Sidney Julio Faria e Sousa
DOI: 10.17545/e-oftalmo.cbo/2016.62
ABSTRACT
This report offers guidelines to the general ophthalmologist on the first consultation with a patient with suspected strabismus. The two main objectives of this report are to describe how to determine whether strabismus actually exists and, in case it does, how to determine whether it is due to an eye disorder or systemic disease. The results of a series of tests conducted by the examiner should lead to logical deductions that will ultimately provide a diagnosis. The patient and his or her family can then be advised about the subsequent measures to be taken.
Keywords: Strabismus: Torticollis: Esotropia: Exotropia
RESUMO
Este artigo fornece diretrizes ao oftalmologista geral para o primeiro atendimento do paciente com suspeita de estrabismo. Os dois principais objetivos são: saber se o estrabismo realmente existe e, em caso positivo, determinar se ele se deve a alguma enfermidade ocular ou sistêmica grave. Na busca dessas respostas, o examinador deverá realizar uma série de exames e raciocínios que, no final, trarão as condições de orientar adequadamente o paciente ou sua família sobre as providências subsequentes a serem tomadas.
Palavras-chave: Estrabismo: Torcicolo: Esotropia: Exotropia
INTRODUCTION
The diagnosis of strabismus in a child can be shocking for parents. Fearing the implications of such a diagnosis, many parents ignore the problem, bolstered by the hope that the deviation will disappear spontaneously over time. This attitude is especially common in the early stages of the disorder when strabismus is not very obvious or constant and tends to delay the diagnosis and treatment, not only of the oculomotor disturbance, but also of any associated visual abnormalities. However, eventually the family will consult an ophthalmologist who should be adequately prepared for examining these cases. The objective of this report is to guide the ophthalmologist in conducting the first consultation objectively and effectively.
GUIDELINES
On presentation of the patient, several questions need to be answered.
Does strabismus actually exist?
In cases of suspected strabismus, the first concern of the examiner is to determine whether the deviation exists. To answer this question, it is of benefit to divide it into two parts, as follows.
1. Does the patient appear to be strabismic?
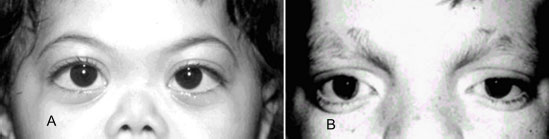
The diagnosis should be made with care because numerous conditions can simulate strabismus. For example, epicanthal folds can simulate convergent strabismus. This condition occurs when the skin of the eyelid covers the nasal corner of the eye in a proportion greater than would normally be expected. The nasal sclera is less visible, giving the impression of endotropy (Figure 1A). It is prevalent in children with a poorly developed nose base. Hypertelorism that simulates exotropy is another example in which the excessive distance between the orbits creates the impression that the eyes are turned outwards (Figure 1B).
On the other hand, a true deviation may not be detected during the examination because of its intermittent nature or because it is small in degree.
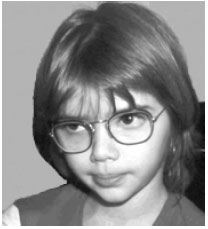
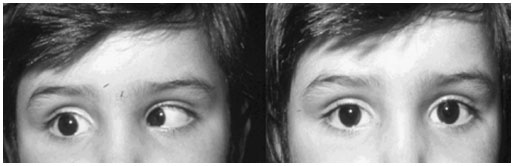
2. Does the patient have torticollis (wry neck)?
Often the only evidence of strabismus is the twisted position of the neck. The head may be tilted to one side or turned to the right or left, and/or there may be elevation or lowering of the chin. A typical sign of strabismus with limited eye rotation is muscular paresis or mechanical restriction of movement. The patient positions the head to the side opposite the limitation to avoid double vision. In the presence of wry neck, the head needs to move in the direction opposite the torticollis to reveal the deviation; head tilts suggest paresis of the superior oblique muscles (Figure 2); horizontal twisting is associated with problems in the horizontal rectus muscles; and rising and/or lowering of the chin indicates complications in the vertical rectus muscles.
3. Do the corneal reflexes suggest deviation?
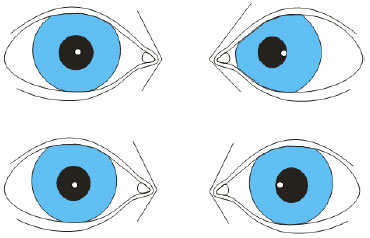
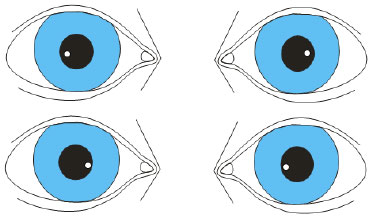
The cornea functions like a convex mirror. When the eyes look directly into a light source, corneal reflections form in the center of the pupil. However, this only occurs when both eyes are fixed on the target. When the eye is turned inward (endotropy), the corneal reflection appears temporally decentralized, and when the eye is turned outward (exotropy), the reflection is nasally decentralized (Figure 3). Asymmetry of the corneal reflections between the eyes is strongly indicative of strabismus. However, this condition should be differentiated from the symmetrically decentralized corneal reflexes in some non-strabismic eyes. In the latter, the visual axes do not coincide with the pupillary centers. When the patient looks at a light source, the corneal reflections are symmetrically decentralized either temporally, simulating endotropy, or nasally, simulating exotropy (Figure 4). The absence or presence of symmetry in the reflections differentiates the two conditions.
4. How does the patient respond to the simple cover test?
The main test for the diagnosis of strabismus is the simple cover test (Figure 5). The patient is asked to stare at an object. The fixed eye is covered and the behavior of the other eye is observed. The movement of the uncovered eye to assume fixation indicates deviation, and thus strabismus. In cases in which the uncovered eye does not move, the test is repeated with the other eye. In cases in which neither eye moves, the patient probably does not have strabismus. In children aged less than one year old, the cover test can be conducted using the examiner's thumb, and the fingers serve as support for the patient's forehead. An excellent stimulus for this age group is the shake of a bunch of keys in front of the patient's eyes.
The simple cover test has flaws. The conditions that most often lead to its failure are lack of the patient's attention, eccentric fixation, and microstrabismus. In inattention and eccentric fixation, the refixation movement may not occur even in the presence of strabismus. In the first case this would be because the patient is not looking at the target and in the second case because the object being viewed is already viciously aligned with an extrafoveal point. In microstrabismus (deviation equal to or smaller than 5 prism-diopters), the movement of fixation may not be detected by the examiner.

5. Is there a clinical explanation for strabismus?
This question can only be answered with a complete eye examination. The patient should be cyclopleged to detect severe refraction defects, opacity of the transparent media, and retinal and optic nerve lesions that justify the suspicion of strabismus. The likelihood of an oculomotor abnormality increases in the case of positive findings.
6. Is the vision affected?
The difference in vision between the two eyes may be a cause or a consequence of strabismus, and therefore this information is essential. It is not necessary to measure vision with grouped optotypes in this initial examination. The examiner should use the resource that most appeals to the patient. Children tend to be more interested in isolated optotypes, especially when presented creatively in the form of a game.
In infants, vision can only be inferred. This inference is based on the pattern of fixation and the alternation of deviation. The pattern of fixation is defined as the way that the eye observes an object. Eyes with low vision (<0.05) have difficulty finding the object and keeping it in view. Pendular nystagmus is the most typical example of this eventuality. The pattern of fixation is tested by having the eye follow an object that is moving slowly in the field of vision.
Alternating strabismus occurs when the vision in each eye is similar. In cases in which there is a difference in vision between the eyes, the brain tends to favor the eye with better acuity. Therefore, the greater the preference for one eye, the higher the chance that the other eye will have worse vision.
Normal vision is inferred in cases in which no eye deviation or abnormality is found.
7. Are there any familial or environmental causes of strabismus?
It is necessary to investigate whether the patient underwent any fetal distress, and whether there are any close relatives with serious hyperopia or strabismus. These three conditions increase the chances of manifestation of the condition.
If after all these questions have been answered it is possible to conclude that there is no evidence of strabismus, a return visit should be scheduled for three months later to confirm the diagnosis. In cases in which there is still no evidence of the disorder, additional return visits should be scheduled until a definite diagnosis is made.
This author has examined patients with epicanthus at the age of 8 months and with eye deviations at the age of 2 years. In cases in which strabismus is present, the cover test gives clues about the type of deviation: horizontal, vertical, or mixed. Although this information is important for the characterization of the oculomotor condition and treatment planning, the detection of the deviation is most important. After diagnosis, the examiner should determine whether the condition is associated with severe ocular or systemic disease.
Is the deviation secondary to some severe illness?
The strategy for answering this question is to classify the strabismus as belonging to one of the following five classifications.
1. Paretic strabismus. This results from the weakness of one or more extraocular muscles. The most common causes are lesions of cranial nerve pairs II, IV, and VI. This type of strabismus is distinguished by the asymmetry of the deviations and limited eye rotation. The asymmetry is observed in cases in which the deviation increases with the fixation of the affected eye and in the field of action of the weakened muscle. The diagnosis is made by examining the eye rotations and by measuring the deviations in the nine diagnostic positions of the eye: forward, right, left, up, down, right up, left up, right down, and left down. Photographs of the child that show abnormal positions of the head will indicate that the problem has existed at least from the time of the oldest photograph.
2. Sensory strabismus. This results from a difficulty in merging the images from the two eyes, caused by a marked difference in image quality. The most frequent causes are high-magnitude anisometropia (>3D), opacity of the transparent media and abnormality of the eye fundus and optic nerve. The diagnosis is made using the ocular refraction test, reflex test, biomicroscopy and fundoscopy.
3. Restrictive strabismus. This results from a mechanical restriction in ocular rotation and includes Duane1 and Brown2 syndromes, orbital floor fractures 3, and thyroid myopathy 4. The differential diagnosis of paretic strabismus is made using electromyography or the forced-duction test that evaluates the passive rotation of the eye in the field in which there is limited movement. It is performed under topical anesthesia, and the limbus is secured with forceps on the side opposite the intended rotation. The test is considered positive in cases in which there is mechanical restriction of movements. In paresis, rotation with the forceps encounters no resistance. The diagnosis of restrictive strabismus is easier in cases in which the ophthalmologist has knowledge of restrictive diseases of the eyeball (Figure 6).
4. Accommodative strabismus. This results from excessive or insufficient convergence accommodation. It is associated with high refractive defects or an abnormal CA: A ratio. The diagnosis is made by studying the variation of the angle of deviation with and without optical correction. The CA: A ratio measures the fraction of ocular convergence (CA) associated with the accommodation (A). A very high ratio can lead to endodeviation and a very low ratio can lead to exodeviation. Other cases of ocular convergence involve fusional convergence (FC) originating from the tendency of the visual cortex to fuse the images of both eyes.
5. Essential Strabismus. This is of indeterminate cause. It may result from a congenital fusional difficulty. The diagnosis is made by exclusion.
The cases of strabismus usually associated with severe illnesses are paretic and sensory strabismus. The former, particularly those with recent evolution without a history of trauma, should be immediately referred for neurological investigation. However, before such referral, the following precautions should be taken: (1) ensure that the strabismus is recent because older conditions generally do not require immediate attention; (2) confirm that the strabismus is paretic and not restrictive; (3) in cases of recent onset with confirmation of the type of strabismus, wait for a definition of the condition by repeated ocular motility tests; and (4) in cases in which the superior oblique muscle is affected, confirm that the paresis is recent and not a recently decompensated but old paresis. Old images showing twisted head positions reinforce the second hypothesis.
Sensory strabismus suggests problems in the eye or vision system. It probably indicates a threat to overall health. The first sign of a retinoblastoma may be strabismus.
Considering that accommodative and essential strabismus are the more common classicications, the probability of the need for a general clinical follow-up in the strabismic patient is very low. Therefore, it is expected that in most of the cases under the responsibility of the clinician, the decision will be limited to either treating them or referring them to a specialist in ocular motricity. In either case, the examiner should adequately guide the patient and the family on the best course of action.
REFERENCES
1. DeRespinis PA, Caputo AR, Wagner RS, Guo S. Duane's retraction syndrome. Surv Ophthalmol. 1993;38(3):257-88. http://dx.doi.org/10.1016/0039-6257(93)90077-K
2. Faria e Sousa SJ. Síndrome da restrição do obliquo superior. Arq Bras Ophthalmol. 1981;44(5):155-6
3. Tang DT, Lalonde JF, Lalonde DH. Delayed immediate surgery for orbital floor fractures: less can be more. Can J Plast Surg. 2011 ; 19(4):125-8. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3269201/
4. Hodes BL, Shoch DE. Thyroid ocular myopathy. Trans Am Ophthalmol Soc. 1979;77: 80-103. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1311695/pdf/taos00022-0102.pdf

Funding source: None
Conflicts of interest: None
Received on:
October 2, 2016.
Accepted on:
October 11, 2016.