Danielle Ribeiro Brega1; Aline Mota Freitas Matos1; Maíra Costa Navais1; Marta Halfeld Ferrari Alves Lacordia1; Bianca Figueiredo Barczewski1; Raphael Defina1; Louise Gracielle de Melo e Costa2
DOI: 10.17545/eOftalmo/2022.0003
ABSTRACT
Primary Cutaneous Mucinous Carcinoma is a rare skin adnexal tumor and it most commonly affects the eyelids. This tumor presents low clinical suspicion, since it can simulate several benign eyelid lesions, which often leads to incorrect diagnosis and treatment, resulting in a worse prognosis. The authors describe a case of Primary Cutaneous Mucinous Carcinoma that initially presented itself mimicking a Moll’s cyst and after 6 months of the initial evaluation had significant growth with loss of eyelashes. The anatomopathological and immunohistochemical studies revealed the diagnosis of Primary Cutaneous Mucinous Carcinoma of the eyelid. This case highlights the importance of recognition and correct diagnosis of this tumor with appropriate treatment and follow-up. Although rare and indolent, it presents a high risk of local recurrence and the possibility of regional or distant metastases.
Keywords: Adenocarcinoma; Mucinous; Eyelid Neoplasms; Neoplasms; Adnexal and Skin Appendage.
RESUMO
O carcinoma mucinoso cutâneo primário é um tumor raro dos anexos cutâneos que acomete mais comumente as pálpebras. Este tumor apresenta baixa suspeição clínica, pois pode simular diversas lesões palpebrais benignas, o que muitas vezes leva a diagnóstico e tratamento incorretos, resultando em pior prognóstico. Os autores descrevem um caso de carcinoma mucinoso cutâneo primário que inicialmente se apresentou mimetizando um cisto de Moll e após 6 meses da avaliação inicial se demonstrou com crescimento significativo e perda de cílios. Os estudos anatomopatológico e imuno-histoquímico revelaram o diagnóstico de carcinoma mucinoso cutâneo primário de pálpebra. Este caso destaca a importância do reconhecimento e diagnóstico correto deste tumor com tratamento e acompanhamento adequados. Apesar de raro e indolente, apresenta alto risco de recorrência local e possibilidade de metástases regionais ou à distância.
Palavras-chave: Adenocarcinoma; Neoplasias mucinosas da pálpebra; Neoplasias de anexos cutâneos.
INTRODUCTION
Primary Cutaneous Mucinous Carcinoma (PCMC) is an extremely rare skin adnexal tumor, derived from sweat glands that produce extracellular pools of mucin1. It was first identified by Lenox et al in 19522 with approximately 350 cases reported in the literature so far3.
PCMC is most frequently located on the eyelids (38%) but may affect other sites on the face (20.3%), scalp (16%), and axilla (10%)4. It is characterized as a tumor of low grade of malignancy, presenting slow growth, without clinically distinctive features:5 it can simulate a chalazion, a papilloma, a simple cyst, a nevus, a pyogenic granuloma, hemangioma or other types of neoplasm5. Despite being considered an indolent tumor, its aspect may be mistaken for a benign pathology and the incorrect treatment can lead to poor prognosis since it has a recurrence rate between 26%-40%5 and even a few regional and distant metastases (11% and 3%, respectively)6.
Authors describe a case of PCMC of the eyelid that initially presented itself by mimicking a Moll’s cyst. Written informed consent from the patient was obtained for publication of the medical photography included in the article. The study adhered to the tenets of the Declaration of Helsinki and was submitted to and approved by the Ethics Committee.
CASE REPORT
A 50-year-old white man was referred to the ophthalmology clinic due to the presence of a lesion on his right eye with six months of evolution. He had a history of well controlled systemic arterial hypertension. Visual acuity was 20/25 in each eye and unremarkable slit-lamp exam. On the middle third of the right lower eyelid, there was a cystic lesion, measuring approximately 2-3 mm, suggestive of Moll’s cyst. There were two other lesions on the same eyelid, both with benign aspect, with approximately 1-2 mm each: one temporal, pedunculated and verrucoid, and the other one nasal, flat, with sebaceous appearance. The patient denied symptoms related to them. Preoperative exams were then requested for excision surgery.
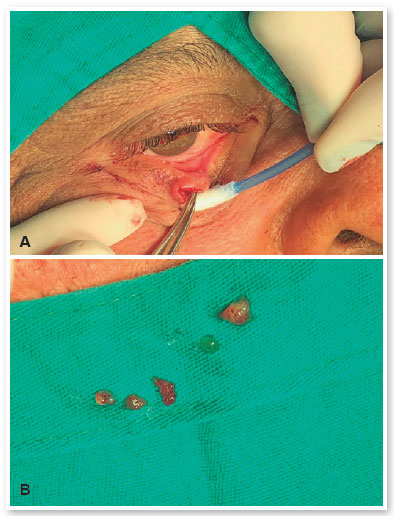
The patient returned 6 months later and the middle lesion had grown significantly, measuring 10 mm, with loss of eyelashes and causing mild ectropion. The two other adjacent lesions remained the same (Figure 1). An incisional biopsy of the middle lesion was then performed, revealing a gelatinous substance (Figure 2 A-B), and the other two were excised completely.

The anatomopathological examination confirmed that the temporal lesion was a verruca vulgaris. During the excision of the nasal lesion, it fragmented due to its cystic nature, and only keratin lamellae were seen in microscopic examination. The middle lesion consisted of a mucinous carcinoma, composed by blocks of cohesive eosinophilic cells with low pleomorphism and low-grade nuclear atypia, embedded in lakes of mucin (highlighted by special stain Alcian Blue) (Figure 3 A-C). The immunohistochemical analysis revealed that the tumor cells were positive for cytokeratin AE1/AE3, while negative for CDX2 (clone EPR2764Y), CEA (clone Il-7), and S100 (polyclonal). This panel in association with morphologic findings favored a PCMC.
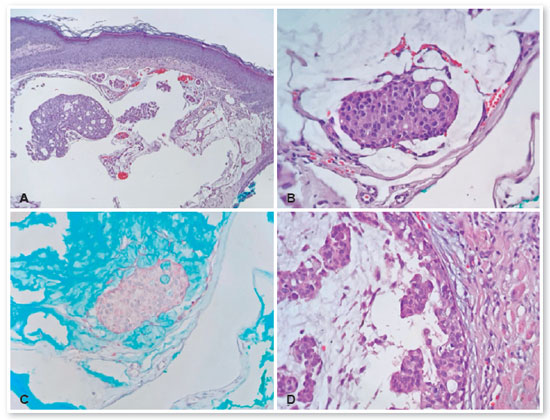
About four weeks later, surgical enlargement of margins was performed with reconstruction by a Tenzel rotation flap. The excised lesion showed the presence of mucinous carcinoma with an in situ component, and surgical margins were free of lesion (Figure 3D).
The patient was referred to the oncologist to exclude the possibility of other neoplasms. Based on the American Joint Committee on Cancer (AJCC), eighth edition, the staging of the tumor was T1cN0M07. The patient has been followed for 6 months without signs of local recurrence or metastasis of the lesion.
DISCUSSION
PCMC is a rare low-grade malignant skin adnexal tumor with a predilection for eyelid involvement. There are divergences in the literature about its origin, being historically classified as an eccrine tumor, although some authors have demonstrated apocrine differentiation2.
Our case was a fifty-year-old white man and illustrates the epidemiological profile described in the literature. PCMC occurs more commonly in men8,9, caucasian1, between the 5th and 7th decades of life8. However, there are some controversies in the literature, since some authors advocate that there is no sex predominance3.
Due to this variety of clinical presentations, the diagnosis of PCMC is almost always made on the basis of anatomopathological analysis5. It may present clinically as a nodular, pigmented, painless lesion, and may be ulcerated, crusted or with telangiectasia10, measuring 0.7-2.5 cm, with slow growth (with a duration of several months to several years)11. In our case, the lesion had a cystic aspect and mimicked a Moll cyst in the first evaluation. However, its rapid growth and loss of eyelashes raised the diagnostic hypothesis of a potential malignant lesion.
Microscopically, PCMC is characterized by nests, strands or individual units of relatively monomorphous neoplastic cells floating in pools of mucin, which are compartmentalized by delicate fibrous septa3,12. In about 60-70% of the cases, an in situ component - reminiscent of mammary intraductal proliferations - is seen3. Since the main differential diagnosis is metastatic adenocarcinoma or direct invasion from an underlying extra cutaneous neoplasm - mainly from the breast, gastrointestinal tract or ovary - finding an in situ component helps the pathologist to qualify the tumor as primary cutaneous. However, its absence does not preclude the diagnosis of PCMC. In such cases, a full clinical work-up is necessary and immunohistochemical examination can be helpful to establish the origin3,12. PCMCs typically express low-molecular-weight cytokeratin, EMA (epithelial membrane antigen), CEA (carcinoembryonic antigen) and E-cadherin. S100 protein expression is variable and they are CK7 positive and CK20 negative, in contrast to gastrointestinal lesions which characteristically express this keratin3,12. Since PCMCs and many breast cancers are ER (estrogen receptor), PR (progesterone receptor) and GCDFP15 (gross cystic disease fluid protein 15) positive, these markers are not useful in the differentiation between them12. Tumors appearing in the trunk are most likely derived from breast, while those arising in the eyelid are most certainly a primary lesion12. Our case lacked expression of CDX2, which is usually positive in gastrointestinal and ovarian mucinous carcinomas13, and showed an in situ component, making the diagnosis of PCMC more certain.
The treatment of this kind of tumor is surgical resection, because it is resistant to both chemotherapy and radiation14. Although Mohs Micrographic Surgery (MMS) has been recommended as the treatment of choice for conferring a lower rate of recurrences15, direct excision also has good results15. Other authors have also reported good results with lower margins1,16. In a recent systematic review, only 9.4% of 215 cases of PCMC were treated with MMS, while the majority was treated with traditional surgical excision (85.5%). Although the recurrence rate in this review was higher in the group treated with simple excision (34% versus 13% in MMS group), there was a bias of follow up (the MMC group was accompanied for a shorter time9). When performed by simple excision, the recommended margins are from 1 to 2 cm17, but this is not always feasible, especially in eyelid tumors.
In our case, MMS technique was not available. Therefore, the tumor was excised with an additional 3 mm margins from the initial scar and was considered free of malignant cells on histologic exam. The patient had no recurrence in the 6-month follow-up.
Despite being rare and mostly of an indolent course, PCMC can be rather aggressive locally. The correct recognition of it is important to ensure effective treatment and adequate follow-up.
REFERENCES
1. Tak MS, Cho SE, Kang SG, Kim CH, Kim DW.Primary Cutaneous Mucinous Carcinoma of the Eyelid. Arch Craniofac Surg. 2016;17(3):176-9.
2. Lennox B, Pearse AG, Richards HG. Mucin-secreting tumours of the skin with special reference to the so-called mixed-salivary tumour of the skin and its relation to hidradenoma. J Pathol Bacteriol. 1952;64(4):865-80.
3. Elder DE MD, Scolyer RA, Willemze R. Mucinous carcinoma. In: WHO Classification of Skin Tumours. Vol 11. 4th Edition ed. Lyon, France: International Agency for Research on Cancer; 2018.
4. Kazakov DV, Suster S, LeBoit PE, Calonje E, Bisceglia M, Kutzner H, et al. Mucinous carcinoma of the skin, primary, and secondary: a clinicopathologic study of 63 cases with emphasis on the morphologic spectrum of primary cutaneous forms: homologies with mucinous lesions in the breast. Am J Surg Pathol. 2005;29(6):764-82.
5. Zhang L, Ge S, Fan X. A brief review of different types of sweat-gland carcinomas in the eyelid and orbit. OncoTargets Ther. 2013 Apr 9;6:331-40.
6. Snow SN, Reizner GT. Mucinous Eccrine Carcinoma of the Eyelid. Cancer. 1992;70(8):2099-2104.
7. Esmaeli B DJ, Graue GF, et al. Carcinoma of the eyelid. In: Amin MB ES, Green FL, ed. AJCC Cancer Staging Manual. 8th ed. ed. New York, NY: Springer; 2017:377-380.
8. Marrazzo G, Thorpe RB, Black WH. Primary mucinous carcinoma of the eyelid treated with Mohs micrographic surgery. Cutis. 2017;100(5):e7-e10.
9. Kamalpour L, Brindise RT, Nodzenski M, Bach DQ, Veledar E, Alam M. Primary cutaneous mucinous carcinoma: a systematic review and meta-analysis of outcomes after surgery. JAMA Dermatol. 2014;150(4):380-4.
10. Scilletta A, Soma PF, Grasso G, Scilletta R, Pompili G, Tarico MS, et al. Primary cutaneous mucinous carcinoma of the cheek. Case report. G Chir. 2011;32(6-7):323-5.
11. Papalas JA, Proia AD. Primary Mucinous Carcinoma of the Eyelid A Clinicopathologic and Immunohistochemical Study of 4 Cases and an Update on Recurrence Rates. Arch Ophthalmol. 2010;128(9):1160-5.
12. McKee PH CE, Lazar A, Brenn T. Primary cutaneous mucinous carcinoma In: McKee’s Pathology of the Skin. 5th ed ed. Edinburgh: Elsevier/Saunders; 2020:1980.
13. Dabbs DJ. Immunohistology of Carcinoma of Unknown Primary Site. In: Diagnostic Immunohistochemistry. 5th Edition ed. Philadelphia, PA: Saunders/Elsevier; 2019:p. 243-244.
14. Burris CK, Rajan KD, Iliff NT. Primary mucinous carcinoma of the periocular region: successful management with local resections over 30 years. BMJ Case Rep. 2013 Feb 15;2013:bcr2012007972.
15. Baker MS, Yin VT, Ivan D, Allen RC, Carter KD, Esmaeli B, et al. Epidemiology and Prognosis of Primary Periocular Sweat Gland Carcinomas. Ophthalmic Plast Reconstr Surg. 2017;33(2):101-5.
16. Bindra M, Keegan DJ, Guenther T, Lee V. Primary cutaneous mucinous carcinoma of the eyelid in a young male. Orbit. 2005;24(3):211-4.
17. Cabell CE, Helm KF, Sakol PJ, Billingsley EM. Primary mucinous carcinoma in a 54-year-old man. J Am Acad Dermatol. 2003; 49(5):941-3.
AUTHOR’S INFORMATION





Funding: No specific financial support was available for this study
Approved by the following research ethics committee: Hospital Universitário da Universidade Federal de Juiz de For a (CAAE: 33950620.5.0000.5133)
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
October 8, 2020.
Accepted on:
June 1, 2022.