Bianca Diogo Lessa Castro1; Pedro Henrique de Santana Pereira1; Sandy Ester Freire Sobral1; Aline Lourenço Cordeiro1; Sarah Dibe Santos1; Ana Adélia Sá Costa1; Herculano Pontes Barros Ribeiro1; Lorena Ribeiro Ciarlini2; Ana Karenina Mazulo Ribeiro2; Juliana de Lucena Martins Ferreira1,2
DOI: 10.17545/eOftalmo/2021.0023
ABSTRACT
OBJECTIVE: To compare the findings of the ophthalmological evaluation performed by students in the last year of specialization in ophthalmology (R3) with that of an experienced glaucomatologist by taking into account the early findings of glaucomatous disease.
METHODS: A cross-sectional study involving patients screened for eye examination at Fundação Leiria de Andrade (Leiria de Andrade Foundation). This evaluation was first performed by the R3 students of the foundation specialization course and then repeated by the glaucoma preceptor.
RESULTS: Of the 25 patients examined by R3 students, 5 were suspected of having glaucoma, of which three were male and two were female, two were between 41 and 60 years old, and three were between 61 and 80 years old. Regarding gonioscopy, there was no patient with a closed angle. The mean intraocular pressure was 16.6 mmHg in the right eye and 15.8 mmHg in the left eye. Fundoscopy revealed a mean excavation/disc ratio of 0.74 × 0.74 in Oculus Dexter and 0.74v × 0.72h in Oculus Sinister.
CONCLUSIONS: The R3 students performed satisfactorily in suspecting glaucoma, of which two had a confirmed diagnosis of glaucoma and the remaining three were suspected of having increased constitutional excavation. However, the sample was insufficient to show statistical relevance.
Keywords: Glaucoma; Ophthalmology; Medical education; Thyroid diseases.
RESUMO
OBJETIVO: Comparar os achados da avaliação oftalmológica realizada por alunos do último ano (R3) de especialização em Oftalmologia com a avaliação de glaucomatólogo experiente, tendo em vista os achados precoces da doença glaucomatosa.
MÉTODOS: Estudo transversal envolvendo pacientes triados para exame oftalmológico na Fundação Leiria de Andrade. Esta avaliação era primeiramente realizada pelo R3 do curso de especialização da Fundação Leiria de Andrade e depois repetida pelo preceptor de glaucoma.
RESULTADOS: Dos 25 pacientes examinados pelos R3, cinco eram suspeitos para glaucoma, dos quais três eram do sexo masculino e dois do sexo feminino, dois apresentavam-se entre 41 e 60 anos e três entre 61 e 80 anos. Em relação à gonioscopia, não havia paciente com ângulo fechado. A pressão intraocular média foi de 16,6 mmHg em olho direito e de 15,8 mmHg em olho esquerdo. Fundoscopia revelava uma relação escavação/disco média de 0,74 x 0,74 em OD e de 0,74v x 0,72h em OE.
CONCLUSÕES: os R3 apresentaram desempenho satisfatório na suspeição do glaucoma, os quais dois deles tiveram diagnóstico confirmado de glaucoma e os três restantes possuíam suspeita por portarem escavação aumentada constitucional. No entanto, a amostra possuía tamanho insuficiente para demonstrar relevância estatística.
Palavras-chave: Glaucoma; Oftalmologia; Educação médica; Doenças da tireoide.
INTRODUCTION
Glaucomatous disease should be investigated in every ophthalmological evaluation, considering it to be a disease that often presents subclinically, even in the presence of neuropathy, in addition to presenting, an unfavorable prognosis with irreversible visual loss in the long term. Glaucoma consists of a progressive optic neuropathy, which evolves with the destruction of retinal ganglion cells, causing visual loss. Glaucoma is considered the leading cause of irreversible blindness, according to the World Health Organization. It has affected more than 67 million people worldwide, of which 10% are blind1-3.
The most common type is primary open-angle glaucoma (POAG) and the risk factor mostly associated with the evolution of this disease, besides being the only factor susceptible to modification, is the increase in intraocular pressure (IOP), due to several pathophysiologies. In addition, age over 40 years, increased optic nerve excavation, ethnicity (black for POAG and yellow for the primary closed angle glaucoma [PCAG]), family history, ametropia (myopia for POAG and hyperopia for PCAG), decreased ocular perfusion pressure, and genetic conditions are other risk factors associated with the development of glaucoma, and changes involving thyroid hormones are still controversial in the etiopathogenesis of the disease1-4.
Because glaucoma is an especially silent disease, many patients seek medical care in the later stages of the disease, where they already have serious impairment to their vision. IOP control minimizes the risk of damage to the optic nerve, consequently delaying the evolution of the disease. Thus, early identification and rapid referral to specialized centers are of elemental importance for a better prognosis of this disease5,6.
Therefore, in order to prevent unfavorable outcomes, it is fundamental to increase efforts in the areas of health education, medical specialization, and infrastructure, and the present study aims to compare the findings of the ophthalmologic evaluation of patients with thyroid disease performed by students in the last year of specialization in ophthalmology (R3) with the evaluation of an experienced glaucomatologist by considering the early findings of glaucomatous disease.
METHODS
The research followed the principles outlined in the Declaration of Helsinki and was previously submitted to Plataforma Brasil and approved by the Comitê de Ética em Pesquisa, CEP (Research Ethics Committee) under the numbers CAAE: 88276418.1.0000.5049 and 88875518.4.0000.5049, being part of a scientific initiation project at the Centro Universitário Christus, UNICHRISTUS (Christus University Center).
This was a cross-sectional study conducted between August 2018 and March 2019, with patients with thyroid disease followed at the outpatient clinic of the Clínica Escola de Saúde da Unichristus (UNICHRISTUS Health Clinic) in Fortaleza-Ceará-Brazil. Individuals were screened by medical students through electronic medical records and approached by them via telephone call to perform a complete ophthalmologic examination at Fundação Leiria de Andrade (FLA), a reference hospital in the state of Ceará and with a specialization service in ophthalmology accredited by the Conselho Brasileiro de Oftalmologia (CBO). This evaluation was first performed by R3 of the FLA specialization course and then repeated by the professor/preceptor of the Ophthalmology/Glaucoma discipline at UNICHISTUS/FLA, without knowing the data obtained by R3, and corresponding ophthalmological examination, in order to avoid biases.
Patients suspected of having glaucoma underwent the following additional eye and vision examinations, taking into account the reliable parameters of each device: ultrasonic pachymetry, color retinography (Digital retinal camera CX-1, Canon, Inc.), computerized campimetry (Humphrey Field Analyzer SITA-FAST 24-2, Carl Zeiss Meditec, Inc.), and optical coherence tomography (Cirrus HD-OCT, software version 3.0, Carl Zeiss Meditec, Inc.) for evaluating the nerve of the peripapillary and macular region. After these complementary eye and vision tests, the patients received a definitive diagnosis, with glaucoma staging based on functional and/or structural changes to classify severity as follows: 1) simplified Hodapp-Parrish-Anderson criterion, using the Humphrey® perimeter, an initial defect would be one in which the mean deviation (MD) parameter is better than or equal to -6.00 dB, a moderate defect when the MD is between -6.01 dB and -12.00 dB, an advanced defect when the MD is between -12.01 dB and -20.00 dB, and a severe defect when the MD is higher than -20.00 dB5; 2) by taking into account structural and functional parameters, being the initial stages (altered OCT with or without change to CC), moderate (altered OCT compatible with the CC injury), or advanced (OCT altered by more than 270° and compatible with the CC injury affecting nealry the entire periphery)7.
Patients who refused to participate in the study or did not sign the Free and Informed Consent Form were excluded from the sample.
The collected data were described by employing the usual descriptive statistics parameters of frequency and average using Microsoft Excel® 2010 software.
RESULTS
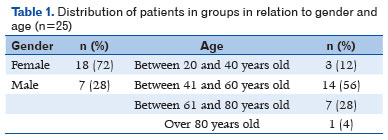
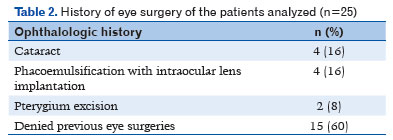
Among the medical records selected during this period, only 25 patients showed up for ophthalmologic appointments. The epidemiological characteristics (gender and age) of these patients are shown in Table 1, while 10 patients reported previous eye surgery (Table 2).
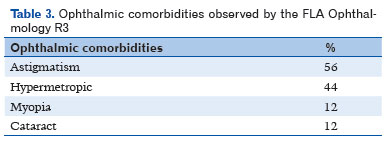
After ophthalmologic examination by R3 students, it was clear that most (92% of patients) had normal corrected visual acuity (CVA) (=1.0), according to the Snellen chart (decimal scale values), whereas the others had CVA <0.5. Regarding ophthalmologic findings, 56% had astigmatism, 44% were hypermetropic, 12% had myopia, and 12% had cataracts.
With regard to IOP, measured by Goldman’s applanation tonometer, the average found in the right eye (OD) was 14.5 mmHg and 13.9 mmHg in the left eye (OS). Gonioscopy was altered only in one patient (increased pigmentation of the camerular sinus by 3+/4+). Fundoscopy showed, as the mean excavation/disc (E/D) ratio, in OD, 0.4 vertical (v) and 0.4 horizontal (h), with the same mean value for the OS.
The R3 students found that 5 patients out of the 25 examined were suspected of having glaucoma, two women and three men, with two patients aged between 41 and 60 years and three between 61 and 80 years. The family history of glaucoma disease was positive in only one patient and four denied previous eye surgery (one patient had undergone phacoemulsification). In these five suspected patients, the R3 students evidenced three patients with altered biomicroscopy, with findings of cataracts, pterygium, and upper eyelid ptosis. Regarding gonioscopy, there was no patient with a closed angle, and the last structure visualized at the angle in both eyes (Oculus Uterque (OU)) was the ciliary band in three patients and up to the scleral spur (SS) in two. Regarding the pigmentation of the camerular sinus, it was evident from gonioscopy that three patients presented 2+/4+, one with 1+/4+, and the other with 3+/4+. Regarding the shape of the iris, three patients presented a convex shape and two presented a flat shape in OU. The mean IOP was 16.6 mmHg in OD (lower value of 12 mmHg and higher value of 22 mmHg) and 15.8 mmHg in OS (lower value of 12 mmHg and higher value of 21 mmHg). Fundoscopy revealed an average E/D of 0.74 × 0.74 in OD and 0.74v × 0.72h in OS.
The same five patients suspected of having glaucoma were re-examined by an experienced glaucomatologist, without knowing the data obtained by R3. The same findings as evidenced by the residents were observed; however, some aspects were different, as shown in Table 4. The IOP found was slightly higher, with an average of 17.4 mmHg in OD (lower value of 15 mmHg and higher value of 20 mmHg) and 18.6 mmHg in OS (lower value of 13 mmHg and higher value of 30 mmHg). After complementary exams with reliable parameters of ultrasonic pachymetry, color retinography, CC, and OCT, glaucoma was found in two patients out of the five suspects, counting three patients with increased excavation/constitutional asymmetry and two with POAG, with three eyes in moderate stage and one eye at an early stage of the disease. All patients were properly medicated and instructed for disease follow-up.
DISCUSSION
Specialization in ophthalmology, regulated by the CBO, requires 3 years of study and work in the area, in centers also regulated by this body, in order to provide physicians with more experience and, consequently, greater knowledge in the field of ophthalmology. At the end of the 3 years, doctors undergo a test for acquiring the title of a specialist in ophthalmology via CBO, giving the opportunity to enter the labor market duly regulated by the Conselho Regional de Medicina (Regional Council of Medicine), with a Registro de Qualificação de Especialista (Specialist Qualification Registry in Ophthalmology). Many of these specialists choose to concentrate on a particular ocular segment, such as sub-specialization in glaucoma (then becoming glaucomatologists), which requires at least one more year of study to obtain greater experience and clinical-surgical refinement in this important pathology8,9.
Glaucoma is an optic neuropathy disease that is the leading cause of irreversible blindness in the world. It includes a group of eye diseases of multifactorial etiology, correlated by a bilateral, asymmetric, and potentially progressive optic neuropathy, which leads to slow loss of the visual field. Because most patients are asymptomatic, when a definitive diagnosis is made, many people have already lost part of their vision. Therefore, a thorough and accurate evaluation is fundamental, in a routine ophthalmologic examination that leads to suspicion of glaucoma, giving the patient the opportunity be diagnosed early and improve the prognosis of the disease.
Based on a detailed anamnesis conducted during the ophthalmic examination, it is possible to identify risk factors that corroborate the diagnosis of glaucoma (age, previous eye diseases, history of eye surgery, family history of glaucoma, history of trauma, use of medications, and systemic pathologies)10. The present study found suspected glaucoma in patients over 40 years of age, most of whom were older than 60 years, corroborating the literature, but differening in family history, because only one of the five patients was associated with the disease (later confirmed as a carrier of POAG)11. This fact underscores the relevance of periodic eye and vision examinations and suspicion of glaucoma in patients over 40 years of age for the prevention, diagnosis, and early treatment of this pathology12.
In the fundoscopy examination, it is possible to perform optic nerve inspection and evaluate the E/D, where a value equal to or lower than 0.3 is present in 70% of normal individuals, while a ratio above 0.6 is present in only 4% of normal individuals13. Only 2% of the population has an E/D ratio greater than 0.7, requiring differentiation between glaucoma or constitutional increase in excavation14. In patients screened by R3 students, the suspicion was raised owing to increased excavations (i.e., above 0.4) because the IOP was not elevated at the time of the examination (higher value of 22 mmHg), a suspicion confirmed by the glaucomatologist (who, however, found an IOP peak of 30 mmHg). This led to them for further investigation with additional tests for this pathology, confirming two cases of POAG and three cases of IE/CA, corresponding to about 8% of the present sample (n=25). Based on an epidemiological study conducted in Brazil in 2007, among individuals over 40 years of age, the incidence of glaucoma was observed to be 3.4%15, but our highest rate corroborates the selection bias for a small sample size.
Gonioscopy is the most relevant examination for the classification of glaucoma disease. Based on this evaluation, it is possible to visualize the amplitude of the iridocorneal angle, and this angle is found to cause an increase in IOP when it is closed or has a small amplitude, which results in PCAG, with low frequency in our population16, and not evidenced in the patients evaluated in the present study. In case of patients with POAG, gonioscopy is used to exclude other causes of increased IOP, such as inflammatory precipitates, increased pigmentation, angular recess, synechiae, and new vessels,17. In the present study, the R3 students presented increased pigmentation in two patients, which was different from the result of the examination conducted by the glaucomatologist, showing physiological pigmentation in these same patients. This difference in results between examiners is frequent because this test requires a longer learning curve, requiring more years of experience for greater security in detailing the camerular sinus. According to a published study, it was proven that students recently graduated from the ophthalmology residency presented great difficulty in diagnosing cases of greater complexity of glaucoma because they did not have contact with more complex glaucoma cases in comparison with glaucomatologists18.
This difference also occurs with respect to E/D, wherein there was a difference in the measurement conducted by residents and the glaucomatologist in three patients (out of the five evaluated), with a higher value being found by the glaucomatologist for two patients and for one patient with lower value for one eye (perhaps this asymmetry generated insecurity on the part of the resident in better defining the excavation). These different results between the findings of R3 students and the glaucomatologist were also evidenced in other studies, with a comparative evaluation between teachers and residents, including post-surgical care and practices, with teachers presenting lower rates of error. At the end of this study, further comparison studies were suggested to be conducted to identify ways to improve the performance of future specialists so that they are better prepared for practice and care19. In another cross-sectional study, in which a comparison was made between two groups of residents from the first and third year and a specialist in glaucoma disease, with an agreement that varied from poor to moderate, the results of R3 students were closer to the findings of the glaucomatologist20. Both studies showed that more were the number of years of study in the field of glaucoma, the greater was the accuracy of the clinical findings, which consequently reinforced the results found in the present study.
With regard to IOP, ocular hypertension was detected in only two patients. Although high IOP is considered the main risk factor, it is not sufficient to make a definitive diagnosis of glaucoma, making it necessary to perform more tests such as CC and OCT, because the IOP measured at the time of medical appointment may not be the peak value or the patient may have normal tension glaucoma (although not very prevalent, it affects the age group of the present study)21.
According to Joshi et al., in 2019, of 200 patients examined by general and resident ophthalmologists, 85% were referred to as suspected glaucoma based on optic nerve examination. Of these, after being examined by a glaucomatologist, only 14.5% had the diagnosis confirmed. Therefore, this study also emphasizes the importance that more training is required for general and resident ophthalmologists for the correct diagnosis of glaucoma22.
The R3 students presented satisfactory performance in screening suspects for glaucoma disease, of which two had a confirmed diagnosis of glaucoma and three were suspected of having increased constitutional excavation.
Although the values were not absolutely equal in relation to the evaluation of the glaucomatologist, it is observed that the difference found did not interfere with the number of cases diagnosed, giving clues to the outstanding quality of education in this institution accredited by the CBO. However, the sample was insufficient to show statistical relevance regarding the quality of specialization services in ophthalmology in the context of the study.
REFERENCES
1. Demarco AL, Rodrigues M de L, Demarco LA. Perfil oftalmológico de pacientes ingressantes no setor de glaucoma de um serviço universitário. Medicina, Ribeirão Preto. 2002;35(4):478-86.
2. Ministério da Saúde. Protocolo Clínico e Diretrizes Terapêuticas Glaucoma. Brasília: Ministério da Saúde; 2018.
3. Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262-7.
4. Wu SY, Nemesure B, Hennis A, Schachat P, Hyman Leslie, Leske Cristina. Open-angle glaucoma and mortality: The Barbados Eye Studies. Arch Ophthalmol. 2008;126(3):365-70.
5. Conselho Internacional de Oftalmologia. Diretrizes para Tratamento Ocular do Glaucoma. 1 ed. São Francisco: Conselho Brasileiro de Oftalmologia (CBO); 2016.
6. Fingeret M, Medeiros FA, Susanna R Jr, Weinreb RN. Five rules to evaluate the optic disc and retinal nerve fiber layer for glaucoma. Optometry. 2005;76(11):661-8.
7. Gupta N, Aung T, Congdon N, Dada T, Lerner F, Olawaye S et al. Diretrizes do ICO para tratamento do glaucoma. Conselho Internacional de Oftalmologia. 2015:1-27.
8. Hospital de olhos [https://hospitaldeolhos.net/]. Conheça as especialidades da oftalmologia [acesso em 21 mar 2020]. Disponível em: https://hospitaldeolhos.net/dicas/especialidades-da-oftalmologia/
9. Ministério da Educação [http://portal.mec.gov.br/]. Residência médica [Acesso em 21 mar 2020]. Disponível em: http://portal.mec.gov.br/residencias-em-saude/residencia-medica.
10. Ottaiano JAA, Ávila MP, Umbelino CC, Taleb AC. As condições de saúde ocular no Brasil. 1ed. São Paulo: Conselho Brasileiro de Oftalmologia (CBO). 2019.
11. American Academy of Ophthalmology. Primary Open-Angle Glaucoma. Preferred Practice Pattern. São Francisco: Elsevier; 2015.
12. 12. Gonçalves MR, Guedes MMR, Chaves MAPD, Pereira CCL, Otton R. Análise dos fatores de risco e epidemiologia em campanha de prevenção da cegueira pelo glaucoma em João Pessoa, Paraíba. Rev Bras Oftalmol. 2013;72(6):396-9.
13. Mello PAA, Júnior RS, Almeida HG. Série Oftalmologia Brasileira. 3 ed. Rio de Janeiro. Cultura Médica. 2014.
14. Kanski JJ, Bowling B. Oftalmologia clínica. 8° ed. Rio de Janeiro: Elsevier; 2016.
15. Sakata K, Sakata LM, Sakata VM, Santini C, Hopker LM, Bernardes R, et al. Prevalence of glaucoma in a South brazilian population: Projeto Glaucoma. Invest Ophthalmol Vis Sci. 2007; 48(11):4974-9.
16. Sociedade Brasileira de Glaucoma. II Consenso de Glaucoma Primário de Ângulo Fechado. São Paulo: Novartis; 2012.
17. Ribeiro, JCML, Alves, APX, Ferreira JLM, Neto LA. Oftalmologia para a graduação. 1ed. Fortaleza: EdUnichristus; 2019.
18. Millán T. Percepções de médicos oftalmologistas de como os programas de residência médica do estado de São Paulo os preparam para a prática profissional. Programa de residência médica do estado de São Paulo. São Paulo: Unicamp; 2012.
19. Zebardast N, Solus JF, Quigley HA, Srikumaran D, Ramulu PY. Comparison of resident and glaucoma faculty practice patterns in the care of open-angle glaucoma. BMC Ophthalmology. 2015 Apr 14;15:41.
20. Rossetto JD, Melo Jr LAS, Campos MS, Tavares IM. Agreement on the evaluation of glaucomatous optic nerve head findings by ophthalmology residents and a glaucoma specialist. Clin Ophthalmol. 2017 Jul 10;11:1281-4.
21. Tavares IM, Mello PAA. Glaucoma de pressão normal. Arq Bras Oftalmol. 2005;68(4):565-75.
22. Joshi PL, Jha B, Paudyal I, Thapa SS. Referral parameters for diagnosis of glaucoma in general eye clinic at Tilganga Institute of Ophthalmology. Nepal J Ophthalmol. 2019;11(21):33-9.
AUTHOR’S INFORMATION
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
August 27, 2020.
Accepted on:
August 25, 2021.