Rafael Erthal Robbs1; Gustavo Erthal Robbs2; Erika Marques Demori1
DOI: 10.17545/eOftalmo/2022.0024
ABSTRACT
Graves’ disease and myasthenia gravis are both related to autoimmunity and can coexist in the same patient. We report a case of Graves’ ophthalmopathy associated with myasthenia gravis, asymmetric ocular form, and its diagnosis based on clinical findings and a positive ice-pack test.
Keywords: Graves’ ophthalmopathy; Myasthenia gravis; Blepharoptosis; Exophthalmos.
RESUMO
Doença de Graves e miastenia gravis, ambas doenças relacionadas a autoimunidade, podem coexistir em um mesmo paciente. Relatamos um caso de oftalmopatia de Graves associado a miastenia gravis, forma ocular assimétrica, seu diagnóstico baseado em achados clínicos e ice-pack test positivo.
Palavras-chave: Oftalmopatia de Graves; Myasthenia gravis; Blefaroptose; Exoftalmos.
INTRODUCTION
Graves’ disease and myasthenia gravis (MG), both related to autoimmunity, can coexist in the same patient. Few population studies have associated both conditions, but there seems to be a considerable occurrence of the diseases as comorbidities1. A population study identified a prevalence of thyroid disease in patients with MG of around 18.4% (odds ratio 3.895, 95% interval of confidence 3.574-4.246)2. We report a case of Graves’ ophthalmopathy associated with MG, asymmetric ocular form, and its diagnosis based on clinical findings and a positive ice-pack test.
CASE REPORT
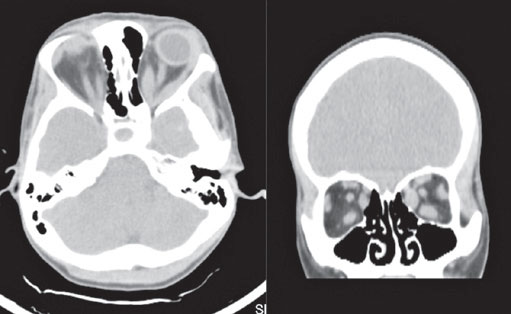
DMS, female, 35 years old, with Graves’ disease, complaining of ptosis in the left eye (OS) and fluctuating diplopia throughout the day, with no other clinical complaints. Ophthalmological examination showed upper eyelid retraction in the right eye, ptosis in the OS with accentuation of the ptosis it in supraversion, exophthalmos of 24 mm in the right eye and 25mm in the OS, restriction of extrinsic eye movement in all directions in the OS (Figure 1) with significant restriction in supraduction of the OS, fluctuating ophthalmoplegia in the OS, exotropia, and mild hypertropia in the OS. Uncorrected visual acuity of 20/20 in both eyes, isochoric pupils, no relative afferent pupillary defect, conjunctivae calm, and no chemosis was observed. Cranial computed tomography (CT) revealed thickening of the extrinsic extraocular muscles in both orbits, more significant on the left (Figure 2). The ice-pack test was then performed for 2 minutes, with significant improvement of the ptosis in the OS (Figure 3). A clinical diagnosis of MG, ocular form, associated with Graves Ophthalmopathy, was given. The patient subsequently underwent CT of the Chest, with no evidence of thymic hyperplasia or thymoma. On treatment with anticholinesterase therapy and optimization of hyperthyroidism, the patient was euthyroid, with improvement in the diplopia and ptosis.


DISCUSSION
The presence of ptosis in a patient with Graves’ ophthalmopathy should raise the diagnostic hypothesis associated with MG. In our case, the occurrence of MG in its ocular form can be seen, with clear asymmetry between the eyes, ptosis in the OS, fluctuating throughout the consultation, and demonstrating moments of fatigue, which drew the attention of the team to the diagnosis. With clinical suspicion, the ice-pack test was performed, which has high sensitivity and specificity for the diagnosis of MG3,4. This test can be a quick and fully accessible tool, although it must be interpreted with caution when the result is negative (low predictive value). In addition to the association of the case in question, the authors also bring to mind other diseases in the autoimmune spectrum of MG5, such as systemic lupus erythematosus, Addison’s disease, and dermatomyositis/polymyositis.
REFERENCES
1. Amin S, Aung M, Gandhi FR, Pena Escobar JA, Gulraiz A, Malik BH. Myasthenia Gravis and its Association With Thyroid Diseases. Cureus. 2020;12(9):e10248.
2. Chou CC, Huang MH, Lan WC, Kong SS, Kuo CF, Chou IJ. Prevalence and risk of thyroid diseases in myasthenia gravis. Acta Neurol Scand. 2020 Sep;142(3):239-247.
3. Larner AJ. The place of the ice pack test in the diagnosis of myasthenia gravis. Int J Clin Pract. 2004;58(9):887-8.
4. Golnik KC, Pena R, Lee AG, Eggenberger ER. An ice test for the diagnosis of myasthenia gravis. Ophthalmology. 1999;106(7):1282-6.
5. Fang F, Sveinsson O, Thormar G, Granqvist M, Askling J, Lundberg IE, et al. The autoimmune spectrum of myasthenia gravis: a Swedish population-based study. J Intern Med. 2015;277(5):594-604.
AUTHOR’S INFORMATION
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
October 25, 2022.
Accepted on:
November 9, 2023.