Juliana Angélica Estevão de Oliveira1; Alice Novato Saraiva Silva1; Mariluze Maria Souza Sardinha2
DOI: 10.17545/eOftalmo/2022.0017
ABSTRACT
Orbital emphysema is a condition that involves accumulation of air/gas in the orbit. It is often associated with blowout fracture of an orbital bone due to its communication with paranasal sinuses. This article reports a rare case of orbital emphysema in the absence of trauma, following forceful nose-blowing. A detailed anamnesis and a careful physical examination, accompanied by imaging studies, are essential to clarify diagnosis and pathophysiological mechanism. In most cases, orbital emphysema is a benign condition and resolves spontaneously within 2 weeks. However, it can evolve with signs of orbital compartment syndrome such as reflective afferent pupillary defect, elevated PIO, significant proptosis and visual compromise. This syndrome is an ophthalmologic emergency that requires immediate management through air puncture or lateral orbital canthotomy and cantholysis to avoid serious complications.
Keywords: Emphysema; Orbit; Ethmoid bone; Orbital fractures; Spontaneous fractures.
RESUMO
O enfisema orbital (EO) é uma condição que envolve o acúmulo de ar/gás na órbita. Está frequentemente associado à fratura por explosão de um osso orbital devido à sua comunicação com os seios paranasais. Este artigo relata um caso raro de enfisema orbital na ausência de trauma, decorrente de uma forte assoada de nariz. Anamnese detalhada e exame físico cuidadoso, acompanhados de estudos de imagem, são essenciais para esclarecer o diagnóstico e o mecanismo fisiopatológico. Na maioria dos casos, o enfisema orbital é uma condição benigna e resolve-se espontaneamente dentro de 2 semanas. Contudo, pode evoluir com sinais de síndrome compartimental orbitária, tais como defeito pupilar aferente reflexivo, pressão intraocular (PIO) elevada, proptose significativa e comprometimento visual. Esta síndrome é uma emergência oftalmológica que requer intervenção imediata através de punção de ar ou cantotomia orbital lateral e cantólise para evitar complicações graves.
Palavras-chave: Enfisema; Órbita; Osso etmoide; Fraturas orbitais; Fraturas espontâneas
INTRODUCTION
Orbital emphysema (OE) is a rare condition involving accumulation of air/gas within the orbit1,2. It is often associated with blowout fracture of an orbital bone, mainly of the medial wall, by blunt trauma due to its communication with paranasal sinuses2,3. Although emphysema is extremely rare in the absence of trauma, nontraumatic OE due to coughing, sneezing, nose blowing, as a complication of ophthalmologic, otolaryngologic and dental procedures and infection by gas producing microorganisms have been described1,2. This article reports a case of OE following a spontaneous fracture of the papyraceous lamina of the ethmoid bone. Regardless of a history of trauma, early recognition of OE is crucial to prevent possible vision-threatening complications related to orbital compartment syndrome2,3.
CASE REPORT
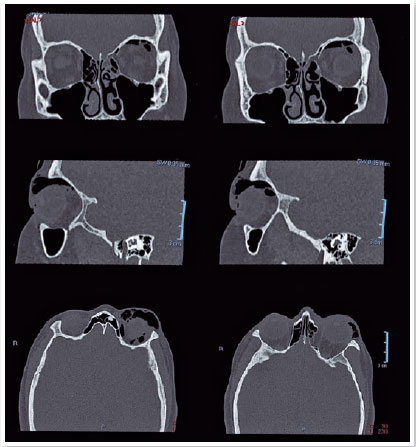
A 23-year-old healthy female patient was admitted at emergency department with a sudden and painless left periorbital swelling following forceful nose-blowing. Ophthalmologic examination revealed swollen upper left eyelid with crepitus at palpation, mechanical ptosis, mild conjunctival hyperemia, hypotropia and limitation of supraduction in the left eye (OS) (Figure 1). Pupils were equal and reactive to light, visual acuity (VA) was 20/20 in both eyes (OU), intraocular pressure (IOP) was 10mmHg in OU and fundoscopy showed no abnormal findings in OU. Orbital computed tomography (CT) revealed orbital and subcutaneous emphysema and fracture of the papyraceous lamina of the left ethmoid bone (Figure 2). As there were no sign of orbital compartment syndrome, the patient was treated conservatively. After 7 days, the patient became asymptomatic and evolved with complete regression of the condition (Figure 3).
DISCUSSION
OE occurs as a complication of orbital fractures involving any of the paranasal sinuses4 and it is a rare condition in the absence of trauma2. This case describes a spontaneous OE caused by forceful nose-blowing. Concomitant conditions, such as mucosal tears and acute elevated intranasal pressure causes a defect in the lamina papyracea, creating a passage of air from the sinus ethmoid into the orbital cavity and subcutaneous tissue4-6. Orbital fat creates a ball valve system by obstructing the exit of air from the orbit1,4. This condition is usually observed in elderly people since the bones are more predisposed to fracture2. Our patient was young and healthy, which may pose a diagnostic challenge. The most important differential diagnosis of OE in nontraumatic cases is orbital cellulitis, which may contain chemosis, visual loss, pain on eye movement and fever, besides the unilateral eye swelling1,7.
A detailed anamnesis and a physical examination are essential in patients with acute increased orbital volume8, including inspection and palpation of the affected region6. The presence of subcutaneous eyelid crepitus and subconjunctival air bubbles are significant clinical signs for diagnosis6. Also, evaluation of ocular motility, visual acuity, light reflex, intraocular pressure and fundoscopy are mandatory to judge if a urgent management will be necessary3. The clinical manifestations can vary from a short increase in eyelid volume to proptosis, diplopia, eye pain or complete vision loss6.
CT is useful in locating intraorbital contents and can provide the origin of the gas collections, the pathophysiological mechanism and clinical findings1,7. The site of OE can be categorized into five compartments: the periorbital subcutaneous (anterior to the orbital septum), peribulbar, intraconal retrobulbar, extraconal retrobulbar and pterygopalatine fossa, all posterior to the orbital septum. The post septal OE is associated with more serious injuries, including lesion of the optic nerve4.
In most cases, OE is a benign condition and resolves spontaneously in about 2 days to 2 weeks with only conservative treatment4,5. There is no consensus regarding antibiotic prophylaxis, and it is usually indicated in cases of contaminating lesions, the presence of sinusitis or immunosuppressed patients7. Patients should be instructed to avoid nose blowing3.
However, extreme caution is necessary due to possible complications resulting in vision loss, such as elevated IOP, optic neuropathy and ischemia of the central retinal artery2, secondary to high retrobulbar pressure and acute orbital compartment syndrome1. In such instances, immediate management is essential, including air drainage with a syringe, a simple and quick procedure that can avoid surgical intervention3,9. If this is not effective, lateral orbital canthotomy and cantholysis (LOC) may be done for orbital decompression2. Orbital compartment syndrome is a serious ophthalmologic emergency, and all emergency clinicians should be able to diagnose this condition and comprehend the LOC procedure in attempting to prevent vision loss10. Surgical intervention can also be determined based on IOP, fundoscopy and reflective afferent pupillary defects tests on those patients who do not cooperate with visual acuity test1.
In some cases, medial orbital wall fracture can leave some important complications, such as extraocular muscle restriction, diplopia and enophthalmos, and further reduction of the fracture is warranted2,3. However, orbital fracture reduction can be delayed as retrobulbar pressures can get out through the fracture site2.
Our patient presented with severe orbital emphysema on CT, but there was no globe tenting or clinical signs of orbital compartment syndrome. The visual acuity was preserved, the IOP was normal, and she had a normal pupillary reaction, indicating an intact optic nerve function. As she evolved with a dramatic improvement on follow up, medical or surgical intervention was not necessary.
In conclusion, physicians should know how to identify a case of orbital emphysema and orbital fracture. For this, a complete anamnesis and a careful physical examination, accompanied by imaging studies, are essential to make the precise diagnose and avoid serious complications. Once diagnosed, the management varies from simple observation to needle aspiration or even bone decompression, if necessary.
REFERENCES
1. Ariyoshi Y, Naito H, Yumoto T, Iida A, Yamamoto H, Fujisaki N, Aokage T, Tsukahara K, Yamada T, Mandai Y, Osako T, Nakao A. Orbital Emphysema as a Consequence of Forceful NoseBlowing: Report of a Case. Case Rep Emerg Med. 2019 Jun 18; 2019: 4383086.
2. Sarbajna T, Valencia MRP, Kakizaki H, Takahashi Y. Orbital Blowout Fracture and Orbital Emphysema caused by Nose Blowing. J Craniofac Surg. 2020;31(1):e82-e84.
3. Dong QN, Ide T, Karino M, Okuma S, Koike T, Kanno T. Retrobulbar Orbital Emphysema Associated with Medial Orbital Wall Fracture. J Craniofac Surg. 2019;30(5):1549-1551.
4. van Issum C, Courvoisier DS, Scolozzi P. Posttraumatic orbital emphysema: incidence, topographic classification and possible pathophysiologic mechanisms. A retrospective study of 137 patients. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115(6):737-42.
5. Islamoglu Y, Mulazimoglu S, Ozgursoy O. Unilateral orbital emphysema after nose blowing. Cukurova Medical Journal 2014;39(4):876-879.
6. Muñoz GS, Ríos BR, Rodríguez OM, Palma DC, Zúñiga GP. Enfisema orbitario espontáneo tras la maniobra de Valsalva. Revista Médica de Chile. 2015;143(2), 257-261.
7. Solanas-Álava S, Rodríguez-Marco NA, Artigas-Martín JM, Fernández-Larripa S. [Orbital emphysema: radiologic and ophthalmologic findings]. Emergencias. 2017;29(2):122-125. Spanish.
8. Slavsky A, Fraga J, Frea GG, Ronchetti MP, Miauro J, Castagna A, et al. Fractura de etmoides como diagnóstico diferencial de celulitis orbitaria en pediatría: caso clínico / Ethmoidal/fracture: differential diagnosis of orbital cellulites in pediatrics: clinical case. Arch Argent Pediatr. 2010;108(5):e118-e120.
9. Furlani BA, Diniz B, Bitelli G, Martins EM. Enfisema orbitário compressivo após asseio nasal: relato de caso. Arquivos Brasileiros de Oftalmologia [online]. 2009; 72(2):e251-e253
10. Desai NM, Shah Su. Lateral Orbital Canthotomy. [Updated 2021 Jan 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557476/
AUTHOR’S INFORMATION


Funding: No specific financial support was available for this study
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
July 11, 2022.
Accepted on:
August 23, 2022.