Thaís Mota Gomes; Gustavo David Ludwig; Eric Pinheiro de Andrade
DOI: 10.17545/eOftalmo/2022.0009
ABSTRACT
Horner’s syndrome, a disorder associated with ipsilateral damage to the sympathetic pathway, is a rare complication of cannulation into the internal jugular vein. Depending on the intensity of the injury and location, the damage may be irreversible, even in young children.
Keywords: Horner’s syndrome; Children, Sympathetic nerve; Injury; Jugular vein.
RESUMO
A síndrome de Horner, um distúrbio associado a lesão ipsilateral da via simpática, é uma complicação rara da canulação na veia jugular interna (VJI). Dependendo da intensidade da lesão e da localização, o dano pode ser irreversível, mesmo em crianças pequenas.
Palavras-chave: Síndrome de Horner; Crianças; Nervo simpático; Lesão; Veia jugular.
INTRODUCTION
Horner’s syndrome is classically described as a triad of miosis, blepharoptosis and anhidrosis, but may also be present enopthalmos, pseudo enophthalmos (due to ptosis of the upper lid and elevation of the lower lid), hyperemia of the cheek and iris heterochromia on the ipsilateral side of the lesion to sympathetic nerve along its course from the hypothalamus to the eye1.
In pediatrics, Horner’s syndrome is classified as congenital or acquired. The diagnosis is important for subsequent etiologic diagnosis by providing therapeutic measures and follow-up1,2.
Clinical evaluation and neuroimaging (CT/MRI and angiography) are essential to differentiate inflammatory, neoplastic or traumatic causes3.
We report a rare case of pediatric and complete Horner’s syndrome secondary to internal jugular vein cannulation where there was no regression of the sequelae even after one year.
CASE HISTORY
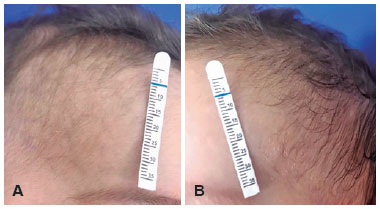
A seven-month-old boy, preterm twin, was examined to our institution two months after admission to another hospital for bronchiolitis. According to the mother, the child needed central venous access due to the impossibility of peripheral access for medication administration. Initially, peripherally inserted central catheters (PICC) was tried without success, so the centrally inserted venous catheters (ICRC) were chosen. A day later, the patient’s mother noticed her son’s right eyelid ptosis. An ophthalmologist has been consulted and the child was referred to neurophthalmology department. On examination: upper eyelid ptosis, facial anhidrosis (Figure 1), and miosis visible in scotopic environment [left pupil (4mm) greater than right (2mm) Figure 2] ipsilateral to the puncture site. Anisocoria was not shown in photopic environment. There were no alterations found both in the oculomotricity exam and biomicroscopy. The clinical evaluation concluded a diagnosis of Horner’s syndrome. Despite the history of ICRC suggesting a traumatic mechanism, the investigation with imaging exams was performed. Two months after placement of CVC, cerebral and cervical magnetic resonance imaging (MRI) with angiographic sequences, chest CT and VJID Doppler US was also normal. No ocular pharmacological tests or urine catecholamine testing were performed. Excluding neoplastic and inflammatory causes, traumatic lesion of oculo-sympathetic pathway was admitted. We concluded that it was a case of complete Horner’s Syndrome induced by mechanical trauma during IJV cannulation with damage to a second order neuron of the sympathetic nervous supply. Conservative management with periodic monitoring was carried out. One year after diagnosis, there is no evidence of visual impairment or damage to the patient’s psychomotor development when compared to other children of the same age group and his identical twin who does not have Horner’s syndrome.

DISCUSSION
Horner’s syndrome is classically known as unilateral blepharoptosis, miosis with variable degrees of facial anhidrosis and enophthalmos may also be presente. The syndrome results from ipsilateral interruption of the sympathetic innervation4,5.
In youngers the incidence of 1.42 per 100,000 had been estimated, where 40% were congenital, 42% were acquired after a surgical procedure in the thorax, neck, or central nervous system, and 15% were acquired from causes that included neuroblastoma, spinal cord tumors, rhabdomyosarcoma embryonal cell carcinoma, vascular malformations, intrathoracic aneurysm and trauma6.
In the present report, we demonstrate a case of pediatric Horner’s syndrome induced by a central venous catheter, caused by direct trauma. Similar cases have been reported, usually secondary to anatomic abnormalities or complications of puncture technique.
During PICC, a peripheral vein is punctured and a device passed until reaching the distal third of the superior vena cava or proximal third of the inferior vena cava. This technique is advantageous due to its lower cost, ease of catheterization and lower risk of infection, but it is not preferable if large volume of fluid is required. In this situation, as in the present case, a large central vein is directly accessed (ICRC). The right internal jugular vein is preferred in children because of the lower risk of pneumothorax and easier compression in case of hematomas. However, in this case, the injury to the sympathetic pathway may have occurred due to respiratory distress caused by the acute bronchiolitis, psychomotor agitation and difficulty in sedating the child during insertion. In addition, US was not used during the procedure, a non-mandatory resource, which would reduce the risk of complications.
The sympathetic trunk is closely related to the carotid sheath in its posterior wall and 18% of patients younger than six years have anomalous IJV anatomy, mostly IJV overlapping the carotid artery7. To avoid complications, the literature highlights factors that decrease the risk of damage to the sympathetic trunk: professional experience, patient positioning, sedation and use of ultrasound (USG). The right internal jugular vein (IJV) has several advantages as a cannulation site, having a predictable anatomy, even in children. Although the posterior approach is technically more difficult a 98% success rate of cannulation has been reported using the posterior approach in infants and children aged one day to 12 years8. Especially in pediatric cases, sedation is important to decrease psychomotor agitation.
The symptoms presented depend on the location of the sympathetic ocular pathway. In the exposed case, the presence of anhidrosis, absence of psychomotor damage or involvement of cranial nerve associated with the topography of the trauma suggests involvement in the second order neuron. The sympathetic nervous supply to the eye originates in the posterolateral hypothalamus. The first order neurons (central) descends to synapse, with second-order neurons at the ciliospinal center (Budge) between C8 and T1. These second order neurons (preganglionic fibers) pass over the pulmonary apex, ascend in the neck in the cervical sympathetic chain behind the common carotid artery outside the carotid sheath, ascend through the stellate and middle cervical ganglia and synapse with third order neurons (postgangionic) in the superior cervical ganglion, located at the angle of jaw1,3.
For confirmation diagnosis, localization of injury in the oculosympathetic pathway and etiologic elucidation, clinical evaluation, pharmacological and laboratory tests and neuroimage can be used. Especially in pediatric cases, ruling out malignancy is the main objective.
In this case, in which the clinical signs show a complete Horner’s syndrome initiated after ipsilateral trauma by IJV cannulation, no ocular pharmacological tests (cocaine, apraclonidine, or hydroxyamphetamine) or urine catecholamine testing were performed. The neuroimaging study was performed to exclude other injuries and to identify complications with the insertion of a central catheter that could justify the syndrome.
The most recent protocol for image investigation in Horner’s syndrome includes magnetic resonance imaging of the head, neck and upper chest, the angiogram of the neck vessels in suspected post ganglionic involvement or without probable cause. CT is mostly indicated if a traumatic injury of the skull base is suspected3,5.
George et al. recommend only images of the head, neck and chest for patients over one year of age at the time of presentation2. For patients under one year of age, they recommend urinary catecholamine and examination for cervical or abdominal masses, but Jeffery et al. mentions that abdominal investigation should be acquired in cases without known injury (that is, surgical or birth trauma)9.
Corroborating with the neuroimaging study carried out in the present report, Barrea et al state that history of trauma or surgery may reduce the need for extensive systemic evaluation5. However, it’s important make sure that require thorough evaluation should be imaged in patients in whom the clinical examination does not provide enough information to locate the lesion with certainty or there is no probable cause because of the frequent association of serious underlying disease.
Three months after IJV cannulation, maternal observation and clinical examination showed that the hair on the right side was smoother than the contralateral. During apresentation or evaluation, no enopthalmos, pseudo enophthalmos, hyperemia of the cheek or iris heterochromia have been reported. At 12 months of age, the child maintains right ptosis, miosis and anhidrosis with no resolution, but the hair is bilaterally curly. Other studies without neuroimaging changes with probable direct damage of the needle in the sympathetic trunk have had different results. A six-year-old child had regression of ptosis and miosis 18 days after developing Horner’s syndrome and a five-year-old boy had complete remission of the symptoms after five months3,5. In a younger child, seven-month-old, at the 12-month follow-up slight right eye ptosis could still be noticed and anisocoria was completely resolved10.
REFERENCES
1. Cahill JA, Ross J. Eye on children: acute work-up for pediatric Horner’s syndrome. case presentation and review of the literature. J Emerg Med. 2015;48(1):58-62.
2. George NDL, Gonzalez G, Hoyt CS. Does Horner’s syndrome in infancy require investigation? Br J Ophthalmol.1998;82(1):51-4.
3. Kadom N, Rosman NP, Jubouri S, Trofimova A, Egloff AM, Zein WM. Neuroimaging experience in pediatric Horner syndrome. Pediatr Radiol. 2015;45(10):1535-43.
4. Barrea C, Vigouroux T, Karam J, Milet A, Vaessen S, Misson JP. Horner syndrome in children: a clinical condition with serious underlying disease. Neuropediatrics. 2016;47(4):268-72.
5. Links DJR, Crowe PJ. Horner’s syndrome after placement of a peripherally inserted central catheter. JPEN J Parenter Enteral Nutr. 2006;30(5):451-2.
6. Smith SJ, Diehl N, Leavitt JA, Mohney BG. Incidence of pediatric Horner syndrome and the risk of neuroblastoma: a populationbased study. Arch Ophthalmol. 2010;128(3):324-9.
7. Alderson PJ, Burrows FA, Stemp LI, Holtby HM. Use of ultrasound to evaluate internal jugular vein anatomy and to facilitate central venous cannulation in paediatric patients. Br J Anaesth. 1993;70(2):145-8.
8. Chatrath RR, Stock JG, Jones OD. Internal jugular catheterisation in small children. The use of a posterior approach. Anaesthesia. 1983;38(4):380-3.
9. Jeffery AR, Ellis FJ, Repka MX, Buncic JR. Pediatric Horner syndrome. J AAPOS. 1998;2(3):159-67.
10. Knyazer B, Smolar J, Lazar I, Rosenberg E, Tsumi E, Lifshitz T, et al. Iatrogenic Horner Syndrome: Etiology, Diagnosis and Outcomes. Isr Med Assoc J. 2017;19(1):34-38.
AUTHOR’S INFORMATION

Funding: No specific financial support was available for this study
Conflict of interest: None of the authors have any potential conflict of interest to disclose
Received on:
July 5, 2022.
Accepted on:
August 2, 2022.