Andrea Mara Simões Torigoe; Gustavo de Carvalho Pazeto; Ahmad Mohamad Ali Hamade; Ricardo Ramos Daoud Yacoub
DOI: 10.17545/eOftalmo/2022.0010
ABSTRACT
The choroid is the structure with the highest occurrence of ocular metastasis. The sites that most commonly metastasize to the choroid are the lung and breast, with lung carcinoma responsible for about 30% of choroidal metastases. We report a case of a female patient with choroidal metastasis in the left eye due to pulmonary adenocarcinoma. The patient presented low visual acuity with the presence of a mass in the upper temporal region, endophytic, irregular and non-pigmented, associated with a detachment of sensorineural retina. It was conducted with the immunomodulator Gefitinib, a drug class of tyrosine kinase inhibitors. After 03 months using the medication, the patient showed improvement in visual symptoms, and marked regression of the lesion in the left eye. The result shows the benefit of this medication in a patient with this specific type of tumor.
Keywords: Choroidal metastasis; Gefitinibe; Lung adenocarcinoma
RESUMO
A coroide é a estrutura de maior ocorrência de metástase ocular. Os sítios que mais comumente metastatizam para a coroide são o pulmão e mama, sendo o carcinoma pulmonar responsável por cerca de 30% das metástases coroidais. Relatamos o caso de uma paciente do sexo feminino com metástase coroidal em olho esquerdo por adenocarcinoma pulmonar. A paciente apresentou baixa da acuidade visual com a presença de massa em região temporal superior, endofítica, irregular e não-pigmentada, associada a um descolamento de retina neurossensorial. Foi conduzida com o imunomodulador Gefitinibe, um medicamento classe dos inibidores da tirosina quinase. Após 03 meses em uso da medicação, a paciente apresentou melhora dos sintomas visuais, e acentuada regressão da lesão em olho esquerdo. O tratamento evidencia o benefício da medicação em paciente com este tipo específico de tumor.
Palavras-chave: Metástase coroidal; Gefitinibe; Adenocarcinoma pulmonar
INTRODUCTION
The choroid is the most frequent ocular site of metastases occurrence1, and other sites include the ciliary body, the iris, the neural retina, the optic nerve, and, in some cases, the vitreous2. In addition, only 25% of such cases are identified as the primary tumor site at diagnosis2.
The most common sites for cancers to metastasize to the choroid include the lung and breast1,3, with lung carcinoma accounting for approximately 30% of choroidal metastases. Symptoms such as blurred vision, visual field loss and/or decreased visual acuity are the most frequent visual symptoms2,3 and are typically some of the first symptoms to appear.
In addition to the more frequent occurrence of ocular metastasis in patients with adenocarcinoma, high serum levels of biomarkers-carcinoembryonic antigen (CEA), cancer antigen 15-3 (CA15-3), and total prostate-specific antigen (PSA)-would have a positive predictive value for ocular metastasis in older adults4.
In Brazil, approximately 70% of cases present with locally advanced or metastatic disease at the time of diagnosis5. Although lung cancer represents the main cause of mortality among neoplasms6,7, two-thirds of secondary choroidal metastases show favorable responses to different systemic or ocular treatments, promoting early diagnosis and treatment and consequently increasing the patient’s quality of life.
Systemic chemotherapy is more effective in the treatment of ocular metastases, especially in chemosensitive tumors, such as small-cell carcinoma2. Regarding cases of non-small-cell neoplasia, several case reports have reported the reversal of choroidal metastasis through the administration of bevacizumab, an anti-vascular endothelial growth factor (anti-VEGF)8-10. Chemotherapy, photocoagulation, cryosurgery, and surgical resection are among the options currently available for ocular metastases2.
The occurrence of ocular metastasis is higher in patients with advanced disease and in cases of adenocarcinoma; histological type that became the most frequent in the last 15 years2. These two characteristics associated with the improvement in survival obtained from the new therapeutic modalities, targeted molecular therapy, and immunotherapy11, suggest that newly diagnosed patients could benefit from a routine screening for ocular metastasis.
Gefitinib is a selective inhibitor of epidermal growth factor receptor (EGFR) tyrosine kinase, which is commonly expressed in human solid tumors of epithelial origin. Inhibition of EGFR tyrosine kinase activity inhibits tumor growth, metastasis and angiogenesis, increasing apoptosis of tumor cells12.
The objective of this report is to present a case where a choroidal metastasis associated with lung adenocarcinoma was resolved with the use of systemic gefitinib.
CASE REPORT
A 60-year-old female patient, asymptomatic, during routine chest X-ray examinations, a mass in her left lower lobe of the lung (LLL) was observed. The patient had no comorbidities and denied smoking. The positron emission tomography–computed tomography (PET-CT) performed in the sequence showed a pulmonary mass measuring 5.0 × 4.0 × 3.5 cm in the LLL and mediastinal lymph nodes in subcarinal, inferior and bilateral paratracheal chains, in the left inferior pulmonary ligament and descending thoracic aortic and lymph node in the left pulmonary hilum. She underwent LLL lobectomy and drainage of mediastinal lymph nodes in another service.
Pathological examination revealed lung adenocarcinoma (NSCLC), pathological staging pT2b pN2. The search for EGFR mutation (activating mutation of epidermal growth factor receptor) was positive for exon 19 deletion and lack mutations in KRAS, NRAS, BRAF, and ALK genes. For PDL-1 search, an expression of 30% was observed.
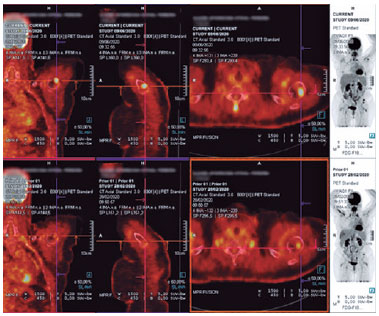
After surgery, the patient was referred to the Oncopneumology Service of HC Unicamp for adjuvant treatment (4 cycles of carboplatin+paclitaxel and sequential radiotherapy in mediastinum 4500 cGy 3D). PET-CT post chemotherapy showed ground-glass opacities and interlobular interstitial thickening in the left upper lobe (LUL), corresponding to post-radiotherapy pneumonitis.
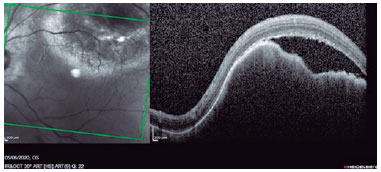
One year after the end of chemotherapy, she presented with the recurrence of a hyper-captivating pulmonary mass in the middle lobe. The patient experienced holocranial headache and blurred vision, associated with photopsias. Cranial tomography showed no alterations; however, retinal mapping showed a subretinal macular lesion with whitish appearance, elevated with approximately 10 papillary diameters of the superior temporal region. Visual acuity in the right eye of 20/20, without significant injuries; and visual acuity of 20/50 in the left eye, associated with a solid, endophytic lesion, with irregular, hypochromic, delimitation in the superior temporal region measuring approximately 10 mm at the base on retinography and height of 2.8 mm on ultrasound, with the presence of inferior sectoral serous retinal detachment and absence of Kappa angle. Optical coherence tomography (OCT) showed sensorineural retinal detachment, with perifoveal involvement and choroidal bulging in the superior temporal region, with compression of the external retina (Figure 1).
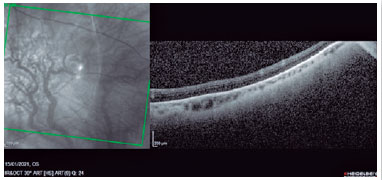
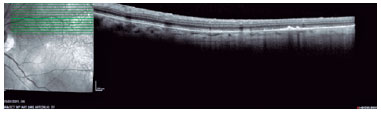
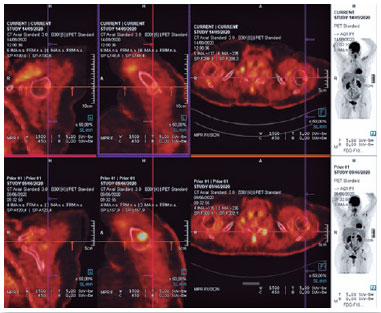
Owing to the progression of metastatic disease, gefitinib 250 mg/day was introduced. After 03 months using gefitinib 250 mg, the patient had improvement in visual symptoms, recovery of visual acuity to 20/20 and marked regression of the left eye lesion, with superior temporal focal alteration of the retinal pigment epithelium, without signs of activity, with OCT of the lesion area showing atrophy of the cystic spaces of the Satler and Haller layers, but maintenance of the integrity of the outer and inner retinal layers and the ellipsoid zone. In a new PET-CT the disease remission was observed, with no metastatic lesions and no signs of active disease (Figures 2 a 5)
DISCUSSION
Systemic medications circulate freely through the choroid, not being involved in the blood-retinal barrier, owing to the choroidal capillaries, but the effectiveness of chemotherapeutic agents depends on tumor susceptibility8. The prompt response to metastatic control, with a single treatment using gefitinib, for patients with EGFR mutation has shown excellent and surprising responses13.
In the present case, we demonstrated a complete remission of ocular metastasis in a patient with EGFR mutation exon 19 deletion, resulting in excellent quality of life. Recent studies have shown that gefitinib prolongs disease-free survival, preserving a favorable quality of life13,14.
Female patients or of Asian ethnicity who have never smoked, with adenocarcinoma histology, are more likely to benefit from gefitinib treatment13. These clinical features are also associated with high rates of EGFR13 mutation-positive tumors and are those found in the reported case.
Other treatment options for ocular choroidal metastases described in the literature include external beam radiotherapy, brachytherapy, laser, and photodynamic therapy15.
In conclusion, in this case report, we demonstrated the surprising effectiveness in resolving choroidal metastasis of lung adenocarcinoma in a patient with EGFR mutation. We believe that to avoid irreversible impairment or visual loss, screening tests should be performed early, in cases of breast and lung cancer for the early diagnosis and treatment of ocular metastases.
REFERENCES
1. Kreusel K, Wiegel T, Stange M, Bornfeld N, Hinkelbein W, Foerster M. Choroidal metastasis in disseminated lung cancer: frequency and risk factors. Am J Ophthalmol. 2002;134(3):445-7.
2. Lampaki S, Kioumis I, Pitsiou G, Lazaridis G, Syrigos K, Trakada G, et al. Lung cancer and eye metastases. Med Hypothesis Discov Innov Ophthalmol. 2014;3(2):40-4
3. Su H, Chen Y, Perng R. Symptomatic ocular metastases in lung cancer. Respirology. 2008;13(2):303-5.
4. Ge Q, Zou Y, Shi W, Zhang Y, Li B, Min Y, et al. Ocular Metastasis in Elderly Lung Cancer Patients: Potential Risk Factors of CA-125, CA-153 and TPSA. Cancer Manag Res. 2020;12:1801-1808.
5. Araujo L, Baldotto C, Castro Jr G, Katz A, Ferreira C, Mathias C, Mascarenhas E, Lopes GL, Carvalho H, Tabacof J, Martínez-Mesa J, Viana LS, Cruz MS, Zukin M, De Marchi P, Terra RM, Ribeiro RA, Lima VCC, Werutsky G, Barrios CH, Grupo Brasileiro de Ocologia Torácica. Lung cancer in Brazil. J Bras Pneumol. 2018;44(1):55-64.
6. Mathias C, Prado GF, Mascarenhas E, Ugalde PA, Gelatti ACZ, Carvalho ES, Faroni LD, Oliveira R, Lima VCC, Castro G Jr, Grupo Brasileiro de Oncologia Torácica. Lung Cancer in Brazil. J Thorac Oncol. 2020;15(2):170-175.
7. Herbst R, Morgensztern D, Boshoff C. The biology and management of non-small cell lung cancer. Nature. 2018; 553(7689):446-454.
8. Chen CJ, McCoy A, Brahmer J, Handa J. Emerging Treatments for Choroidal Metastases. Surv Ophthalmol. 2011;56(6):511-21.
9. Makabe K, Kurishima K, Shiozawa T, Miyazaki K, Ohara G, Kagohashi K, et al. Treatment of choroid metastasis from lung adenocarcinoma with bevacizumab-containing chemotherapy: A case report. Exp Ther Med. 2015;11(1):239-242.
10. Kim SW, Kim MJ, Huh K, Oh J. Complete Regression of Choroidal Metastasis Secondary to Non-Small-Cell Lung Cancer with Intravitreal Bevacizumab and Oral Erlotinib Combination Therapy. Ophthalmologica. 2009;223(6):411-3.
11. Arbour K, Riely G. Systemic Therapy for Locally Advanced and Metastatic Non–Small Cell Lung Cancer. JAMA. 2019;322(8):764-774.
12. Inoue M, Watanabe Y, Yamane S, Kobayashi S, Arakawa A, Tsukahara, T et al. Choroidal Metastasis with Adenocarcinoma of the Lung Treated with Gefitinib. Eur J Ophthalmol. 2010;20(5):963-5.
13. Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or Carboplatin–Paclitaxel in Pulmonary Adenocarcinoma. N Engl J Med. 2009;361(10):947-57.
14. Verduyn SC, Biesma B, Schramel FMNH, van der Scheer FW, Langenfeld MK, de Peuter MA, et al. Estimating quality adjusted progression free survival of first-line treatments for EGFR mutation positive non small cell lung cancer patients in The Netherlands. Health Qual Life Outcomes. 2012 Sepo10;10:108.
15. Schields JA, Shields CL. Intraocular Tumors an Atlas and Textbook, 3rd Edition. Lippincott, Williams & Wilkins. 2015.
AUTHOR’S INFORMATION




Funding: No specific financial support was available for this study
Conflict of interest: None of the authors have any potential conflict of interest to disclose
Received on:
July 19, 2022.
Accepted on:
August 8, 2022.