. DOI: 10.1002/chp.21284
17. Tasker F. How to prepare a personal development plan. BMJ Careers; 2015 [cited 2018 Mar 23]. Available from: http://careers.bmj.com/careers/advice/How_to_prepare_a_personal_development_plan
18. American Council for Accreditation of Continuing Medical Education (ACCME). Criterion 5 [cited 2018 Mar 23]. Available from: http://www.accme.org/requirements/accreditation-requirements-cme-providers/criteria/criterion-5
19. Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700-5.
20. Davis DA, O'Brien MA, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282(9):867-74.
21. Légaré F, Freitas A, Thompson-Leduc P, Borduas F, Luconi F, Boucher A, et al. The majority of accredited continuing professional development activities do not target clinical behavior change. Acad Med. 2015;90(2):197-202.
22. Anderson LW, Krathwohl DR, eds. A Taxonomy for Learning, Teaching, and Assessing: A Revision Of Bloom's Taxonomy of Educational Objectives. Boston: Allyn & Bacon; 2000.
23. Union Européenne des Mêdecins Spécialistes (UEMS). Continuing Medical Education & Professional Development. Brussels: UEMS; 2013 [cited 2018 Mar 23]. Available from: https://www.uems.eu/areas-of-expertise/cme-cpd
24. Institute of Medicine (US) Committee on Planning a Continuing Health Professional Education Institute. Redesigning Continuing Education in the Health Professions. Washington: National Academies Press (US); 2010.
25. Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(6):CD000259. DOI: 10.1002/14651858.CD000259.pub3
26. Davis D, Barnes B, Fox RD. Continuing Professional Development of Physicians: From Research to Practice. Chicago: American Medical Association Press; 2003. p. 249-74.
27. Grant J. The Good CPD Guide: A Practical Guide to Managed Continuing Professional Development in Medicine. 2nd ed. London: Radcliffe Publishing; 2011.
28. Moore DE Jr, Green JS, Gallis HA. Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. J Cont Educ Health Prof. 2009;29(1):1-15.
29. Stevenson R, Moore DE Je. Ascent to the Summit of the CME Pyramid. JAMA. 2018;319(6):543-4. DOI: 10.1001/jama.2017.19791
30. Golnik KC. Resident competence assessment: Best practices. J Curr Ophthalmol. 2016;28(2):53-4.
31. American Council for Accreditation of Continuing Medical Education (ACCME). Criterion 30 [cited 2018 Mar 23]. Available from: http://www.accme.org/requirements/accreditation-requirements-cme-providers/criteria/criterion-30
32. Schön DA. The Reflective Practioner: How Professionals Think in Action. New York: Basic Books; 1983.
33. Keister DM, Hansen SE, Dostal J. Teaching Resident Self-Assessment Through Triangulation of Faculty and Patient Feedback. Teach Learn Med. 2017;29(1):25-30. DOI: 10.1080/10401334.2016.1246249
34. Kim S, Dunkin BJ, Paige JT, Eggersted JM, Nicholas C, Vassilliou MC, et al. What is the future of training in surgery? Needs assessment of national stakeholders. Surgery. 2014;156(3):707-17.
35. Kjaer NK, Vedsted M, Høpner J. A new comprehensive model for Continuous Professional Development. Eur J Gen Pract. 2017;23(1):20-26. DOI: 10.1080/13814788.2016.1256998
36. Ellaway RH, O'Gorman L, Strasser R, Marsh DC, Graves L, Fink P, et al. A critical hybrid realist-outcomes systematic review of relationships between medical education programmes and communities: BEME Guide No. 35. Med Teach. 2016;38(3):229-45. DOI: 10.3109/0142159X.2015.1112894
37. Steinert Y, Snell LS. Interactive lecturing: strategies for increasing participation in large group presentations. Med Teach. 1999;21(1):37-42.
38. Sharma N, Lau CS, Doherty I, Harbutt D. How we flipped the medical classroom. Med Teach. 2015;37(4):327-30.
39. Jaques D. Teaching small groups. BMJ. 2003;326(7387):492-4.
Funding: No specific financial support was available for this study.
CEP Approval: Not applicable
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
March 20, 2018.
Accepted on:
May 11, 2018.