Luiza Maretti Scomparin1; Andrea Mara Simões Torigoe1; Albina Messias de Almeida Milani Altemani2; Isabela Mazzo Miorim1; Ludmyla Kandratavicius2; Lucas Yunes Cominatto Barbosa3
DOI: 10.17545/eOftalmo/2024.0021
ABSTRACT
Mesectodermal leiomyoma of the ciliary body is a rare benign tumor, often mistaken for melanoma and usually diagnosed after enucleation and histopathological analysis. We report the case of a patient with rapid and aggressive progression of a tumor in the right eye, initially suspected as malignant, which culminated in enucleation. In addition, a congenital, non-progressive hamartoma of the retinal pigment epithelium was detected in the macula of the contralateral eye, which was benign but caused vision impairment. This report describes the association of two rare diagnoses that has not been previously reported.
Keywords: Leiomyoma; Hamartoma; Mesectodermal leiomyoma; Retinal pigment epithelium hamartoma; Simple hamartoma.
RESUMO
O leiomioma mesectodérmico do corpo ciliar é um tumor benigno raro, frequentemente confundido com melanoma e geralmente diagnosticado após enucleação e análise histopatológica. Relatamos o caso de um paciente com progressão rápida e agressiva de um tumor no olho direito, inicialmente suspeito de malignidade, que culminou em enucleação. Adicionalmente, foi identificado um hamartoma congênito e não progressivo de epitélio pigmentar da retina na mácula do olho contralateral, de caráter benigno mas com comprometimento visual. Este relato reúne dois diagnósticos raros e previamente não descritos em associação.
Palavras-chave: Leiomioma; Hamartoma; Leiomioma mesectodérmico; Hamartoma de EPR; Hamartoma simples.
INTRODUCTION
Rare benign tumors of the eye pose significant diagnostic challenges due to their low prevalence and characteristics that often mimic malignant lesions. They include mesectodermal leiomyoma of the ciliary body and simple hamartoma of the retinal pigment epithelium (RPE), which are both are scarcely described in the literature.
Mesectodermal leiomyoma of the ciliary body is an uncommon benign tumor, with only around 30 cases documented in the last five decades1. It was first described in 1977 by Jakobiec et al.2. Its main distinguishing feature is the combination of neurogenic and myogenic elements, suggesting an origin in the neural crest1-4. Studies indicate that this tumor is more prevalent among women of childbearing age, often presenting with symptoms, such as blurred vision and preserved visual acuity above 20/2001,5.
Simple RPE hamartoma is a rare benign lesion, first described in 1981 and further explained in 19896. It is located between the choriocapillaris vessels and photoreceptors in the outer retina7 and appears as a dark lesion in the macular region. This tumor is congenital, non-progressive, and has limited visual impact8.
Below, we present an unprecedented case report that illustrates the coexistence of these two rare tumor findings in contralateral eyes, with the aim of contributing to an understanding of their clinical presentation and management.
This case report was approved by the ethics committee and published with the patient’s consent. This is a retrospective report based on data obtained from medical records.
CASE REPORT
A 26-year-old male from Campinas-SP came to the Ophthalmology Emergency Department at Hospital de Clínicas of Unicamp complaining of low visual acuity in right eye for six days, accompanied by the perception of a dark spot in the superior temporal visual field and floaters. He denied pain, hyperemia, or other ocular symptoms. He reported a history of myopia corrected with glasses and worse visual acuity in the left eye since childhood, without previous investigation.
On ophthalmological examination, visual acuity was finger counting at 4 meters in right eye and 20/200 in left eye. Anterior and posterior examination of right eye showed a large brownish expansive mass with a whitish halo in the lower nasal region near the ora serrata, associated with retinal detachment (Figure 1). In left eye, there was an elevated, brownish macular lesion with no exudation and the retina was attached (Figure 2).
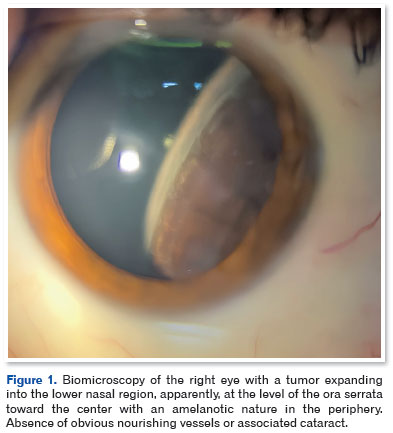
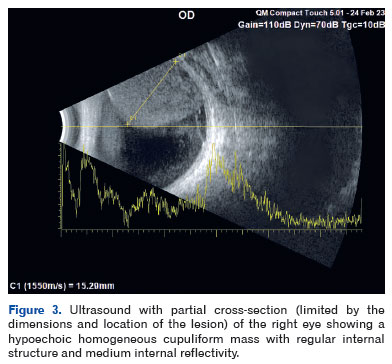
In view of these findings, the initial hypothesis was ciliary body melanoma in right eye and an unrelated congenital lesion in left eye, prompting further tests. Ultrasound (US) of right eye showed a hypoechoic cupuliform mass measuring 15.3 × 18.7 mm that was homogeneous and had medium internal reflectivity and no angle kappa (Figure 3). In left eye, US showed a hyperechogenic flat lesion measuring 1.1 × 1.3 mm. Optical coherence tomography (OCT) of left eye showed focal elevation of RPE with posterior shadowing (Figure 4), whereas OCT angiography (OCT-A) showed anomalous superficial vascularization, without deep vessels or signs of ischemia, compatible with simple RPE hamartoma (Figure 5).
Magnetic resonance imaging (MRI) of the orbits confirmed an expansive lesion in the posterior segment of right eye, with iso-signal on T1 and hypo-signal on T2, with no visible extraocular infiltration (Figure 6). Systemic and laboratory tests ruled out metastases or systemic abnormalities. Due to rapid progression of the lesion and lack of prognosis for vision, a decision was made to enucleate right eye.
Pathology showed a mesectodermal leiomyoma of the ciliary body, measuring 1.8 × 1.7 × 1.4 cm, with free margins and retinal detachment secondary to the neoplasm. Immunohistochemical profile confirmed the mesectodermal origin, with positivity for 1A4, calponin, CD56, and vimentin, and negativity for S100, which allowed ruling out the initial suspicion of uveal melanoma (Figure 7 and Table 1). After a year’s follow-up, the lesion in left eye remained stable, with no signs of progression.
DISCUSSION
We present an unprecedented case of the coexistence of two benign hamartomas in contralateral eyes: a mesectodermal leiomyoma of the ciliary body and a simple RPE hamartoma.
Mesectodermal leiomyoma of the ciliary body is a rare benign tumor of the eye derived from smooth muscle, histologically characterized by uniform spindle cells, elongated nuclei, eosinophilic cytoplasm, and absence of cellular atypia or significant mitotic activity1-3. Despite being a benign tumor, it can grow and occupy intraocular space, resulting in the compression of adjacent structures and progressive visual loss1. The clinical presentation, which is more common in women, occurs at the average age of 35.8 years but can occur from the age of 8 to 80 years9. In the early stages, the tumor may be asymptomatic but as it grows the symptoms include low vision, eye pain, diplopia, and inflammation.
Differential diagnosis is challenging, including other ciliary body masses, such as melanoma, nevus, adenoma, and epithelial adenocarcinoma1. In the case reported herein, US and MRI of the eye were fundamental in characterizing the extent and location of the lesion. The imaging characteristics, such as the absence of angle kappa on US and iso-signal on T1-weighted MRI, were not typical of melanoma. However, due to the rapid growth, severe visual impairment, and lack of effective therapeutic alternatives, enucleation was the chosen treatment.
Immunohistochemical profile confirmed the diagnosis of mesectodermal leiomyoma, with positivity for smooth muscle markers (1A4, calponin, and vimentin) and negativity for malignancy markers such as S-100 and HMB-4510-12. The prognosis for this tumor is excellent, with a low risk of recurrence after complete excision. However, regular monitoring is essential in conservatively managed cases to assess growth and preserve visual function.
However, simple RPE hamartoma is a rare congenital malformation consisting of normal RPE cells organized in an anomalous way, without atypia or mitotic activity7,8. Clinically, the lesion presents as a focal, flat, or slightly raised pigmented area located at the posterior pole. It is usually asymptomatic and is detected incidentally during eye examinations. In the case reported herein, the lesion was diagnosed via multimodal exams, such as OCT and OCT-A, which showed focal elevation of RPE and anomalous superficial vascularization.
The differential diagnosis of hamartoma includes chorioretinal nevus, melanocytoma, and choroidal melanoma. Although most cases only require regular monitoring, complications such as macular edema or retinal detachment can occur. Interventions are rarely necessary, except in cases of significant visual impairment.
From an embryological point of view, mesectodermal leiomyoma is believed to originate in the neural crest, whereas RPE hamartoma derives from ectopic progenitor cells with incomplete differentiation during embryonic development13. There is no evidence of a direct relationship between these lesions, and this is the first case of this association described in the literature.
This report highlights the importance of accurate diagnosis, multidisciplinary management, and regular follow-up in cases of rare tumors of the eye and contributes to the understanding of these lesions and their clinical implications.
REFERENCES
1. Kim JM, Hall LB, Elia M, Ehrlich MS, Materin MA, Sinard JH. Acute Presentation of Mesectodermal Leiomyoma of the Ciliary Body. Ocul Oncol Pathol. 2017 Nov;3(4):304-309.
2. Jakobiec FA, Font RL, Tso MOM, Zimmerman LE. Mesectodermal leiomyoma of the ciliary body. A tumor of presumed neural crest origin. Cancer. 1977;39(5): 2102-2113.
3. Jakobiec FA, Iwamoto T. Mesectodermal Leiomyoma of the Ciliary Body Associated With a Nevus. Arch Ophthalmol. 1978;96(4):692–695.
4. Inamori O, Fukuoka H, Nagamine M, Sotozono C, Konishi E. Mesectodermal Leiomyoma of the Ciliary Body: A Unique Variant of Leiomyoma with Myogenic and Neurogenic Histological Features. Int J Surg Pathol. 2022;30(1):114-119.
5. Alenda C, Aranda FI, Paya A, Cordoba C. Mesectodermal Leiomyoma of Ciliary Body. International Journal of Surgical Pathology. 2002;10(4):309-312.
6. Gass JD. Focal congenital anomalies of the retinal pigment epithelium. Eye (Lond) 1989;3 (Pt 1):1–18.
7. Baba K, Goyal V, Tosini G. Circadian Regulation of Retinal Pigment Epithelium Function. Int J Mol Sci. 2022;23(5):2699.
8. Shields CL, Shields JA, Marr BP, Sperber DE, Gass JD. Congenital simple hamartoma of the retinal pigment epithelium: a study of five cases. Ophthalmology. 2003;110(5):1005-11.
9. Tomar AS, Finger PT, Iacob CE. Intraocular leiomyoma: Current concepts. Surv Ophthalmol. 2020;65(4):421-437.
10. Koletsa T, Karayannopoulou G, Dereklis D, Vasileiadis I, Papadimitriou CS, Hytiroglou P. Mesectodermal leiomyoma of the ciliary body: report of a case and review of the literature. Pathol Res Pract. 2009;205(2):125-30.
11. Park SH, Lee JH, Chae YS, Kim CH. Recurrent mesectodermal leiomyoma of the ciliary body: a case report. J Korean Med Sci. 2003;18(4):614-7.
12. Lai CT, Tai MC, Liang CM, Lee HS. Unusual uveal tract tumor: mesectodermal leiomyoma of the ciliary body. Pathol Int. 2004;54(5):337-42.
13. Pujari A, Agarwal D, Chawla R, Todi V, Kumar A. Congenital simple hamartoma of the retinal pigment epithelium: What is the probable cause? Med Hypotheses. 2019 Feb:123:79-80.
| AUTHORS INFORMATIONS |
|
 |
» Luiza Maretti Scomparin |
 |
» Andrea Mara Simões Torigoe |
 |
» Albina Messias de Almeida Milani Altemani |
 |
» Isabela Mazzo Miorim |
 |
» Ludmyla Kandratavicius |
 |
» Lucas Yunes Cominatto Barbosa |
Funding: The authors declare no funding.
Ethics Committee approval: State University of Campinas - UNICAMP (CAAE: 74089623.7.0000.5404).
Conflicts of interest: The authors declare no funding.
Received on:
September 23, 2024.
Accepted on:
February 23, 2025.