Marcelo Bezerra Diógenes1; Ana Carolina P. de Freitas1; Nayara Queiroz Cardoso Pinto2; Islane Maria Castro Verçosa3; Dácio Carvalho Costa3
DOI: 10.17545/eOftalmo/2020.0009
ABSTRACT
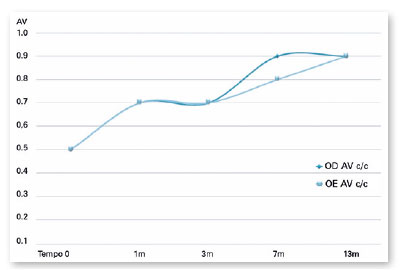
Herein, we have described the benefits of using a 0.55% cysteamine ophthalmic solution in a nine-year-old patient with ocular cystinosis. Cystinosis is a rare autosomal recessive disease that affects on average 1 in 200,000 people. It is characterized by the deposition of cystine in various tissues, including the eyes. Treatment should be performed with one drop of a 0.55% cysteamine ophthalmic solution every 2 hours, but high cost and difficult access hinder the use of this medication. The patient described in this report presented significant improvement in visual acuity and photophobia in a 13-month period of follow-up and irregular treatment with a 0.55% cysteamine ophthalmic solution. At the beginning of treatment, the patient presented a visual acuity of 0.5 in both eyes, and at the end of treatment, it reached 0.9 in both eyes. Photophobia was initially described as grade 2 (photophobia to the thinnest beam of the slit lamp) and as grade 0 (no photophobia to the slit lamp) after 3 years of irregular treatment. This study presents the benefits of irregular use of this topical medication for visual acuity and photophobia in a patient with ocular cystinosis.
Keywords: Cystinosis; Cysteamine; Cornea, Photophobia.
RESUMO
Descrever os benefícios da solução oftalmológica de cisteamina 0.55% em uma paciente de nove anos com cistinose ocular. Cistinose é uma doença autossômica recessiva rara que atinge em média 1 a cada 200.000 pessoas. Ela é caracterizada pelo depósito de cistina em vários tecidos, entre eles o olho. O tratamento deve ser feito com solução oftalmológica de cisteamina 0,55% uma gota a cada duas horas, porém o alto custo e o difícil acesso dificultam o uso contínuo dessa medicação. A paciente descrita nesse relato apresentou melhora significativa de acuidade visual e fotofobia em um período de 13 meses de acompanhamento e tratamento irregular com solução oftalmológica de cisteamina 0,55%. No início do tratamento a paciente apresentava acidade visual de 0,5 em ambos os olhos e ao final a acuidade visual chegou a 0,9 em ambos os olhos. A fotofobia foi descrita inicialmente como grau 2 (fotofobia ao feixe mais fino da lâmpada de fenda) e após 3 anos de tratamento irregular como grau 0 (sem fotofobia à lâmpada de fenda). Esse estudo descreve benefícios do uso irregular dessa medicação tópica na acuidade visual e fotofobia de uma paciente com Cistinose ocular.
Palavras-chave: Cistinose; Cisteamina; Córnea, Fotofobia.
INTRODUCTION
Cystinosis is a rare autosomal recessive disorder with an incidence ranging from 1:100,000 to 1:200.0001,2. A mutation of the 17p chromosome has been associated with a primary defect in active cystine transportation through the lysosomal membrane. This transportation defect leads to the deposition of cystine crystals in lysosomes1. Affected tissues include the thyroid, testicles, pancreas, muscles, brain, and eyes1,3.
Three phenotypic forms of cystinosis are described: infantile nephropathic cystinosis, intermediate cystinosis, and nonnephropathic cystinosis. This article focuses on the infantile form, which is the most related to ocular changes1,4,5.
The ocular symptoms of cystinosis result from the deposit of cystine crystals, mainly in the cornea and conjunctiva6. Corneal deposits occur in the peripheral cornea and anterior stroma; as the disorder progresses, crystals start depositing centripetally and posteriorly, involving the whole stroma around the age of 7 years4,7. Deposits may also affect the corneal epithelium, which may be related to the foreign body sensation reported by some patients8. Without treatment, deposits become increasingly dense, causing photophobia and progressively affecting visual acuity5.
Other factors may be related to visual acuity impairment in cystinosis: retinitis pigmentosa, macular crystal deposit, posterior synechia, glaucoma, and hemorrhagic retinopathy3,5. The increased life expectancy of patients with infantile cystinosis has led to increased frequency of these rare changes2.
To minimize eye complications related to the progression of this systemic disorder, regular and multidisciplinary follow-up is required9. Treatment should be performed with oral and topical cysteamine. A 0.55% cysteamine ophthalmic solution used continuously every 2 hours has shown good results and should be prescribed in all cases of cystinosis with ocular involvement6. In this report, we describe the impact of topical treatment on ocular symptoms of a ten-year-old patient.
CASE DESCRIPTION
A ten-year-old female patient from Ceará, Brazil, with a short stature for her age, was diagnosed with infantile cystinosis at the age of 7 years. She was started Cystagon 200 mg four times per day. At the age of 9 years, the patient underwent single kidney transplantation for cystinosis-related chronic kidney disease. She presented with a complaint of photophobia.
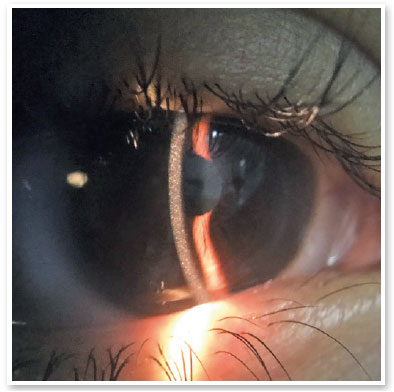
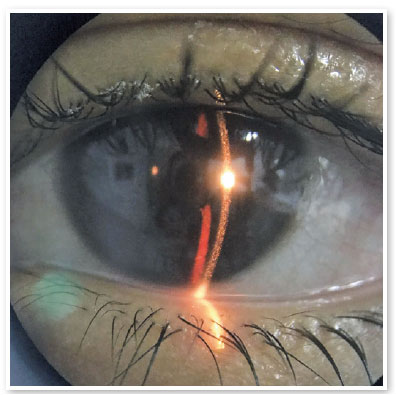
Initial eye examination, at the age of 10 years, showed a 0.5 corrected visual acuity (CVA) in both eyes (OU). Refractometric examination showed emmetropia in OU. On biomicroscopic examination, the patient presented photophobia to the thinnest light beam and showed diffusely distributed crystal deposits in the corneal stroma. No changes were observed in the eyelids, conjunctiva, iris, lens, corneal epithelium, or endothelium in OU. Fundoscopic examination was normal in OU.
Six months later, the patient started irregular use of 0.55% cysteamine eye drops, one drop every 2 hours in both eyes, with progressive improvement of visual acuity. After a month using this medication, she presented a 0.7 CVA in OU. With 3 months of use, VA remained the same, and with 7 months there was a new improvement: 0.9 CVA OD and 0.8 OS. Finally, after approximately 13 months of use, the patient presented a 0.9 CVA OU (Figure 1), without photophobia and with the presence of crystals in the stromata of both eyes on slit lamp examination (Figures 2 and 3).
DISCUSSION
The effectiveness of the topical treatment of cystinosis is already well-described in the literature4,5. Without treatment, cystine deposits can lead to blindness due to corneal opacity, glaucoma, or changes in the retina3,5.
Treatment with topical cysteamine has been recently recognized in Brazil and can be acquired by judicial means, as in the case of the patient described. Unfortunately, the 0.55% cysteamine ophthalmic solution is a high-cost drug, each 3.8ml bottle costing around 4,500 Brazilian reais, which makes it difficult to use the medication every 2 hours, in accordance with the literature5.
In the case reported, the patient used the 0.55% cysteamine ophthalmic solution for approximately 4 months within a period of 13 months. Although she did not use the topical drug for most of the year, the patient presented significant improvement in visual acuity and photophobia. We had initially identified photophobia grade 2 (photophobia to the thinnest beam of the slit lamp), and after 13 months of irregular use of cysteamine, we identified photophobia grade 0 (without photophobia on examination with slit lamp)6.
This study highlights the importance of topical treatment for ocular cystinosis, which in this case not only prevented progression but also improved photophobia and visual acuity. Considering how rare the disorder is and how difficult it is to obtain cysteamine eye drops, we encourage the reporting and publication of cases describing the use of topical cysteamine 0.55% and the results of treatment in an attempt to identify new dosages compatible with the reality of developing countries and communities in social vulnerability.
REFERENCES
1. Gahl, WA, Thoene JG, Schneider JA. Cystinosis. N Engl J Med. 2002;347(2):111-21.
2. Victor G, Campos PJG, Alves MR, Nosé W. Microscopia confocal in vivo na cistinose: relato de caso. Arq Bras Oftalmol. 2004; 67(3):553-7.
3. Tsilou E, Zhou M, Gahl W, Sieving PC, Chan C-C. Ophthalmic manifestations and histopathology of infantile nephropathic cystinosis: report of a case and review of the literature. Surv Ophthalmol. 2007;52(1):97-105.
4. Gahl WA, Kuehl EM, Iwata F, Lindblad A, Kaiser-Kupfer MI. Corneal crystals in nephropathic cystinosis: natural history and treatment with cysteamine eyedrops. Mol Genet Metab. 2000; 71(1-2):100-20.
5. Al-Hemidan A, Shoughy SS, Kozak I, Tabbara KF. Efficacy of topical cysteamine in nephropathic cystinosis. Br J Ophthalmol. 2017;101(9):1234-7.
6. Liang H, Baudouin C, Hassani RTJ, Brignole-Baudouin F, Labbe A. Photophobia and corneal crystal density in nephropathic cystinosis: an in vivo confocal microscopy and anterior-segment optical coherence tomography study. Invest Ophthalmol Vis Sci. 2015;56(5):3218-25.
7. Flockerzi E, Daas L, Schötzer-Schrehardt U, Zimpfer A, Bohle R, Seitz B. Ocular changes in nephropathic cystinosis: The course of the gold-dust. Int Ophthalmol. 2019;39(6):1413-8.
8. Alsuhaibani AH, Khan AO, Wagoner MD. Confocal microscopy of the cornea in nephropathic cystinosis. Br J Ophthalmol. 2005;89(11):1530-1.
9. Pinxten A-M, Hua M-T, Simpson J, Hohenfellner K, Levtchenko E, Casteels I. Clinical practice: a proposed standardized ophthalmological assessment for patients with cystinosis. Ophthalmol Ther. 2017;6(1):93-104.
AUTHOR'S INFORMATION




Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
January 24, 2020.
Accepted on:
June 24, 2020.