André Luís Ayres da Fonsêca1; Fernanda Maria Silveira Souto2; Heitor Panetta3; Maurício Abujamra Nascimento4; Andrea Mara Simões Torigoe5
DOI: 10.17545/e-oftalmo.cbo/2016.75
ABSTRACT
Eales disease is an idiopathic peripheral vasculopathy involving the retina that primarily affects healthy young men. The clinical manifestations consist of three characteristic findings: peripheral retinal vasculitis, capillary nonperfusion, and neovascularization of the retina and the optic disc. Few case studies describe the rare form of central involvement in the disease, known as central Eales disease. In it, the typical findings of Eales disease occur in the posterior pole. Eales disease treatment depends on the clinical stage of the disease. Anti-VEGF therapy has recently been used. This report describes the case of a healthy young man with this rare form of Eales disease and the favorable outcome of intravitreal therapy with ranibizumab used in combination with panretinal photocoagulation. Satisfactory clinical improvement was observed in the eye that underwent intravitreal anti-VEGF treatment with ranibizumab, particularly in terms of the reduction in retinal thickness in the macular region and improvement in visual acuity.
Keywords: Retinal Vasculitis; Macular Edema; Ranibizumab
RESUMO
A doença de Eales é uma vasculopatia retiniana periférica idiopática que acomete principalmente homens jovens saudáveis. As manifestações clínicas consistem em três achados característicos: vasculite retiniana periférica, não perfusão capilar e neovascularização retiniana e de disco óptico. Em poucas séries de casos é descrita rara forma de acometimento central, doença de Eales Central. Nessa forma, os achados típicos da doença de Eales são encontrados no polo posterior. O tratamento da doença de Eales depende do estágio clínico em que se encontra a doença e mais recentemente realiza-se terapia com anti-VEGF. Neste relato descreve-se caso de jovem hígido portador da rara doença de Eales Central e resultado favorável da terapia intravítrea com ranibizumabe usada complementarmente à fotocoagulação panretiniana. Demonstrou-se evolução clínica satisfatória em olho submetido a terapia intravítrea de anti-VEGF ranibizumabe com redução da espessura retiniana em área macular e melhora da acuidade visual.
Palavras-chave: Ranibizumab; Edema Macular; Vasculite retiniana
INTRODUCTION
Eales disease consists of idiopathic peripheral vasculopathy involving the retina. It primarily affects healthy young men between the second and fourth decades of life1. Patients may be asymptomatic in the initial stages of the disease and may later have complaints, the most common of which is painless reduction in visual acuity (VA) and entopsia 1,2. Bilateralism is reported in approximately 50% to 90% of cases 3.
The three characteristic signs of Eales disease are peripheral retinal vasculitis, compromised vascular perfusion, and neovascularization of the retina; the fundoscopic findings vary depending on the clinical stage of the disease1,2,3,4,5,6.
A rare variant of Eales disease known as central Eales has been described in a few case studies 1,4. The central retina is affected and the typical signs of the disease are seen in the posterior pole, not in the most common site of presentation (the mid-periphery). Visual loss is intense and occurs at an early stage because of the presence of cystoid macular edema5,6,7.
The present report describes the case of a healthy young man who, after the exclusion of other causes of retinal vasculitis, was diagnosed with the central form of Eales disease and in whom the clinical improvement of the eye subjected to anti-VEGF intravitreal treatment with ranibizumab was satisfactory.
CASE REPORT
ARM, a 37-year-old man from the city of Mogi Guaçu (São Paulo) and who worked as a production assistant was referred to the emergency room of the Ophthalmology Department of the State University of Campinas complaining of progressive loss of visual acuity in both eyes for the two years prior to his visit, with significant deterioration in the left eye (LE) in the six months prior to his visit. He reported no previous history of personal or ocular problems and exhibited good overall health.
Examination of the eyes showed that the patient's corrected VA was 0.5 in the RE and 0.05 in the LE; the bio microscopy found no abnormalities; open chamber angle and no neovascularization were found in the gonioscopy; and tonometry revealed intraocular pressure (IOP) of 10 mmHg in both eyes.
Fundoscopy showed a clear and cell-free vitreous, microaneurysms, and dot-and-blot and flame retinal hemorrhages concentrated in the posterior pole and scattered throughout the mid-periphery and retinal periphery, as well as peripheral vascular dilatation, and marked vascular remodeling in the posterior pole (telangiectasias and shunts). The mid-periphery was found to have neovessels on the disc (NVD), diffuse macular edema in both eyes, and scattered laser marks.
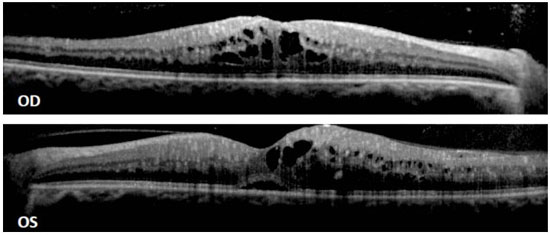
Spectralis® optical coherence tomography (OCT) showed flattening of the foveal depression in both eyes and hyporeflective intraretinal cysts in internal and external layers, sub retinal hyporeflective space in the left foveal region, macular thickness of 534 µm in the RE and of 457 µm in the LE (Figure 1).
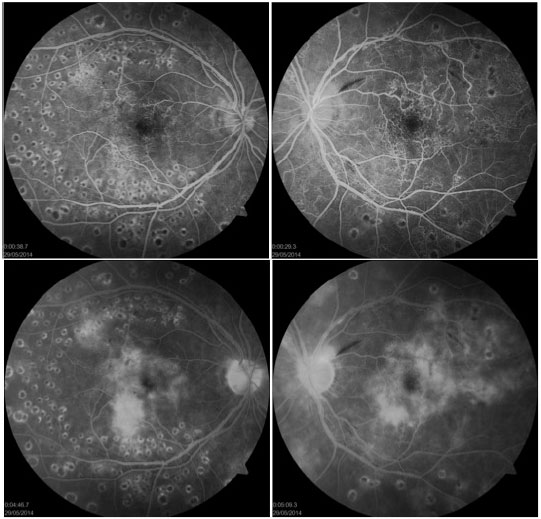
Visucam® fluorescein angiography showed diffuse peripheral vascular insufficiency in both eyes in the four quadrants associated with multifocal areas of capillary nonperfusion, as well as the presence of arteriovenous shunts in the posterior pole and mid-periphery, NVD that did not go further than the papilla, increased avascular zone of the fovea, and late diffuse edema in the macular region (Figure 2).
Complementation with bilateral panretinal photocoagulation was performed, and the following tests were conducted to confirm the diagnosis: serology for hepatitis A, B and C, cytomegalovirus, toxoplasmosis, syphilis, HIV and rubella, FAN, ENA-6, anti-DNA, FR, anti-CCP3, P-ANCA and C-ANCA antibodies, sputum bacilloscopy, anti-anticardiolipin antibody and lupus anticoagulant (all with negative results), fasting blood glucose, glycated hemoglobin, hemoglobin electrophoresis, homocysteine, PPD. In addition, the results of the Doppler ultrasound of the carotid and vertebral arteries was normal. Otolaryngology, gastroenterology, rheumatology, hematology, pulmonology, and neurology exams ruled out systemic obliterative vascular disease, thrombophilia, and sarcoidosis.
Intravitreal treatment with 0.5 mg of ranibizumab in both eyes was initiated, which consisted of three monthly administrations, and monitoring was pro re nata (PRN).
After the second intravitreal injection, the patient exhibited VA of 0.5 in the RE and light perception in the LE. Fundoscopy revealed reduced intraretinal hemorrhages, dry macula in the RE, and regression of the NVD in both eyes. Because low VA persisted in the LE as a result of inflammatory damage to the optical nerve and retinal ischemia (as shown in the full-field electroretinogram), as well as evoked visual potential, the patient chose to stop the intravitreal treatment in the LE.
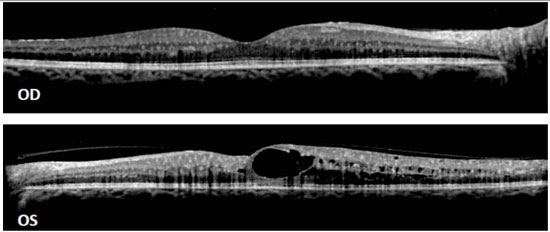
One month after the third intravitreal injection, the patient exhibited VA of 0.4 in the RE and hand movement in the LE. Fundoscopy findings were similar to those described after the second injection, and OCT of the RE revealed restored foveal depression, absence of intraretinal hyporeflective cysts, sponge-like diffuse retinal thickening, and a macular thickness of 415 µm (Figure 3).
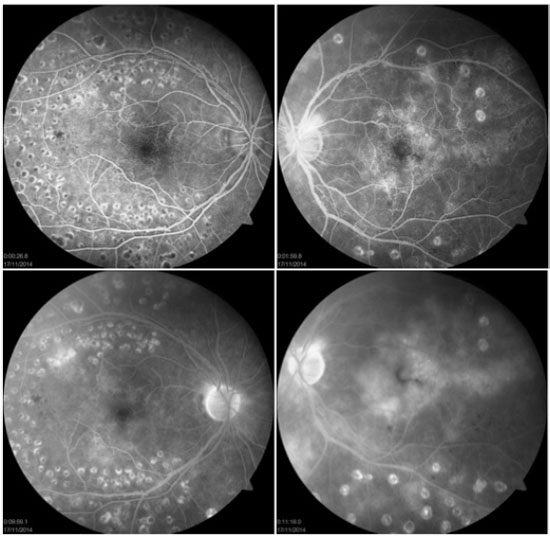
After three more injections of ranibizumab (0.5 mg) and PRN monitoring, the patient exhibited VA of 0.4 in the RE and hand movement in the LE. The macula of the RE remained dry, and the tomography findings remained stable, with a macular thickness of 375 µm. Fluorescein angiography findings showed an improvement in the pattern of peripheral vascular insufficiency in the RE, maintenance of multifocal areas of capillary nonperfusion and numerous arteriovenous shunts in the LE, and late leakage that was discrete in the macular region of the RE and accentuated in the LE (Figure 4).
The patient is currently being monitored in the Retina and Vitreous Sector of the Ophthalmology Department of the Clinical Hospital of the State University of Campinas (HC-UNICAMP), and his VA has been maintained through intravitreal anti-VEGF treatment with ranibizumab 0.5 mg.
DISCUSSION
The etiopathogenesis of Eales disease remains poorly understood1,2,3,4. It has been suggested that immune-mediated mechanisms combined with inflammation and venous and arterial occlusion participate in the pathophysiology of the disease. Associations with systemic diseases such as tuberculosis, systemic sclerosis, auditory-vestibular dysfunction, and blood coagulation disorders have been proposed, but they have never been definitively confirmed1,4.
The diagnosis of Eales disease is a diagnosis of exclusion. Retinal vasculitis, caused by diseases such as leukemia, sarcoidosis, syphilis, systemic lupus erythematosus, toxoplasmosis, tuberculosis, Behçet's disease, should be excluded, as should proliferative vascular retinopathies (such as diabetes mellitus, sickle cell anemia, retinal venous vascular occlusions) that mimic the condition2,4,5.
The clinical case presented herein differs from the typical peripheral presentation of retinal changes, because the central region was the main area affected. It is therefore a case of the rare variant described as central Eales disaese2,4. Macular involvement is an uncommon finding; it is observed in approximately 18% of affected eyes2,4.
The treatment of Eales disease seeks to reduce vasculitis, minimize the risk of vitreous hemorrhage and, in more advanced cases, surgically remove persistent vitreous hemorrhages and vitreoretinal tractions4,7,8,9. In the inflammatory stage with active vasculitis, treatment involves the use of periocular and oral corticosteroids and, in select cases, intravenous and intravitreal corticosteroids. Panretinal photocoagulation is the gold standard treatment in the proliferative stage. Regression of retinal neovascularization has been observed in 89% of cases after adequate laser treatment8,9. Vitreoretinal surgery is indicated in cases of persistent vitreous hemorrhage, tractional retinal detachment involving the posterior pole, and combined tractional and rhegmatogenous retinal detachment 1,4,7,8,9.
Anti-VEGF therapy has been established as an alternative treatment for Eales disease because of the proven association between VEGF expression and neovascular proliferation observed in this disaese1,6,8. Thus, intravitreal therapy with anti-VEGF complements panretinal photocoagulation or vitreoretinal surgery, depending on the clinical stage of the disease 1,6,8. In addition, other studies have found it to be effective in reducing macular thickness in cases of macular edema, thereby significantly improving VA 10. This finding is consistent with the result obtained in the case reported herein.
In this report of a patient with central Eales disease, the eye that was subjected to intravitreal anti-VEGF treatment with ranibizumab had a satisfactory clinical outcome. The macular retinal architecture was relatively preserved, as shown by OCT, and there were differences in retinal vascular perfusion and in the pattern of central vascular leakage, as shown by fluorescein angiography.
Visual prognosis in Eales disease depends on the early and adequate administration of the treatment that is most appropriate for the clinical stage of the disease1,4,7. Macular involvement, which is observed in cases of central Eales disease, is an important cause of compromised final VA 4,6,7.
REFERENCES
1. Eales H. Retinal haemorrhage associated with epistaxis and constipation. Birmingham: Hall and Englis; 1980
2. Das T, Pathengay A, Hussain N, Biswas J. Eales' disease: diagnosis and management. Eye. 2010;24(3):472-82. http://dx.doi.org/10.1038/eye.2009.315
3. Davis J, Schecter SH, Sowka J. Eales' disease: the great masquerader. Optometry. 2009;80(7):354-9. http://dx.doi.org/10.10167j.optm.2008.10.016
4. Biswas J, Sharma T, Gopal L, Madhavan HN, Sulochana KN, Ramakrishnan S. Eales disease: an update. Surv Ophthalmol. 2002;47(3):197-214. http://dx.doi.org/10.1016/S0039-6257(02)00288-6
5. Das T, Biswas J, Kumar A, Nagpal PN, Namperumalsamy P, Patnaik B, et al. Eales disease. Indian J Ophthalmol. 1994;42(1):3-18. Disponível em: http://www.ijo.in/text.asp?1994/42/1/3/25586
6. Agarwal R, Biswas J. Macular involvement in eales disease. Am Acad Ophthalmol New Orleans. 1998;118
7. Saxena S, Kumar D. New classification system-based visual outcome in Eales' disease. Indian J Ophthalmol. 2007;55(4):267-9. Disponível em: http://www.ijo.in/text.asp?2007/55/4/267/33038
8. Juarez CP, Gramajo AL, Luna JD. Combination of intravitreal bevacizumab and peripheral photocoagulation: an alternative treatment in eales disease. Med Hypothesis Discov Innov Ophthalmol. 2013;2(2):30-3. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3939753/
9. El-Asrar AMA, Al-Kharashi SA. Full panretinal photocoagulation and early vitrectomy improve prognosis of retinal vasculitis associated with tuberculoprotein hypersensitivity (Eales' disease). Br J Ophthalmol. 2002;86(11):1248-51. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1771369/
10. Gupta SR, Flaxel CJ. The use of a vascular endothelial growth factor inhibitor (ranibizumab) in macular edema due to eales disease. Retin Cases Brief Rep. 2012;6(1): 122-4. http://dx.doi.org/10.1097/ICB.0b013e31821608e8




Funding source: None
Conflicts of interest: None
Received on:
December 1, 2016.
Accepted on:
December 9, 2016.