Carlos Augusto Moreira Jr1; Silvana Maria Pereira Vianello2; José A Cardillo3
DOI: 10.17545/e-oftalmo.cbo/2015.1
ABSTRACT
Herein we report a case of bilateral Valsalva retinopathy in a young woman following plastic surgery. Vision suddenly decreased to counting fingers in both eyes. The right eye (OD) underwent 25G three-port pars plana vitrectomy, and a good postoperative result was achieved (20/20). The left eye (OS) did not undergo surgery and was observed for 6 months; it showed the development of an epiretinal membrane with 20/40 vision. Such a result may suggest that early intervention may be indicated in cases of large hemorrhage over the macula.
Keywords: General Surgery. Eye. Retinal Diseases. Wounds. Injuries.
RESUMO
Este relato descreve um caso de retinopatia bilateral de Valsalva em uma mulher jovem após ser submetida à cirurgia plástica. A visão de ambos os olhos foi reduzida subitamente até ser possível apenas contar dedos. O olho direito (OD) foi submetido a uma vitrectomia via pars plana 25G com três portas, apresentando bom resultado pós-operatório (20/20). Ao contrário, o olho esquerdo (OS) não foi submetido à cirurgia e após ser observado por 6 meses, apresentou desenvolvimento de uma membrana epirretiniana com visão 20/40. O resultado sugere que a intervenção precoce pode ser indicada em casos de hemorragia intensa sobre a mácula.
Palavras-chave: Cirurgia Geral. Olho. Doenças Retinianas. Ferimentos. Lesões.
INTRODUCTION
Valsalva retinopathy is caused by a rapid increase in intraocular venous pressure, thereby leading to sudden visual loss due to premacular hemorrhage.1 It often occurs in young adults because a variety of causes such as intense exercise, heavy lifting, straining on the toilet, vomiting,2 coughing, labour,3 thoracoabdominal trauma,4 etc.
Treatment options include observation,5 puncturing of the posterior hyaloid face with a neodymium-doped yttrium aluminum garnet (Nd-YAG),6 pneumatic displacement of the hemorrhage by intravitreal injection of gas,7 and pars plana vitrectomy.8
The decision whether one should intervene or not depends on several factors, including bilaterality, size of the hemorrhage, need to regain good vision promptly, as well as surgical risks.
CASE REPORT
A 35-year-old Caucasian woman developed a bilateral premacular hemorrhage following lipoaspiration plastic surgery. The report of the anesthetist was that she was superficial at some point during surgery. Immediately after recovering from general anesthesia, she noticed a sudden decrease of vision in both eyes (OU). Her visual acuity (VA) at first examination was counting fingers (CF) in OU.
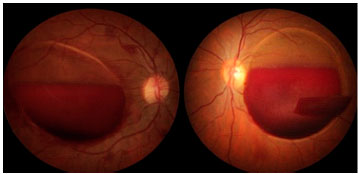
Fundus examination revealed bilateral pre-retinal hemorrhage over the macular area in both eyes (Figure 1). Because vision was reduced to CF, we decided to perform a 25G three-port pars plana vitrectomy in the right eye (OD). Following the removal of the core vitreous and posterior hyaloid, the internal limiting membrane (ILM) was removed and the hemorrhage was cleared. The sub-ILM localization of the hemorrhage was confirmed during surgery.
One week following vitrectomy, VA in the OD improved to 20/25 and remained unchanged during the follow-up period of 6 months (Figure 2).
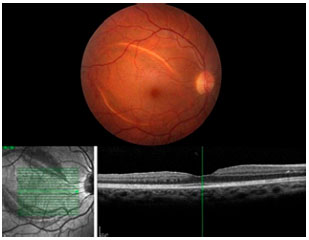
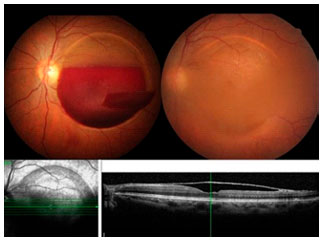
As the patient’s vision completely recovered in the OD, the patient decided to wait for spontaneous clearing of the hemorrhage in the left eye (OS). After 3 months, some clearing was already observed and vision improved to 20/60. OCT examination clearly demonstrated ILM displacement (Figure 3).
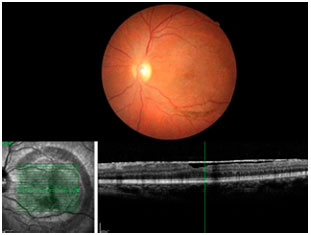
Six months after the hemorrhage, clearing was completed and a dense and translucent ILM with some pigment interiorly could be observed, covering the posterior pole of the OS (Figure 4). Vision was 20/40, and the patient was complaining about her OS vision. Surgery was scheduled for the OS.
REFERENCES
1 Fernandez MG, Navarro JC, Casta-o CG. Long-term evolution of Valsalva retinopathy: a case series. J Med Case Rep. 2012;6:346. http://dx.doi.org/10.1186/1752-1947-6-346.
2 Jayaprakasam A, Matthew R, Toma M, Soni M. Valsalva retinopathy in pregnancy: SD-OCT features during and after Nd:YAG laser hyaloidotomy. Ophthalmic Surg Lasers Imaging. 2011 ;17:42. http://dx.doi.org/10.3928/15428877-20110210-06.
3 Ladjimi A, Zaouali S, Messaoud R, Ben Yahia S, Attia S, Jenzri S, Khairallah M. Valsalva retinopathy induced by labour. Eur J Ophthalmol. 2002;12:336-338.
4 Azad R, Pal N, Sharma Y, Chhabra MS. Valsalva and Purtscher's retinopathy with optic neuropathy in compressive thoracic injury. Eye (Lond). 2005;19:914-915. http://dx.doi.org/10.1038/si.eve.6701665.
5 Lavezzo MM, Zacharias LC, Takahashi WY. Sub-internal limiting membrane hemorrhage in Valsalva retinopathy: case report. Arq Bras Oftalmol. 2012;75(6):436-8. http://dx.doi.org/10.1590/S0004-27492012000600015.
6 Kirwan RP, Cahill MT. Nd:YAG laser hyaloidotomy for Valsalva pre-macular haemorrhage. Ir J Med Sci. 2011 ;80:749-752. http://dx.doi.org/10.1007/s11845-009-0355-z.
7 Park SW, Seo MS. Subhyaloidhemorrhage treated with SF6 gas injection. Ophthalmic Surg Lasers Imaging. 2004;35:335-337.
8 De Maeyer K, Van Ginderdeuren R, Postelmans L, Stalmans P, Van Calster J. Sub-inner limiting membrane haemorrhage: causes and treatment with vitrectomy. Br J Ophthalmol. 2007;91:869-872. http://dx.doi.org/10.1136/bio.2006.109132.

VALSALVA RETINOPATHY
Silvana Maria Pereira Vianello
Universidade Federal de São Paulo - UNIFESP, Juiz de Fora, MG, Brasil, silvanampvianello@ia.com.br
The Valsalva retinopathy was described by Gass as a circumscribed bleeding under the internal limiting membrane in or near the central macular area. Part of the blood can become yellow after some days, and the spontaneous recovery of normal vision is usual.1 It may be associated with physical exertion in patients with tortuosity of the second and third order arterioles, as in familial retinal arteriolar tortuosity.1
There are no guidelines or consensus regarding the therapeutic options and the conditions of each case must be considered. It is also important to stress the need for discussing the available treatment options with the patient, explaining their advantages and disadvantages.
The treatment of Valsalva retinopathy can be expectant/conservative, membranectomy of hyaloid posterior with Nd:YAG laser, or pars plana vitrectomy. 2 The intravitreal gas injection associated with tissue plasminogen activating factor has also been described in a series of cases of submacular bleeding, showing functional improvement in over half of the cases. However, complications such as diffuse vitreous hemorrhage, cataract, and retinal detachment were described with a significant incidence.3
For therapeutic decision-making, the frame duration, location of bleeding, and amount of blood present should be considered,2 in addition to the need for rapid visual restoration in binocular cases.
Kuruvilla et al4 described a series of cases treated by posterior hyaloidotomy with Nd:YAG laser between 1.7 and 3.8 mJ to drain the bleeding. The initial visual acuity ranged from 20/400 to count fingers; after therapy, visual acuity reached from 20/20 to 20/30 in approximately 3 days. No significant changes were observed, other than the wrinkling of the internal limiting membrane over the macula.
Few side effects are reported with this type of YAG laser therapy compared with the natural course of the disease, which in rare instances, can evolve to pre-retinal fibrosis.5 However, for best results, this treatment should be performed as quickly as possible in order to prevent coagulation of the hematoma.6 Laser treatment can be a good alternative in cases of recent pre-retinal hemorrhages, with rapid visual rehabilitation, thus reducing the need for vitrectomy.3 This option appears to be safe and effective and has low cost. It could perhaps be an interesting option for treating one eye, as in the mentioned case, which presented bilateral bleeding.
Pars plana vitrectomy was also reported by other authors as efficient and safe, with the advantage of quick visual recovery, which is important in situations of intense bilateral visual impairment and massive and late bleeding. {TL 4.5 [EN] Missing citation (work not acknowledged)} Its disadvantages are its higher costs and the fact that it can evolve to secondary complications such as macular hole.7 Although the risks of surgical complications are low, these should be reported to the patient when this therapeutic option is chosen.
In summary, regarding the discussed case, the option of vitrectomy for the right eye was adequate because it achieved an excellent anatomical and functional outcome. The hyaloidotomy/posterior YAG laser membranotomy could have been an earlier therapeutic option for the left eye, shortening the course of visual recovery. Expectant/conservative treatment, which is also accepted for this condition, achieved a good final visual result, albeit with longer evolution.
Optical coherence tomography (OCT) of the left eye at 6 months revealed a partial detachment of the internal limiting membrane, with slightly modified foveolar depression, internal limiting membrane contraction in the nasal portion of the macula (evolving to the formation of the epiretinal membrane compared with the OCT of the same eye at 3 months), and no qualitative alterations in the outer retina. Considering these findings, the evolution of the condition within 3 months of follow-up, and the symptomatology, vitrectomy is a good therapeutic option for this eye in order to reduce visual alterations.
REFERENCES
1 Dugel PU, Win PH, Opber RR. Posterior segment manifestation of closed-globe contusion injury. In: Ryan SJ, editor. Retina. 4a ed. St. Louis: Elsevier; 2006. p. 2365-77.
2 Liu Z, Pan X, Bi H. Treatment of Valsalva Retinopathy. Optom Vis Sci. 2014;91 (11):e278-e282. http://dx.doi.org/10.1097/OPX.0000000000000400.
3 Ratanasukon M, Kittantong A. Results of intravitreal tissue plasminogen activator and expansile gas injection for submacular haemorrhage in Thais. Eye (Lond). 2005;19(12):1328-32. http://dx.doi.org/10.1038/si.eve.6701769.
4 Kuruvilla O, Munie M, Shah M, Desai U, Miller JA, Ober MD. Nd:YAG membranotomy for preretinal hemorrhage secondary to valsalva retinopathy. Saudi J Ophthalmol. 2014;28(2):145-51. http://dx.doi.org/10.1016/i.siopt.2014.02.006.
5 Kirwan RP, Cahill MT. Nd:YAG laser hyaloidotomy for valsalva pre-macular haemorrhage. Irish J Medical Sci. 2011 ;180(3):749-52. http://dx.doi.org/10.1007/s11845-009-0355-z.
6 Pollack AL, McDonald HR, Ai E, Johnson RN, Dugel PU, Folk J, et al. Massive suprachoroidal hemorrhage during pars plana vitrectomy associated with Valsalva maneuver. Am J Ophthalmol. 2001 ;132(3):383-7. http://dx.doi.org/10.1016/S0002-9394(01)01049-2.
7 Kim KY, Yu SY, Kim M, Kwak HW. Macular hole formation after pars plana vitrectomy for the treatment of Valsalva retinopathy: a case report. Korean J Ophthalmol. 2014;28(1):91-5. http://dx.doi.org/10.3341/kio.2014.28.1.91.

VALSALVA RETINOPATHY: MY PERSONAL CLINICAL ASSESSMENT AND GUIDELINES FOR AN OPTIMIZED TREATMENT APPROACH AND IMPROVED OUTCOME
Jose A Cardillo
Universidade Federal de São Paulo - UNIFESP - São Paulo, SP, Brasil, augustocardillo@me.com
Valsalva retinopathy classically presents as a sudden, painless loss of vision or central scotoma in a healthy individual caused by premacular hemorrhage secondary to Valsalva stress.1 The anatomic location of the premacular hemorrhage has been described as the sub-internal limiting membrane (ILM), the subhyaloid, or a combination of both. However, it is generally not possible to clinically distinguish between a subhyaloid and a sub-ILM hemorrhage. The plane of retinal hemorrhage in Valsalva retinopathy is sometimes difficult to determine, particularly in the absence of PVD. Ocular coherence tomography (OCT) has been used to determine the location when the vitreous medium is clear, and it is generally accepted that the location is sub-ILM.2 These preretinal structures are closely apposed to the retinal surface in young adults, although hemorrhages may dissect tissue planes and fill potential spaces. As a result, pathological analysis of the preretinal membrane after surgery is necessary to precisely identify it as the posterior hyaloid or ILM and to determine whether the hemorrhage is subhyaloid or beneath the ILM.
A precise clinical diagnosis is of key importance for any treatment approach, and it is necessary first to rule out other predisposing etiologies. Preretinal hemorrhage is associated with several other medical conditions such as diabetes mellitus, hypertension, sickle cell anemia, and other blood dyscrasias, including thrombocytopenia and leukemia. When the clinical diagnosis is unclear or retinopathy is recurrent, the following tests should be considered: complete blood count with differential, hemoglobin A1c, prothrombin time, partial thromboplastin time, sickle cell prep, hemoglobin electrophoresis, and peripheral smear. In addition to Valsalva retinopathy, the differential diagnoses that should be considered in such a case include:
1. Diabetic retinopathy
2. Hypertensive retinopathy
3. Sickle cell retinopathy
4. Radiation retinopathy
5. Posterior vitreous detachment
6. Terson’s syndrome
7. Purtscher’s retinopathy
8. Anemic retinopathy
POTENTIAL TREATMENTS
In general, no single treatment approach is acknowledged as the standard care of management; it may be considered that distinctive treatments are applicable based on the clinical presentation. Indeed, a comprehensive and detailed clinical-guided evaluation should always be conducted at presentation to individualize and customize the best possible treatment option.
In suspected or confirmed cases, regular follow-ups should be scheduled to closely monitor resolution or progression. In addition, yearly evaluations should be included to test for recurrence. It is important for clinicians to appreciate their role in educating patients about the natural course of this disease and instruct patients to avoid Valsalva maneuvers as well as anticoagulation drugs whenever possible.
Hemorrhages of less than one disk in diameter tend to resolve spontaneously over a short period of time and a conservative approach is generally justifiable. On the other hand, in patients with a large and dense hemorrhage, spontaneous reabsorption of the blood entrapped in the subhyaloid or sub-inner limiting membrane space may take months, potentially resulting in permanent visual impairment due to pigmentary macular changes, formation of epiretinal membranes, or toxic damage to the retina caused by prolonged contact with hemoglobin and iron; therefore, early intervention is recommended.3 As a result, different therapeutic options including conservative management, laser membranectomy, pneumatic displacement of the hemorrhage by an intravitreal injection of gas with or without recombinant tissue plasminogen activator, and pars plana vitrectomy should be considered.3,4,5 The best treatment option should be decided on an individual basis and may vary depending on hemorrhage extension, intra-retinal and posterior pole location, duration, and tendency of spontaneous resolution with no signs of progression or side effects.
If YAG laser membranectomy for non-clearing hemorrhage or for rapid improvement in vision is sought (monocular patient), it can accelerate visual recovery in patients with gross premacular and non-clearing hemorrhage, at the cost, however, of immediate and long-term complications such as retinal detachment, epiretinal membrane (ERM), and macular hole formation.6,7 Clinically, when the premacular hemorrhage is less than three discs in diameter or the blood is coagulated (generally 15 days following the onset) or is located very close to the retina or even under the ILM (in this case we should assume the possibility of blood localization errors even when using advanced retinal imaging techniques such as high resolution OCT), drainage with YAG laser is generally not recommended. In addition, in the long run, focal retinal pigment epithelium (RPE) cell proliferation, similar to that observed in proliferative vitreoretinopathy (PVR) epiretinal membranes, may occur within the neuroretina and specifically in a sub-ILM location by transmigrated RPE cells as a response to intraretinal haemorrhage.3 Such proliferation may prevent complete visual recovery after reabsorption of the retinal hemorrhage and justify early surgical intervention instead of routine observation or laser membranectomy.
In conclusion, except for early and spontaneous resolution cases showing no signs of progression or complication following a close and detailed functional and anatomical monitorization, we generally suggest an early intervention to avoid potential permanent visual impairment due to pigmentary macular changes, formation of epiretinal membranes, or toxic damage to the retina caused by the hemorrhage. Vitrectomy is our preferable interventional approach, which is considered more effective and potentially leads to a better outcome when compared with other treatment modalities in the management of patients with dense premacular hemorrhages and insufficient spontaneous reabsorption. However, surgery is not free of risks, and complications such as cataract or retinal breaks, as observed in one of our patients, may occur
REFERENCES
1 Duane TD. Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc 1972;70:298-313.
2 Shukla D, Naresh K B, Kim R. Optical coherence tomography findings in valsalva retinopathy. Am J Ophthalmol. 2005;140:134-136. http://dx.doi.org/10.1016/i.aio.2004.12.026.
3 De Maeyer K, Van Ginderdeuren R, Postelmans L, Stalmans P, Van Calster J. Sub-inner limiting membrane haemorrhage: causes and treatment with vitrectomy. Br J Ophthalmol 2007, 91:869-872. http://dx.doi.org/10.1136%2Fbio.2006.109132.
4 Park SW, Seo MS. Subhyaloidhemorrhage treated with SF6 gas injection. Ophthalmic Surg Lasers Imaging. 2004;35(4):335-337.
5 Mehdi N, Karkhaneh R, Mirshahi A, Lashay A, Harandi ZA, Roohipoor R, et al. Premacular hemorrhage in Valsalva retinopathy: a study of 21 cases. Iran J Ophthalmol. 2009;21:11-16.
6 Kwok AK, Lai TY, Chan NR. Epiretinal membrane formation with internal limiting membrane wrinkling after Nd:YAG laser membranotomy in valsalva retinopathy. Am J Ophthalmol. 2003 Oct;136(4):763-6. http://dx.doi.org/10.1016/S0002-9394(03)00442-2.
7 Tassignon MJ, Stempels N, Van Mulders L. Retrohyaloid premacular hemorrhage treated by Q-switched Nd-YAG laser. Graefes Arch Clin Exp Ophthalmol. 1989;227(5):440-2. http://dx.doi.org/10.1007/BF02172895.
Funding sources: none declared.
Conflict of interest: none declared.
Received on:
December 25, 2014.
Accepted on:
January 30, 2015.