Paula Virginia Brom dos Santos Soares; João Carlos Gonçalves Cruz; Bruno Boalento dos Santos; Marcello Novoa Colombo Barboza; Guilherme Novoa Colombo Barboza; Priscilla Fernandes Nogueira
DOI: 10.17545/eOftalmo/2022.0018
ABSTRACT
Idiopathic intracranial hypertension is a rare condition that primarily affects obese women of childbearing age. If not treated promptly, it can result in serious eye manifestations, such as visual loss. This is a case report of chronic IIH with no papillary edema as seen in acute cases. The clinical picture was elucidated in association with the Neurology Department through an effective investigation that included neuroimaging, cerebrospinal fluid analysis, and a thorough ophthalmological examination. In the absence of other factors that increase intracranial pressure, a favorable outcome was obtained. Thus, a careful analysis of suspected cases of this disease is essential to avoid irreversible complications.
Keywords: Idiopathic intracranial hypertension; Neurology; Ophthalmology; Weight loss; Ventriculoperitoneal bypass
RESUMO
A hipertensão intracraniana idiopática é uma afecção rara, que acomete principalmente mulheres, em idade fértil e obesas. Se não for solucionada rapidamente, pode resultar em graves manifestações oftalmológicas, como perda visual. Relatamos um caso de hipertensão intracraniana idiopática crônica, com ausência de edema de papila típico dos quadros agudos. O quadro foi elucidado, associado ao setor de neurologia, a partir de uma investigação efetiva por meio de neuroimagem, líquor, exame oftalmológico completo e ausência de outras etiologias que elevem a pressão intracraniana, resultando em um desfecho favorável. Assim, é imprescindível a análise cautelosa de casos suspeitos dessa doença para evitar complicações irreversíveis.
Palavras-chave: Hipertensão Intracraniana Idiopática; Neurologia; Oftalmologia; Perda de Peso; Derivação Ventriculoperitoneal
INTRODUCTION
Idiopathic intracranial hypertension (IIH), also known as pseudotumor cerebri, is a disease characterized by elevated intracranial pressure in the absence of expansive lesions or secondary causes of intracranial hypertension in a patient with normal cerebrospinal fluid (CSF) levels and no altered level of consciousness1-3. It is a rare condition, with an annual incidence of 1-3 cases per 100,000 people, primarily affecting obese females of childbearing age(4,5).
The pathophysiological mechanism remains unclear, but some theories are accepted, such as genetics, metabolic causes, excessive CSF production, reduced CSF absorption, and increased cerebral venous pressure6,7. Headache is the earliest and most common symptom of this disease, which usually lacks specific characteristics such as intensity, location, type, frequency, and exacerbation factors2,8. The clinical picture also includes transient visual dimming, papilledema, photopsia, decreased visual acuity, photophobia, nausea, and vomiting1,5. Progressive peripheral field loss is frequent in IIH, but it is rarely reported by patients themselves2.
Although the neurological manifestations of IIH are generally mild, the disease can cause several serious ophthalmological manifestations, including marked visual loss in up to 25.8% of patients. Thus, careful examination of suspicious cases is necessary for early diagnosis, follow-up, and treatment of this disease2,9.
This article describes a case of chronic idiopathic intracranial hypertension without papilledema and emphasizes the importance of conducting a comprehensive neuro-ophthalmological investigation when a case of chronic IIH is suspected in order to avoid irreversible visual complications.
CASE REPORT
A 53-year-old white female patient, a secretary, presented to an ophthalmological consultation complaining of progressive visual impairment for 6 months. Her personal and ophthalmological history included systemic arterial hypertension, non-insulin-dependent type II diabetes mellitus, and grade II obesity (body mass index, 36.4 kg/m2). She had a history of trigeminal neuralgia and parasellar micromeningioma, both of which were followed up by a neurologist and remained stable for several years.
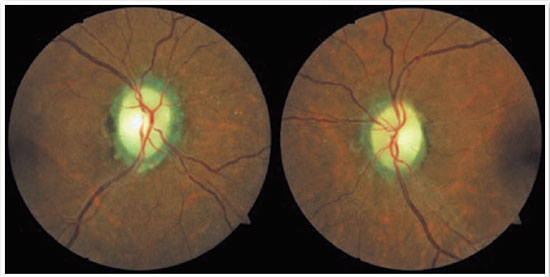
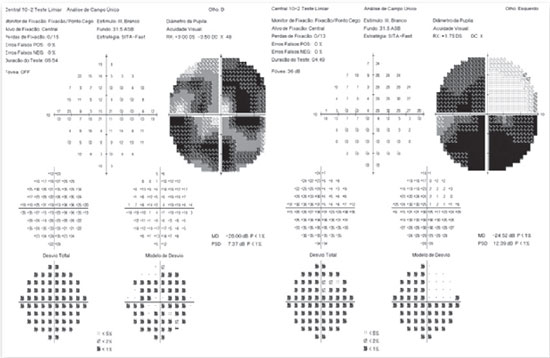
The ophthalmological examination revealed a corrected visual acuity (VAc) of 20/60 in both eyes (OU); refraction of -2.25/–2.25/45° in the right eye (OD) and -0.75/–1.00/50° in the left eye (OS); intraocular pressure (IOP) of 15 mmHg in the OD and 17 mmHg in the OS; and biomicroscopy without changes in OU. Fundoscopy revealed a cup-to-disc ratio of 0.2 in OU and pale, defined borders; 360° rims with physiological excavation (Figure 1); and direct pupillary reflexes of 3+ and 4+ and consensual pupillary reflexes of 2+ and 4+, respectively, in the OD and OS, along with a relative afferent pupillary defect in the OD. On the same day, a 302 visual field (VF) test was performed, with low reliability and absolute scotoma in OU. Thus, a 102 VF test, retinography, contrast magnetic resonance imaging (MRI) of the skull and orbits, and a neurological assessment were requested.
The patient returned after 7 months, reporting low visual acuity with gradual worsening in the OD (first noticed 1 week before) and sporadic, moderate-intensity headaches for 3 months.
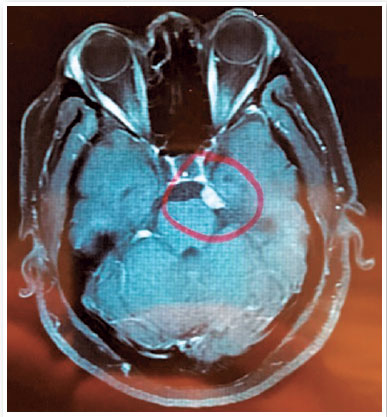
She brought the results of a 102 VF test performed 7 months ago with good reliability, the presence of complete inferior and incomplete superior arcuate scotoma in OU, a mean deviation (MD) of -23.00 decibels (dB) in the OD and -21.00 dB in the OS, and retinography confirming the fundoscopy visualization. Skull MRI performed 4 months earlier revealed a parasellar micromeningioma, flattening of the posterior sclera in OU (Figure 2), a tense oval image with hyperuptake in the cerebellum, and a small image consistent with lacunar infarction. The patient also provided a letter from a neurologist stating that there was no relationship between the brain tumor and the optic pathways.
A new ophthalmological examination revealed a worsening of the VAc to 20/80 in the OD and 20/50 in the OS as well as an IOP of 12 mmHg in the OD and 14 mmHg in the OS. Therefore, a CSF analysis with initial and final manometry was requested, and the patient was asked to bring the results of her previous tests for evaluation.
She returned after 2 months with a CSF examination revealing normal constituents, an initial pressure of 41 cmH2O, and a final pressure of 33 cmH2O. In addition, she brought the report of a CSF analysis performed 5 years ago with a manometry finding of 40 cmH2O. When asked about the follow-up, she said that acetazolamide was started, but she stopped taking it because she was asymptomatic. Thus, the diagnosis of chronic IIH was confirmed. Acetazolamide 250 mg every 6 hours and vitamin K 600 mg/day were then prescribed, and the importance of weight loss and neurological follow-up was reinforced.
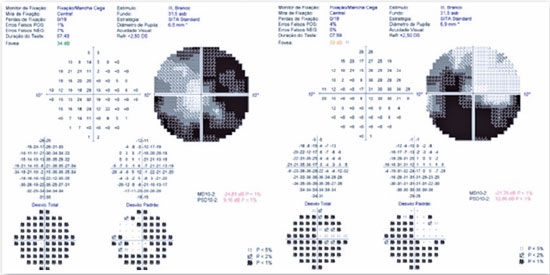
After 9 months, the patient returned with no weight loss and visual deterioration, reporting a VAc of 20/100 in the OD and 20/60 in the OS. A 102 VF test revealed deterioration in OU, with a MD of -26.00 dB in the OD and -24.52 dB in the OS (Figure 3). Because of the worsening of VF and VAc, the case was discussed with the Neurology Department, and ventriculoperitoneal shunt was chosen as treatment. One month after the procedure, the patient’s symptoms and visual acuity improved, with a VAc of 20/40 in the OD and 20/30 in the OS, 102 VF with a MD of -24.81 dB in the OD and -21.78 dB in the OS (Figure 4), improvement in the headache, and an initial CSF pressure of 20 cmH2O, with periodic follow-up at the Ophthalmology Department in collaboration with the Neurology Department.
DISCUSSION
Because IIH is diagnosed by exclusion, it is based on a range of tests. MRI is required to rule out tumor growth and structural changes that compromise CSF drainage. It also aids in the diagnosis by detecting, for example, flattening of the posterior sclera, empty sella turcica, or enlargement of the perioptic subarachnoid space, which occur in 80%, 70%, and 45% of patients, respectively. A CSF sample is essential for both headache relief and laboratory analysis. When collecting CSF, normal constituents and an opening pressure of >25 cmH2O should be observed in adults. Other essential tests are fundoscopy and VF, which are indispensable to assess visual impairment. In patients with IIH, symptoms such as headaches, nausea, and vomiting are common. To confirm the diagnosis, the absence of other causes of increased intracranial pressure is also necessary2,5,8.
Patients with IIH have a doubled risk of cardiovascular diseases, regardless of obesity8. The purpose of IIH treatment is to decrease intracranial pressure, but not understanding the etiopathogenic mechanism prevents specific treatment. The classic close relationship between this disease and obesity is well known, especially in young women who have recently gained weight, but it can also occur in men, children, non-obese adults, and the elderly1,6. The patient in this report was 53 years old, menopausal, and on hormone replacement therapy. Thus, a weight loss program involving diet, exercise, and behavioral intervention is required and should be encouraged in such patients in addition to drug treatment to reduce CSF production10,11.
Acetazolamide, a carbonic anhydrase inhibitor, is considered the first line of treatment for IIH. It plays an important role in decreasing the production of CSF in the choroid plexus, thereby reducing intracranial pressure1,10. In patients refractory to clinical treatment, surgery, such as ventriculoperitoneal shunts, optic nerve fenestration, and stent placement, becomes indispensable5.
The diagnosis of IIH in this case was made based on the clinical presentation and case progression as well as on laboratory and imaging tests. The patient was female and obese, had a headache, was conscious and aware, and campimetry revealed visual alterations. Skull MRI revealed flattening of the posterior sclera in the OU and the absence of deformity, displacement, ventricular system obstruction, or expansive masses. The parasellar micromeningioma and lacunar infarcts evidenced on MRI because of their locations and small sizes do not cause obstruction and chronic intracranial hypertension or campimetry changes. The CSF contained normal constituents and had an initial pressure of 41 cmH2O. Because no other cause of increased intracranial pressure was identified and because it was a diagnosis by exclusion, the case was elucidated. In addition, even with the implementation of drug treatment, failure to follow the advice on weight loss resulted in a worsening of the condition, requiring ventriculoperitoneal shunting. After the procedure, the patient’s vision and headache improved, confirming the diagnosis.
Understanding the ophthalmologic and systemic clinical picture is critical for the investigation, follow-up, and early treatment of IIH, leading to an excellent outcome2. Based on the above findings, a thorough investigation of suspected cases of chronic IIH is important, especially in the absence of papillary edema seen in acute cases. Clinical treatment should focus on preventing or stabilizing visual loss, and the active involvement of both an ophthalmologist and a neurologist in the diagnosis, monitoring, and treatment of this disorder is critical.
REFERENCES
1. Portes ALF, Ramos CDVF, Nunes JS, Valdetaro R, Monteiro MLR. Hipertensão intracraniana idiopática de apresentação atípica com papiledema unilateral. Rev Bras Oftalmol. 2009;68(3):168-74.
2. Monteiro MLR, Moura FC. Aspectos oftalmológicos da síndrome da hipertensão intracraniana idiopática (pseudotumor cerebral). Rev Bras Oftalmol. 2008;67(4):196-203.
3. Wall M. Update on Idiopathic Intracranial Hypertension. Neurol Clin. 2017;35(1):45-57.
4. Boyter E. Idiopathic intracranial hypertension. JAAPA. 2019; 32(5):30-5.
5. Tiveron CCBL, Medeiros LA. Tratamento clínico da hipertensão intracraniana benigna idiopática (HII): relato de caso. Braz J Dev. 2021;7(4):41717-22.
6. Thurtell MJ, Bruce BB, Newman NJ, Biousse V. An update on idiopathic intracranial hypertension. Rev Neurol Dis. 2010; 7(2-3):e56-e68.
7. Madriz Peralta G, Cestari DM. An update of idiopathic intracranial hypertension. Curr Opin Ophthalmol. 2018;29(6):495-502.
8. Wakerley BR, Mollan SP, Sinclair AJ. Idiopathic intracranial hypertension: update on diagnosis and management. Clin Med. 2020;20(4):384-8.
9. Monteiro MLR. Perda visual na síndrome do pseudotumor cerebral. Arq Bras Oftalmol. 1994; 57(2):122-5.
10. Ahmad SR, Moss HE. Update on the Diagnosis and Treatment of Idiopathic Intracranial Hypertension. Semin Neurol. 2019; 39(6):682-91.
11. Koc F, Isik MR, Sefi-Yurdakul N. Weight reduction for a better visual outcome in idiopathic intracranial hypertension. Arq Bras Oftalmol. 2018;81(1):18-23.
AUTHOR’S INFORMATION






Funding: No specific financial support was available for this study
Approved by the following research ethics committee: Universidade de Santo Amaro – UNISA (CAAE: 53327621.3.0000.0081).
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
June 1, 2022.
Accepted on:
August 23, 2022.