Lara Lopes de Almeida; Juliana Senna Figueiredo Barbi; Raianda Maia Alkmim da Costa; Tiago Augusto da Silva Moura; Felipe Leão de Lima
DOI: 10.17545/eOftalmo/2022.0015
ABSTRACT
This is a clinical case of a patient who presented with chronic conjunctivitis, and the cause was determined to be a foreign body reaction to a scleral introflexion band after several diagnostic hypotheses. It was decided to remove the band, and consequently, the symptoms improved overall.
Keywords: Pyogenic granuloma; Scleral curvature; Foreign body reaction.
RESUMO
Trata-se de caso clínico de paciente que apresentou um quadro de conjuntivite crônica, que após diversas hipóteses diagnósticas, atribui-se a causa à reação de corpo estranho à faixa de introflexão escleral. Foi optado pela remoção da faixa com melhora completa dos sintomas.
Palavras-chave: Granuloma piogênico; Recurvamento da esclera; Reação a corpo estranho
INTRODUCTION
The scleral introflexion band is a common procedure in the treatment of rhegmatogenous retinal detachment. It may be rarely associated with complications and requires removal in 1%-24% of cases. There are numerous indications for band removal, which include exposure, extrusion, migration of the band elements, intrusion, infection, chronic pain, inflammation, foreign body sensation, strabismus, diplopia, recurrent subconjunctival hemorrhage, macular distortion, swelling of the elements of the scleral introflexion band, and granuloma. Approximately 15% of the complications are related to chronic conjunctival irritation, which is regarded as a differential diagnosis of chronic conjunctivitis1-³.
Chronic conjunctivitis lasts more than 4 weeks and can be classified in terms of the causal agents as follows: infectious, toxic, allergic, or inflammatory or secondary to eyelid abnormalities (floppy eyelid or lagophthalmos)4.
In the case of a chronic condition, it is important to exclude differential diagnoses such as Parinaud’s oculoglandular conjunctivitis, “silent” dacryocystitis, conjunctival tumors (pyogenic granuloma, papilloma, or lymphoma), and autoimmune diseases (reactive arthritis, sarcoidosis, or discoid lupus erythematosus)4.
The following is a case of scleral introflexion band reaction that presented as chronic conjunctivitis with granulomatous reaction and was treated for several years before its diagnosis was explained.
CASE REPORT
A 72-year-old Caucasian female patient with GCH presented to the emergency department of Fundação Hilton Rocha with a long-standing complaint of conjunctival hyperemia, tearing, and eyelid edema in the left eye (LE).
She reported a history of vitreoretinal surgery in the LE for retinal detachment 8 years ago and a re-approach for retinal detachment 7 years ago.
When the patient’s chart was examined, there was no mention of the use of a scleral introflexion band during surgical procedures. With several different approaches, there were numerous consultations at the emergency department with complaints of conjunctival hyperemia, tearing, eye discharge, eyelid edema, and pain. There was no relief of symptoms after treatment for viral, bacterial, and allergic conjunctivitis and episcleritis.
The patient was referred to the eye plastic surgery department for her case investigation.
Eye examination findings:
CVA: 20/20 OD and LP OS.
Biomicroscopy: right eye without alterations.
LE: mild eyelid edema; a diffuse reddish granulomatous lesion distributed in the upper third of the bulbar conjunctiva; fornix; superior tarsal conjunctiva with the presence of perilesional vessels (Figure 1); transparent cornea; fluoride: negative; anterior chamber: free, no reaction; opacified intraocular lens.
Fundoscopy revealed no abnormalities in the right eye.
LE: unfeasible owing to media opacity.

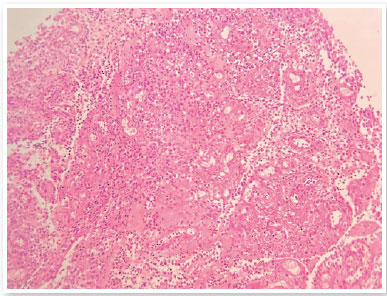
An incisional biopsy of the superior bulbar conjunctiva was performed, and the diagnosis was as follows: conjunctival lesion consisting of ulcerated granulation tissue, containing a dense granulomonuclear inflammatory infiltrate and edema and the absence of cancerous signs (Figure 2).
An evaluation was requested from the retina department because the lack of a description of the use of the scleral introflexion band in the medical records led to the diagnostic hypothesis of silicone oil leakage into the sub-tenon space as a result of vitrectomy. During this evaluation, the presence of a scleral introflexion band was observed, supporting the hypothesis of a foreign body reaction to the band.
The band was removed, and 30 days after surgery, there was a significant improvement in the inflammatory condition, resolution of the granulomatous process, and resolution of the symptoms reported by the patient (Figure 3).

DISCUSSION
Pyogenic granuloma is a vascular tumor that develops in the mucosa or skin, resembling a hyperplastic nodular lesion, and is caused by irritation, physical trauma, or hormonal factors. Most ophthalmologic reports of granulomas are related to chalazion or strabismus surgeries, but there are cases of spontaneous onset5.
For several years, the patient received different treatments for conjunctivitis, delaying her diagnosis. When referred to the eye plastic surgery department, three diagnostic hypotheses were proposed: conjunctival neoplasia, including squamous cell carcinoma of the conjunctiva and lymphoma; Parinaud’s oculoglandular syndrome; and an inflammatory reaction to silicone oil leakage into the subconjunctival space or the scleral introflexion band itself. Because the lesion was well located in the upper bulbar region, a biopsy was performed to rule out neoplasia. The presence of conjunctival granuloma suggested that it was a band reaction caused by topical corticosteroids that limited the inflammation area to the superior scleral introflexion region.
In this case, one of the reasons for delayed diagnosis was that the inflammatory lesion, despite being located in the upper bulbar region, was not observed in the silicone band region alone. The lesion occurred only after the use of topical steroids.
Because it concerns an unusual case with an atypical presentation, this report may be useful for the casuistry of this type of complication after vitreoretinal surgery as a differential diagnosis in cases of chronic conjunctivitis in patients undergoing this procedure.
REFERENCES
1. Covert DJ, Wirostko WJ, Han DP, Lindgren KE, Hammersley JA, Connor TB, et al. Risk factors for scleral buckle removal: a matched, case-control study. Am J Ophthalmol. 2008;146(3):434-9.
2. Roldán-Pallarés M, del Castillo Sanz JL, Awad-El Susi S, Refojo MF. Long-term Complications of Silicone and Hydrogel Explants in Retinal Reattachment Surgery. Arch Ophthalmol. 1999;117(2):197-201.
3. Deutsch J, Aggarwal RK, Eagling EM. Removal of scleral explant elements: a 10-year retrospective study. Eye (Lond). 1992;6 (Pt 6):570-3.
4. Mushlin SB, Greene HL. Decision Making in Medicine. 3rd ed. Philadelphia: Mosby Elsevier; 2010. 768 p
5. Damasceno EF, Pereira C, Damasceno NAP, Horowitz SAP, Amaral Filho OMB. Pyogenic granuloma after retinal detachment surgery with scleral buckle: case report. Arq Bras Oftalmol. 2009; 72(4):543-4.
AUTHOR’S INFORMATION



Funding: No specific financial support was available for this study
Conflict of interest: None of the authors have any potential conflict of interest to disclose
Received on:
June 24, 2021.
Accepted on:
August 31, 2022.