Dillan Cunha Amaral1; Guilherme da Silva Ferreira da Costa1; Márcio Penha Morterá Rodrigues1; Adroaldo Alencar Costa Filho1; Milton Ruiz Alves2; Ricardo Noguera Louzada1, 2
DOI: 10.17545/eOftalmo/2023.0049
ABSTRACT
Solar maculopathy is a retinal disorder caused by intense and unprotected observation of a solar eclipse, but it can also occur after direct and prolonged observation of the sun. Despite exposure factors, individual susceptibility plays an important role and may vary between individuals. This report describes the case of a 22-year-old man complaining of cloudiness with decreased visual acuity in the left eye associated with burns on the body due to prolonged solar exposure and sought ophthalmologic care. Ophthalmologic evaluation showed a yellowish color in the left eye's fovea, and the patient underwent multimodal imaging tests. During regular ophthalmologic follow-up, the patient showed improvement in visual acuity after six months, but without complete recovery. A detailed clinical history and correlation with ophthalmologic findings are important for accurate diagnosis, and there is a need for awareness of the risks of intense sun exposure and eye protection measures.
Keywords: Eye; Retina; Solar radiation; Macular degeneration; Retinal disorders.
RESUMO
A maculopatia solar é uma desordem retiniana causada pela observação intensa e desprotegida de um eclipse solar, mas também pode ocorrer após a observação direta ao sol. Apesar dos fatores de exposição, a suscetibilidade individual desempenha um papel importante, podendo variar entre os indivíduos. O relato descreve um paciente masculino de 22 anos que procurou atendimento oftalmológico com queixa de turvação com diminuição da acuidade visual no olho esquerdo associada a queimaduras pelo corpo por exposição solar prolongada. Na avaliação oftalmológica, o exame evidenciou uma coloração amarelada na fóvea do olho esquerdo e o paciente foi submetido aos exames de imagem multimodal. O paciente durante o acompanhamento oftalmológico regular apresentou melhora da acuidade visual após seis meses, porém, sem recuperação completa. A história clínica detalhada e a correlação com achados oftalmológicos são importantes para um diagnóstico preciso e há necessidade de conscientização sobre os riscos da exposição solar intensa e medidas de proteção ocular.
Palavras-chave: Olho; Retina; Radiação solar; Degeneração macular; Doenças retinianas.
INTRODUCTION
Solar maculopathy (SM) is defined as a retinal disorder that occurs due to increased, intense, and unprotected exposure of the retina to solar radiation. This exposure is known to induce several adverse health effects, mainly related to its ultraviolet (UV) component.
It is important to emphasize that, despite exposure factors, an individual susceptibility's to radiation plays an important role, and the threshold for injury is likely to be different between individuals1. Currently, we know that most cases occur in young men with emmetropia, as their eye lens is more transparent and has greater ability to focus light on the retina. Additionally, climatic factors can increase the risk of exposure to UV radiation.
CASE REPORT
A 22-year-old man sought ophthalmologic care at the Clementino Fraga Filho University Hospital, Federal University of Rio de Janeiro, Brazil, with a history of visual blurring in the left eye (OS) since about 3 days before, after spending the whole day at a swimming pool, reporting intense sun exposure associated with extensive burns on the body, but no other ocular symptoms.
Ophthalmologic examination showed corrected visual acuity (VA) of 20/20, Jaeger score J1 in the right eye (OD) and 20/40 J2 in OS. Biomicroscopy of the anterior segment showed findings within normal parameters, and intraocular pressure was 10 mmHg in both eyes. Pupillary and ocular motility reflexes were normal in both eyes. On fundoscopic examination, regular optic discs with normal coloration were found, along with retinal vasculatures without alterations, but with asymmetry in macular brightness. In OS, a yellowish-white lesion with a diameter smaller than one optic disc was observed in the foveolar region. The vitreous was transparent in both eyes (OU), with no evidence of vitreitis.
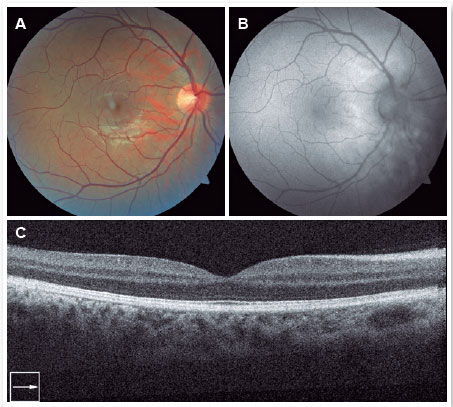
The patient underwent complementary tests. Retinography was normal in OD (Figure 1A), but in OS showed a yellowish lesion in the foveal region of the macula, surrounded by a hyperpigmented edge (Figure 2A). Fundus autofluorescence (FAF; Figure 1B) and spectral-domain optical coherence tomography (SD-OCT; Figure 1C) showed no changes in OD. In OS, FAF identified a hypoautofluorescent foveal lesion (Figure 2B, yellow arrow) corresponding to a characteristic retinal hole that appeared as a hyporeflective square with straight edges (Figure 2C, yellow arrow).
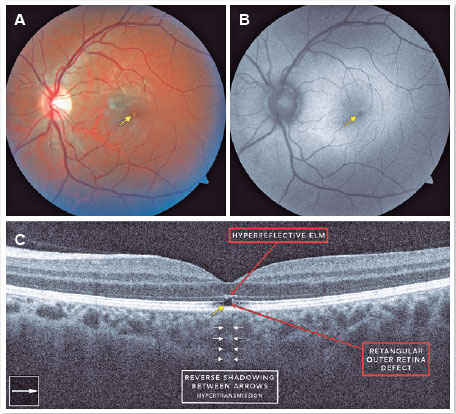
This hole corresponded to a subfoveal rupture extending from the retinal pigment epithelium (RPE) to the external limiting membrane (ELM). A hyperreflective change with discontinuation of the adjacent ellipsoid zone was also observed on SD-OCT, along with a reverse shadow due to choroidal hypertransmission (Figure 2C), which occurred due to increased light transmission beneath the RPE/Bruch membrane complex through the hole2-4.
In view of these findings, the diagnostic hypothesis of unilateral SM in OS was considered, and expectant ophthalmological follow-up was advised. Vision in OS improved gradually and reached a corrected VA of 20/30 J2 after 6 months.
This report demonstrates the importance of properly collecting patients' clinical history and associating it with the ophthalmic findings, ensuring accurate diagnosis.
DISCUSSION
This is the case report of a patient with direct exposure and a clearly recorded long stay under the sun who presented reduced VA in OS, with multimodal retinography and OCT imaging compatible with SM findings. Since there is no specific treatment, it was decided to follow him up clinically, and there was a slight improvement in VA, but still had a deficit in the affected eye. The patient continues to be followed up and maintains the vision and fundoscopic findings. Contrary to what would be expected, the involvement was unilateral. UV light is harmful to photoreceptors as well as to the RPE, and can induce damage by photochemical, photomechanical, and photothermal mechanisms, with the photochemical mechanism causing the most substantial retinal damage1,5. UV radiation causes chemical damage by various mechanisms, one of them being the production of free radicals and oxygen-dependent toxicity. Conversely, lipofuscin, found in the RPE, is highly photoreactive, which increases the toxicity1. The outer layers of the central retina are more sensitive to this damage. Thus, there are several types of mechanisms of UV-induced retinal lesions, but RPE cell disruption and damage to the outer segments of photoreceptors are the evident morphological findings1.
Due to the generally high solar exposure of the population, tracing the prevalence of SM is notoriously difficult, since it is difficult to measure the duration of this exposure. Commonly, affected people only notice visual changes after the injury, which makes the prognosis difficult.
The direct observation of solar eclipses increases the risk of SM due to intense exposure to UV rays. Because these events are rare and attract the attention of many people, they can increase the number of cases of eye damage. There are other circumstances that can significantly influence the probability and severity of cases, such as the angle of solar elevation and the type of eclipse, which can be total or partial.
In addition, cases of SM in certain groups are associated with greater direct exposure to the sun for long periods, such as in religious ceremonies or in users of drugs with mydriatic effects that cause the retina to be more exposed to light, thereby increasing the chances of injury. Contrarily, some sports and professional practices present a greater risk, as in the case of swimmers, military personnel, and climbers1.
From a clinical standpoint, prolonged exposure to UV radiation can lead to symptoms such as headache, blurred vision, achromatopsia, metamorphopsia, and central or paracentral scotomas1. In SM, VA usually varies between 20/30 and 20/60, and most patients have asymmetrical bilateral involvement, usually affecting the dominant eye1.
If there is significant visual loss, patients usually seek an ophthalmologist. Conversely, those with mild impairment seek medical attention only long after the event, not associating the visual impairment with sun exposure, which makes the diagnosis difficult5.
On fundoscopy, marked macular edema may be seen in the first few days after exposure. This edema tends to resolve in a short period, usually between two and three days, giving way to a yellowish-white spot surrounded by dark pigmentation with a mottled pattern in the foveal region. This progresses to a circular, red, well-defined spot1,2. The initial macular lesion, present in the acute phase, is yellowish-white and resembles lesions caused by other conditions, such as Best disease. Contrarily, in the chronic phase, if no history of exposure to radiation is known, the fundoscopic findings can be confused with other diseases, including tamoxifen retinopathy, juxtafoveal telangiectasia, vitreomacular traction syndrome, acute retinal pigment epitheliitis, and Stargardt disease. Unlike SM, these are progressive diseases2.
In general, differential diagnosis of isolated foveal disease is broad, and may include a full-thickness macular hole, an internal lamellar macular hole, a pseudohole associated with an epiretinal membrane, focal geographic atrophy, limited choroidal neovascularization, a small focal area of central serous retinopathy, cystoid macular edema with a large central cyst, idiopathic juxtafoveal telangiectasia (MacTel), a congenital optic pit, cervical lesions, and a solitary macular cyst2.
OCT is used to assist in the diagnosis. This is a non-invasive test that has become the main modality for detecting and monitoring structural changes in the retina. Not only is OCT a diagnostic tool, but it also has prognostic value. In the acute stages of SM, the most common findings are hyperreflective areas in some or all foveal layers, changes in reflectivity, and decreased RPE reflectivity. In the chronic phase, a hyporeflective area appears between the internal and external segments of the photoreceptors, which, although not pathognomonic, is relatively specific to SM1,2.
FAF allows the visualization of lipofuscin contained in RPE cells, with high sensitivity for SM lesions. The characteristic pattern is the presence of small areas of hypoautofluorescence surrounded by an uneven ring of hyperautofluorescence. However, FAF is not as sensitive as OCT. In very late cases, occurring months or years after injury, when the event has been forgotten by the patient, FAF is a useful test when there are no changes in OCT1,3. OCT and FAF imaging reliably detect significant macular defects associated with sun injury. However, all clinically affected eyes show defects in OCT, while not all defects are identified in FAF, but when findings are identified, they are correlated in a multimodal manner by using both imaging techniques2,6.
Fluorescein angiography (FA) is an invasive test, with intravenous contrast administration, that rarely provides relevant findings in cases of SM, but it is useful to rule out other conditions1. Exudations may be observed during the acute phase in the injured area, while in the chronic phase a window-shaped defect is characteristic3,6.
Regarding the prognosis, most cases of SM progress to complete recovery. In cases without full resolution, there is a permanent but modest decrease in VA and persistent scotomas. Most of the visual recovery occurs in the first few weeks after exposure. This improvement is possible because although the cones and rods do not have reproductive capacity, they do have regenerative capacity, which is possible as long as the cell nucleus is not damaged. The overall prognosis is likely to have improved due to awareness-raising campaigns. However, this subjective improvement contrasts with the presence of irreversible changes in the retina, which are easily demonstrable by OCT.
For treatment purposes, there are descriptions of the use of acetylsalicylic acid, vitamin A, vitamin C, and oral corticosteroids, either alone or in combination, but none of these treatments has scientifically proven results. OCT examination makes it possible to visualize, follow-up, and monitor lesions that may be asymptomatic and not identified in other types of examinations. Thus, the best treatment is prevention, with more campaigns and guidelines about the precautions to avoid maculopathy that should be concomitantly disseminated in any exposure to risks.
REFERENCES
1. Modenese A, Korpinen L, Gobba F. Solar radiation exposure and outdoor work: an underestimated occupational risk. Int J Environ Res Public Health. 2018;15(10):2063
2. Comander J, Gardiner M, Loewenstein J. High-resolution optical coherence tomography findings in solar maculopathy and the differential diagnosis of outer retinal holes. Am J Ophthalmol. 2011;152(3):413-419.e6.
3. Jain A, Desai RU, Charalel RA, Quiram P, Yannuzzi L, Sarraf D. Solar retinopathy: comparison of optical coherence tomography (OCT) and fluorescein angiography (FA). Retina. 2009;29(9):1340-5.
4. Louzada RN, Ferrara D, Moult EM, Fujimoto JG, Abu-Qamar O, Duker JS, et al. Full-thickness macular hole size by hypertransmission signal on spectral-domain optical coherence tomography. Retina. 2021;41(10):2059-2065.
5. Wu CY, Jansen ME, Andrade J, Chui TYP, Do AT, Roen RB, et al. Acute solar retinopathy imaged with adaptive optics, optical coherence tomography angiography, and en face optical coherence tomography. JAMA Ophthalmol. 2018;136(1):82-85.
6. Garg SJ, Martidis A, Nelson ML, Sivalingam A. Optical coherence tomography of chronic solar retinopathy. Am J Ophthalmol. 2004;137(2):351-4.
| AUTHORS INFORMATIONS |
|
 |
» Dillan Cunha Amaral https://orcid.org/0009-0002-7948-154X https://lattes.cnpq.br/7959357721386149 |
 |
» Guilherme da Silva Ferreira da Costa https://orcid.org/0000000151393666 http://lattes.cnpq.br/9872668888772635 |
 |
» Milton Ruiz Alves https://orcid.org/0000000167595289 http://lattes.cnpq.br/6210321951145266 |
 |
» Márcio Penha Morterá Rodrigues https://orcid.org/0000000327711542 http://lattes.cnpq.br/5991470601192448 |
 |
» Adroaldo de Alencar Costa Filho https://orcid.org/0009000792979111 http://lattes.cnpq.br/3152075298233631 |
 |
» Ricardo Noguera Louzada https://orcid.org/0000000296105768 http://lattes.cnpq.br/5978866539118374 |
Funding: No specific financial support was available for this study.
Approved by the following research ethics committee: Faculdade de Medicina da Universidade de São Paulo (CAAE: 50810021.7.0000.0068).
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
July 31, 2023.
Accepted on:
October 22, 2023.