Eliza Antonieta Rosana Negrão Grangeiro1; Simone Cristine Hermes Hoff2; Aline Cristina Fioravanti Lui3; Mário Henrique Camargos de Lima4
DOI: 10.17545/e-oftalmo.cbo/2016.70
ABSTRACT
Acute retinal necrosis (ARN) is a rare form of uveitis caused by a viral infection. It manifests as necrotizing retinitis and can result in serious vision loss if not correctly diagnosed and treated. This article reports the case of a patient with a history of previous treatment for ARN, which was completed 3 months ago, who had a relapse in spite of being immunocompetent. The relapse was confirmed and documented by measuring IgM levels in the aqueous humor as blood serology only showed positive IgG. The ophthalmic findings, clinical evolution, treatment (including prophylaxis), and follow-up are described.
Keywords: Retinitis; Cytomegalovirus; Retina
RESUMO
A necrose aguda de retina (NAR) é uma rara uveíte causada por infecção viral que se apresenta como uma retinite necrotizante e pode resultar em grave perda visual se não for diagnosticada e tratada corretamente. É relatado aqui o caso de uma paciente com história de tratamento completo prévio, realizado há três meses, para necrose aguda de retina, que apresentou recidiva embora seja imunocompetente. A confirmação da recidiva foi documentada com dosagem de IgM no humor aquoso visto que a sorologia sanguínea apresentava-se apenas com IgG positiva. São descritos seus achados oftalmológicos, a evolução clínica, o tratamento (incluindo a profilaxia) e o seguimento.
Palavras-chave: Retinite; Citomegalovírus; Retina
INTRODUCTION
Acute retinal necrosis (ARN) is a rare form of uveitis caused by a viral infection. It manifests as necrotizing retinitis that can result in devastating vision loss if not correctly diagnosed and treated.1,2,3 It can be caused by multiple members of the Herpesviridae family, most frequently by Herpes simplex and Herpes zoster and less frequently by cytomegaloviruses (CMVs).2
ARN is a rare disease that typically affects immunocompetent patients,4,5,6 causing extensive and progressive retinitis.7 The diagnostic criteria for ARN are posterior uveitis, retinal necrosis, occlusive vasculopathy, and progression of the retinitis if untreated.3 PCR analysis of the aqueous humor can be used to identify the viral etiology of ARN, with sensitivity and specificity greater than 90%. It can also be used to confirm a diagnosis. Treatment comprises the administration of antiretroviral drugs based on the etiology.3,8
Case details
A 51-year-old female patient was admitted with a complaint of diminished visual acuity (VA) of the right eye (RE) for 1 week. She had undergone treatment for ARN 3 months earlier, for 15 days (ganciclovir 700 mg/day), with no prophylaxis after discharge.
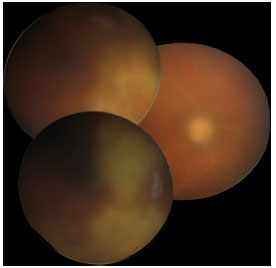
The ophthalmic examination showed VA with correction in “counting fingers” at 1 m for RE and 20/20 for the left eye (LE). On biomicroscopic examination, RE presented with nongranulomatous keratic precipitates in the endothelium, rare cells in the anterior chamber, and paralytic mydriasis; LE showed no abnormalities. Tonometry revealed the intraocular pressure to be 18/14 mmHg (9 am). Fundoscopy of RE showed a pale optic nerve, superior and inferior phantom vessels, and an active inferior temporal retinitis, with superior temporal cicatricial retinitis and 2+/4+ vitreitis (Figure 1). LE was found to be normal (Figure 2).
The following tests were performed to diagnose infectious posterior uveitis: complete blood count, coagulation profile, VDRL, FTA-ABS, PPD, chest X-ray, head CT, and serology for hepatitis B. All the tests revealed normal results. Serology for toxoplasmosis and CMV was negative for IgM and positive for IgG, with no evidence of activity. Thus, it was necessary to perform a puncture of the anterior chamber to test the aqueous humor for CMV. The result was found to be positive for IgM (89.40).
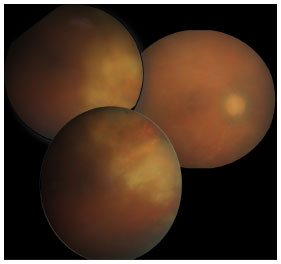
The patient was intravenously treated with ganciclovir 700 mg/day for 15 days. Her VA improved to 20/100 in RE; biomicroscopy showed posterior synechia for 3-9 h, and fundoscopy showed a pale optic nerve, phantom vessels, and an area of cicatricial atrophy corresponding to the location of the inferior and superior temporal retinitis (Figure 3). Prophylaxis was performed with ganciclovir 700 mg/day three times a week for 10 weeks. In the 1-year follow-up, there were no further relapses and the contralateral eye was not affected.
DISCUSSION
ARN due to CMV is a rare condition, which evolves with an extensive area of retinal necrosis and severe visual loss if not properly treated. Although diagnosis is based on retinal changes, serology tests and PCR analysis of the aqueous humor can also be performed to help with the specific therapy.3
The present study patient had a history of ARN for 3 months and was treated with ganciclovir, with no prophylaxis after discharge. Even without immunodeficiency, the patient had a relapse of her previous condition, and the etiology was confirmed by measuring the IgM levels in the aqueous humor, with positive results for CMV. Therefore, therapy with ganciclovir 700 mg/day for 15 days was resumed, resulting in complete cicatrization of the retinitis area and consequently in the improvement of VA. The decision was taken to keep the patient on a prophylactic dose of ganciclovir 700 mg/day three times a week for 10 weeks. Since then, the patient has experienced no further episodes of relapse or infection of the contralateral eye for 1 year.
REFERENCES
1. Rayess N, Rahimy E, Dunn JP. Bilateral neuroretinitis and retinal hemorrhages in an immunocompetent patiente. JAMA Ophthalmol. 2014; 132(10): 1243-44. http://dx.doi.orn/10.1001/iamaophthalmol.P014.3341
2. chaal S, Kagan A, Wang Y, Chan C-C, Kaplan HJ. Acute retinal necrosis associated with epstein-barr virus. JAMA Ophthalmol. 2014; 132(7):881-2. httD://dx.doi.orn/10.1001/iamaoDhthalmol.2014.266
3. Shantha JG, Weissman HM, Debiec MR, Albini TA, Yeh S. Advances in the management of acute retinal necrosis. Int Ophthalmol Clin. 2015;55(3):1-13. Disponível em: httDs://www.ncbi.nlm.nih.nov/Dmc/articles/PMC4567584/-http://dx.doi.org/10.1097/IIO.0000000000000077
4. Asano Y, Kagawa H, Kamo Y, Shiohara T. Cytomegalovirus disease during severe drug eruptions: report of 2 cases and retrospective study of 18 patients with drug-induced hypersensitivity syndrome. Arch Dermatol. 2009;145(9):1030-6. http://dx.doi.org/10.1001/archdermatol.2009.195
5. Stewart MW, Bolling JP, Mendez JC. Cytomegalovirus retinitis in an immunocompetent patient. Arch Ophthalmol. 2005;123(4):572-4. http://dx.doi.org/10.1001/archopht.123.4.572
6. Pathanapitoon K, Tesavibul N, Choopong P, Boonsopon S, Kongyai N, Ausayakhun S, et al. Cytomegalovirus-associated posterior uveitis and panuveitis in patients without human immunodeficiency virus infection. JAMA Ophthalmol. 2013;131(5):638-45. http://dx.doi.org/10.1001/jamaophthalmol.2013.2860
7. Karavellas MP, Lowder CY, Macdonald JC, Avila CP Jr, Freeman WR. Immune recovery vitritis associated with inactive cytomegalovirus retinitis. Arch Ophthalmol. 1998; 116(2): 169-75. http://dx.doi.org/10.1001/archopht.116.2.169
8. Limaye AP, Kirby KA, Rubenfeld GD, Leisenring WM, Bulger EM, Neff MJ, et al. Cytomegalovirus reactivation in critically III immunocompetent patients. JAMA. 2008;300(4):413-22. http://dx.doi.org/10.1001/jama.300.4.413




Funding source: None applicable
Conflicts of interest: None
Received on:
November 3, 2016.
Accepted on:
November 28, 2016.