Fábio Ejzenbaum
DOI: 10.17545/eOftalmo/2023.0044
Este artigo pertence à Edição Especial Neuroftalmologia por imagem: acima e além
We hypothesized that nystagmus could be a sign of neurological disease. This study included a 9-months-old boy presenting with eye twitching for 3 months. The child was born at normal delivery without intercurrences and with good neurological development.
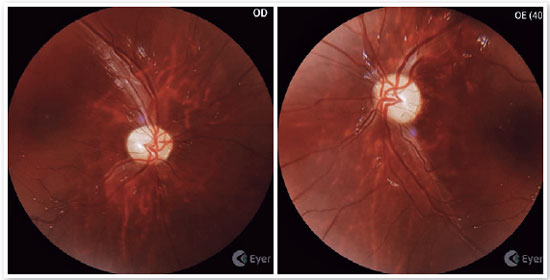
The examination revealed a centered Hirschberg test, good tracking of objects, and a fine, fast-frequency, low-amplitude intermittent nystagmus (Video 1). The photomotor reflexes were slightly reduced and a slight pallor of the optic nerves was noticed.
Cafe au lait stain on his right leg (Figure 1).

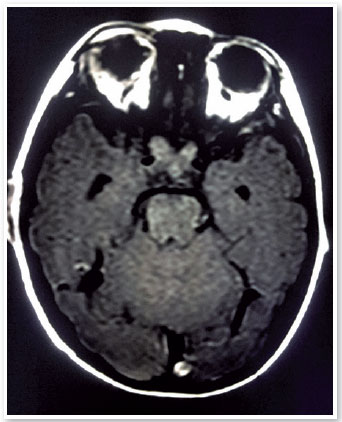
Based on these findings, an MRI examination was requested, which revealed a thickening of both optic nerves in the chiasm region (Figure 2). Thus, an optic nerve glioma hypothesis was confirmed and the child was referred for chemotherapy treatment.
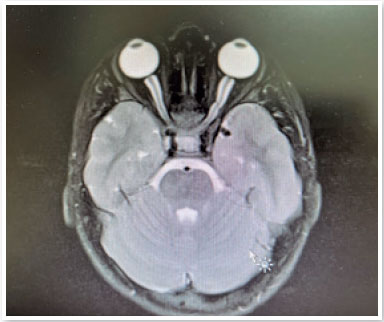
After 5 years, the child underwent significant tumor reduction (Figure 3), maintaining nystagmus (Video 2) and presenting with a 20/25 visual acuity in both eyes. In the fundus picture, a temporal pallor of the optic nerve can be observed (Figure 4).
This study revealed a patient with acquired and early nystagmus. In these patients, it is important to conduct a neurological investigation with neuroimaging that defines the diagnosis. Optic pathway gliomas (OPG) are low-grade neoplasms that affect the precortical visual pathway and are most common in children and adolescents, representing 2-5% of all cases of childhood central nervous system tumors1. They can either occur sporadically or in association with the tumor predisposition syndrome2.
Among children with neurofibromatosis type 1 (NF1), approximately 20% develop OPG3. The presented video confirmed the diagnosis of glioma/NF1 association as the child had a cafe au lait stain. The diagnosis of ONG can usually be made based on neuroimaging and a comprehensive clinical exam. Furthermore, sporadic ONGs only involve one optic nerve, while those associated with NF1 can be unilateral or bilateral.
When tissue is obtained, the most common histology is WHO grade I juvenile pilocytic astrocytoma4, as observed in the presented case.
REFERENCES
1. Farazdaghia MK, Katowitza WR, Avery RA. Current treatment of optic nerve gliomas. Curr Opin Ophthalmol. 2019;30(5):356-363.
2. Avery RA, Fisher MJ, Liu GT. Optic pathway gliomas. J Neuroophthalmol. 2011;31(3):269-78.
3. Listernick R, Charrow J, Greenwald M, Mets M. Natural history of optic pathway tumors in children with neurofibromatosis type 1: a longitudinal study. J Pediatr. 1994;125(1):63-6.
4. de Blank PMK, Fisher MJ, Liu GT, Gutmann DH, Listernick R, Ferner RE, et al. Optic Pathway Gliomas in Neurofibromatosis Type 1: An Update: Surveillance, Treatment Indications, and Biomarkers of Vision. J Neuroophthalmol 2017;37Suppl 1 (Suppl 1):S23-S32.
| AUTHOR INFORMATION |
|
 |
»Fábio Ejzenbaum http://orcid.org/0000-0002-8802-5610 http://lattes.cnpq.br/7170759182175903 |
Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
April 28, 2023.
Accepted on:
April 28, 2023.