Leonardo Provetti Cunha1,2
DOI: 10.17545/eOftalmo/2023.0035
Este artigo pertence à Edição Especial Neuroftalmologia por imagem: acima e além
The differential diagnosis of vision loss is a broad process and mainly involves disorders affecting the retina or optic nerve. The differentiation of these conditions requires a detailed medical history, a comprehensive ophthalmologic examination, and appropriate complementary examinations. Here, we present the fundus images of a patient who complained of bilateral visual impairment and had marked optic disk edema. The findings of the optic disk suggested optic neuropathy as the cause of the visual impairment. However, fundus images, including fundus autofluorescence and optical coherence tomography (OCT) images, together with the patient’s clinical history indicated retinal involvement, which had significant impacts on the diagnosis and treatment of this patient.
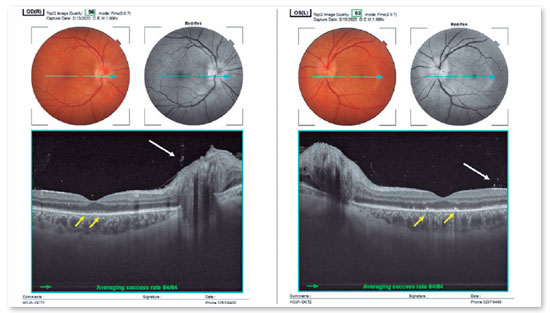
The patient was a 37-year-old man who worked in the food industry. He complained of experiencing painless bilateral vision loss for the last 4 months. He noted dark scotomas and blurred vision in both eyes (OU). The best corrected visual acuity (BCVA) was 20/20 in his right eye (OD) and 20/80 in his left eye (OS). The fundus. Fundus retinography revealed bilateral optic disk edema and mild pigmentary changes in the posterior pole, which were more prominent in the left eye (Figure 1). A previous magnetic resonance imaging scan of the brain did not reveal any relevant findings. Fundus autofluorescence imaging revealed areas of hyperautofluorescence interspersed with points of hypoautofluorescence throughout the macular region and around the optic disk (Figure 1). Furthermore, OCT revealed an increase in the thickness of the peripapillary nerve fiber layer, showed no signs of anteroposterior displacement of the optic disk and the peripapillary retina/Bruch’s membrane complex, and revealed signs of hyperreflective dots over the optic disk, which were suggestive of the presence of inflammatory cells in the vitreous in OU (Figure 2). B-scan OCT performed over the macula revealed fragmentation and disruption of the ellipsoid zone (EZ) and external limiting membrane (MLE) OU (Figure 2). These findings suggested the possibility of syphilitic neuroretinitis. Moreover, the patient had a positive VDRL test result (1/64), and the fluorescent treponemal antibody-absorption (FTA-ABS) test identified IgM and IgG antibodies. The serological test for HIV was negative. Based on the test results, the patient was treated with crystalline penicillin G for 14 days. Ophthalmologic examination at 6 weeks after treatment showed an improvement in VA (20/20 in OU). Moreover, OCT revealed improvement of the optic disk edema, a reduction in the presence of inflammatory cells in the vitreous, and reconstitution of the EZ and MLE (Figure 3). The patient underwent ophthalmological and neurological follow-up, and there have been no intercurrences or signs of worsening.
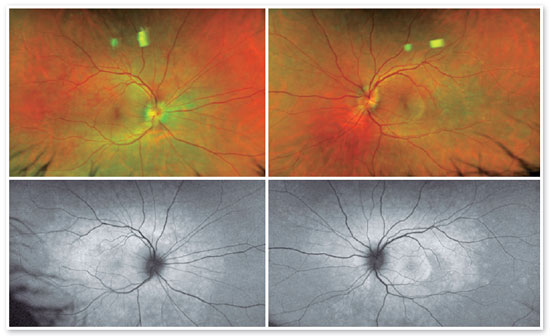
In our case, the possibility of neuroretinitis was suggested by the occurrence of vision loss associated with optic disk edema and retinal pigment changes in OU1. Classically, the term neuroretinitis is used for inflammatory conditions that simultaneously affect the optic disk and retina2-5. Acute syphilitic posterior placoid chorioretinitis (ASPPC) is a rare manifestation of ocular syphilis that has been described in patients with secondary syphilis. ASPPC lesions are located on the retinal surface (retinal pigmented epithelium) at or near the macula. They are placoid, are yellowish in color, and have a faded center with the stipulation of the adjacent retina. These lesions result from inflammation, possibly due to direct invasion of the choriocapillaris by Treponema pallidum, deposition of immune complexes, or a combination of these.
OCT is one of the most valuable tools in the diagnosis of ocular syphilis. In addition to optic disk edema, it reveals discrete inflammatory signs of the pre-papillary vitreous and disruption of the EZ and MLE. When these findings are present along with optic disk edema, there is a high suspicion of ocular syphilis. In our patient, fundus autofluorescence and OCT findings clearly pointed to a process at the choroidretinal pigment epithelium complex level, which had repercussions in the photoreceptor internal/external segment junction (EZ) layer and the MLE. After treatment, we observed a complete ultrastructural recovery of these OCT findings, including the outer retinal changes, suggesting syphilis-related temporary physiological impairment of the retina. In such cases, prompt diagnosis allows adequate treatment, increasing the chances of visual improvement.
REFERENCES
1. Kiss S, Damico FM, Young LH. Ocular manifestations and treatment of syphilis. Semin Ophthalmol. 2005;20(3):161-7.
2. Purvin VA, Chioran G. Recurrent neuroretinitis. Arch Ophthalmol. 1994;112(3):365-71.
3. Ghauri RR, Lee AG. Optic disk edema with a macular star. Surv Ophthalmol. 1998;43(3):270-4.
4. Purvin V, Sundaram S, Kawasaki A. Neuroretinitis: review of the literature and new observations. J Neuroophthalmol. 2011; 31(1):58-68.
5. Brazis PW, Lee AG. Optic disk edema with a macular star. Mayo Clin Proc. 1996;71(12):1162-6.
AUTHOR INFORMATION

Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
May 5, 2023.
Accepted on:
July 21, 2023.