Paula Paiva Pegoraro, Graziela Boschetti, Letícia Sato Fernandes Alli Ahmad, Dinorah Piacentini Engel Castro
DOI: 10.17545/eOftalmo/2020.0008
ABSTRACT
Differentiating glaucomatous from nonglaucomatous optic neuropathy may be complex for the ophthalmologist, since both can have a similar clinical picture. Thus, neurological lesions become essential as differential diagnoses for glaucoma. Not only the diagnosis but also the follow-up and treatment of patients with neurological lesions associated with glaucoma are considered challenges. Therefore, a comprehensive and detailed investigation of the changes suggestive of each etiology, as well as complementary examinations to better elucidate the case are necessary. This report aims to highlight the importance of these differential diagnoses.
Keywords: Ophthalmology; Glaucoma; Neuro-ophthalmology; Meningioma.
RESUMO
A diferenciação entre neuropatia óptica glaucomatosa de não glaucomatosa pode ser complexa para o médico oftalmologista, uma vez que ambas podem cursar com quadro clínico semelhante. Dessa forma, as lesões neurológicas se tornam essenciais como diagnósticos diferenciais de glaucoma. Não só o diagnóstico, mas também o seguimento e tratamento de pacientes com lesões neurológicas associadas ao glaucoma são considerados desafios. Portanto, é necessária uma investigação abrangente e detalhada a respeito das alterações sugestivas de cada etiologia, além de exames complementares para melhor elucidação do caso. O presente relato tem por objetivo alertar a importância de tais diagnósticos diferenciais.
Palavras-chave: Oftalmologia; Glaucoma; Neuoroftalmologia; Meningioma
INTRODUCTION
Meningioma is a primary neoplasm of the central nervous system, corresponding to 14%-20% of intracranial tumors and 25%-32% of spinal tumors. It is the second most common type of primary brain tumor. The incidence is 6 cases per 100,000 per year1 and the prevalence is 97.5 cases per 100,0002. The World Health Organization classifies meningeomas into four groups: classical, atypical, papillary, and anaplastic or malignant3. Most tumors have a benign presentation4. The tumor’s location may vary but is predominantly in the cerebrum, adhering to the dura mater. The location and extent of the tumor determine the clinical picture5. Therefore, computerized axial tomography (which enables diagnosis in 63% of cases without contrast and 90% of cases with the use of contrast)5,6 associated with magnetic resonance imaging (in which meningiomas are isointense relative to the brain in T1 and T2)5,7 are essential for diagnosis. Vision changes are common when tumor involves optical pathways, e.g., visual field defects, optic atrophy, visual loss and papilledema. These changes make the disease an important differential diagnosis for glaucoma8. Meningeoma is predominant in females, from 50 to 70 years old, usually grows slowly, and can reach large proportions before manifesting any sign or symptom9,10.
Glaucoma is a slowly progressive optic neuropathy that causes characteristic changes to the visual field. It is the leading cause of irreversible blindness worldwide. The main risk factor is intraocular pressure (IOP). Another risk factors are increased age, family history, ethnicity, corneal pachymetry, low ocular perfusion pressure, type 2 diabetes mellitus and refractive errors11.
This report aims to pay attention to differential diagnoses for glaucoma. Alterations of the optic disc and visual field changes are indicators of glaucoma, however may have other etiologies. The case was initially diagnosed as glaucoma, and, subsequently, due to visual field changes, a meningeoma was found.
CASE REPORT
Patient E.D.V.C., female, 72 years old, came to a routine medical visit presenting low visual acuity for one year. She reported no systemic comorbidities, no previous history of ophthalmic conditions and no family history of glaucoma.
She presented 1.0 corrected visual acuity in both eyes (OU) and IOP of 16mmHg in the right eye (OR) and 20mmHg in left eye (OS), with Goldmann tonometry. Biomicroscopy showed no relevant changes in OU. Fundoscopy (Figure 1) showed thinning of the neural rim with nasal remnants, with an inferior nasal defect of peripapilar nerve fiber layer (HOYT), and superior disc hemorrhage in OR; OS showed pale optic disc with total excavation and diffuse nerve fiber layer defect. Gonioscopy showed the posterior trabecular meshwork in superior and inferior quadrants and anterior trabecular meshwork in the nasal and temporal quadrants in OR. Posterior trabecular meshwork was observed in nasal quadrant and anterior trabecular meshwork was observed in other quadrants in OS. Cornea thickness was 495μm in OR and 531μm in OS.
Diagnostic hypothesis was glaucoma with an occluded angle in OU and laser iridotomy was performed. Gonioscopy pos iridotomy showed open angle and posterior trabecular meshwork visualization in the four quadrants of OU.
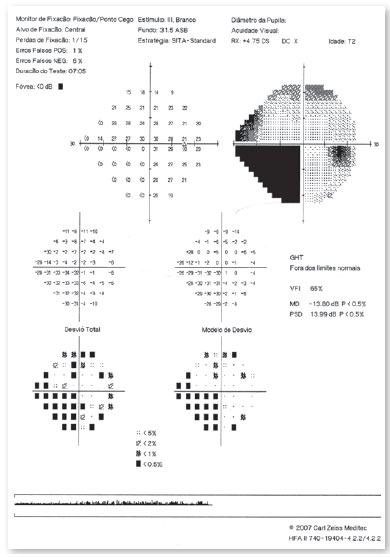
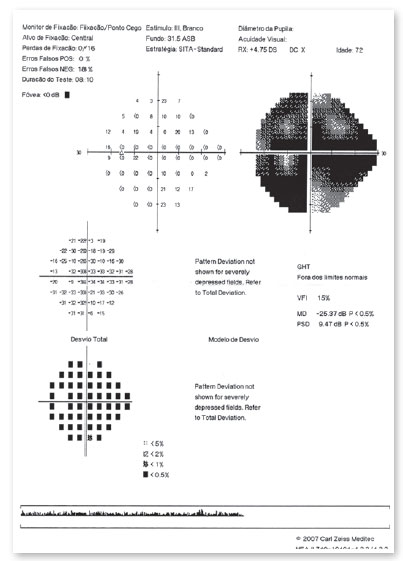
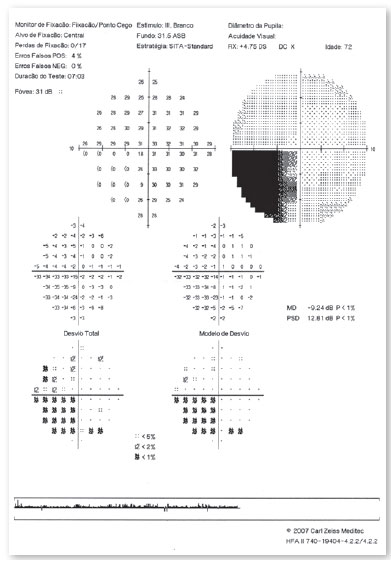
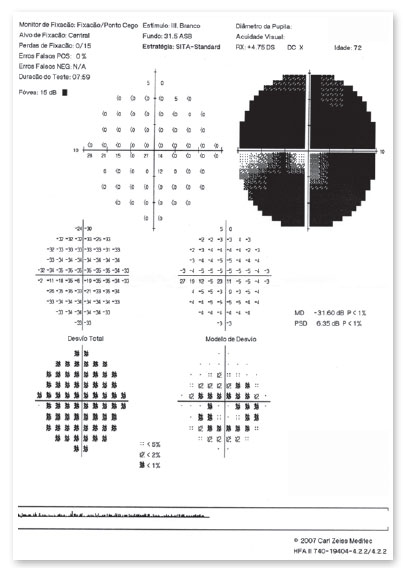
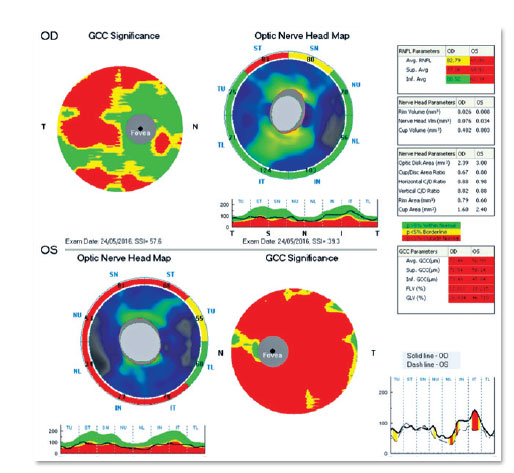
Computerized visual field (VF) (Figure 2, 3) showed an inferior nasal defect in OR and generalized depression in OS. Central visual field (Figure 4, 5) suggested inferior nasal quadrantanopsia in OR.
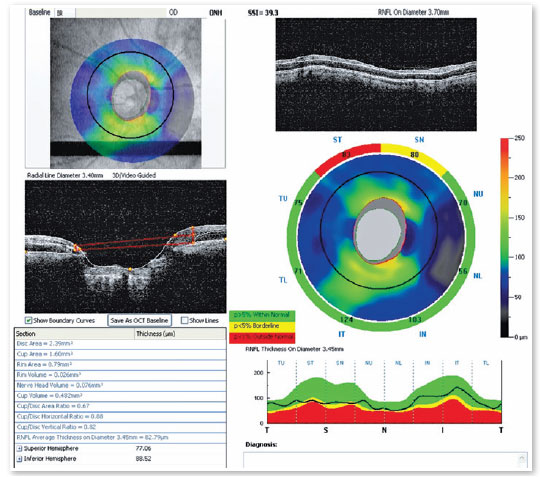
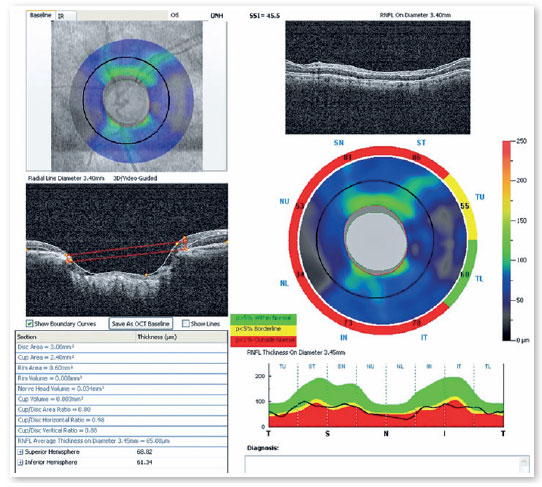
Optical coherence tomography (Figure 6, 7) showed superior temporal thinning of peripapilary nerve fiber layer in OR and diffuse thinning in OS, except for the lateral temporal region. The macular ganglion cell layer report (Figure 8) showed perifoveal thinning in OU.
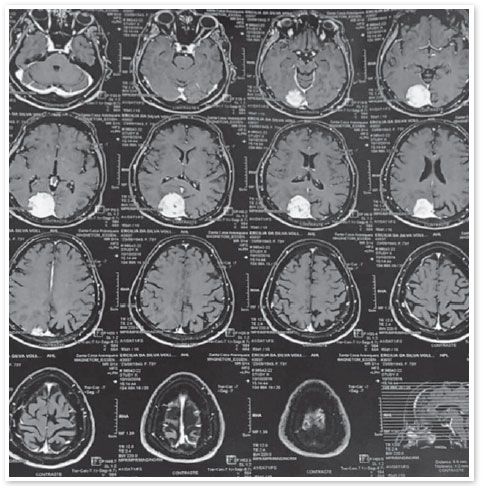
The hypothesis of glaucoma with an occluded angle in OU was maintained; however, the differential diagnosis of a possible neurological condition was added. Therefore, magnetic resonance imaging of the skull was requested (Figure 9) a right occipital meningioma was found.
DISCUSSION
Differentiating glaucomatous from nonglaucomatous optic neuropathy based on optic disc changes can be challenging. Therefore, detailed medical hystory and complete clinical examination are essential for an accurate diagnosis8.
Glaucoma is the most frequent cause of increased acquired excavation12-14. Other etiologies as ischemia, toxicity, compressive lesions such as meningioma and genetic disorders can cause similar changes8.
Some findings may assist the physician in the differential diagnosis. Loss of visual acuity and color vision may occur in advanced glaucoma, but usually take place earlier in nonglaucomatous optic neuropathies8,12. In this case, the patient had good visual acuity and no color vision alteration. Some optic neuropathies tend to be more symmetrical and do not present afferent pupillary defect, such as glaucoma, papilledema, nutritional deficiency, toxicity, and genetic disorders8. The reported case did not show afferent papillary defect, suggesting glaucoma.
More vertical cup-to-disc ratio (CDR), hemorrhages, atypical change in disc vessels, and usual coloration of papillary rim suggest glaucomatous neuropathy12-14. The patient presented disc hemorrhage and opt disc changes suggestive of glaucomatous optic neuropathy.
Some signs are common to both glaucomatous and nonglaucomatous optic neuropathy, e.g.: IOP, cribriform plate exposure and partial neuroretinal rim thinning8,12-14. In this case, IOP was not very high but the corneal pachymetry showed thin value.
Vision acuity reduction (0,5), rim pallor, age <50 years, VF respecting the vertical midline, VF defects not consistent with CDR and vascular changes in retina are findings suggestive of nonglaucomatous optic neuropathy8.
VF changes, due to glaucoma, usually follow four main patterns: isolated scotoma, arcuate scotoma, nasal step and generalized depression. VF findings in nonglaucomatous optic neuropathy, on the other hand, are often more central, respecting the vertical meridian most of the time8,12-14. The VF changes in the reported case were essential for central alterations suspicious, enabling meningeoma diagnosis.
The avaluation of a patient with optic changes should consider neuro-ophthalmological disorders, especially in the presence of the following findings: loss of color vision disproportionate to the reduction in VA, VF defects not correlated with optic disc changes, VF defects in vertical alignment, relative afferent pupillary defect and pale residual optic disc rim8.
This report showed a patient with bilateral optic disc changes and VF defects which raised nonglaucomatous optic neuropathy hypothesis. Imaging exam could elucidated the diagnosis.
VF testing is important not only to monitor glaucoma but also to diagnose neurologic lesions. Monitoring and treatment patients with neurologic lesions associated with glaucoma are challengig, since optic disc damage may have associated etiologies.
REFERENCES
1. Chou SM, Miles JM. The pathology of meningiomas. In: Mefty O. Meningiomas. New York: Raven Press. 1999, p.37-57
2. Claus EB, Bondy ML, Schildkraut JM, Wiemels JL, Wrensch M, Black PM. Epidemiology of intracranial meningiomas. Neurosurgery. 2005;57:1088-9.
3. Louis DN, Ohgaki H, Wiestler OD, et al. A Classificação da OMS de 2007 de Tumores do Sistema Nervoso Central. Acta Neuropathol 114, 97-109 (2007) doi: 10.1007 / s00401-007-0243-4
4. Jaaskelainen J, Haltia M, Servo A. Atypical and anaplastic meningiomas: radiology, surgery, radiotherapy and outcome. Surg Neurol. 1986;25:233-242.
5. Torres, LFB et al. Meningiomas: estudo epidemiologic e anátomopatológico de 304 casos. Arquivos de Neuro-Psiquiatria. 54(4), 549-556.
6. Dietemann, J.L., Heldt, N., Burguet, J.L. et al. CT findings in malignant meningiomas. Neuroradiology. 23, 207-209 (1982) doi:10.1007/BF00342542
7. Zee CS, Chen T, Hinton DR, Tan M, Segall HD, Apuzzo MLJ. Magnetic resonance imaging of cystic meningiomas and its surgical implications. Neurosurgery. 1995;36:482-488.
8. Fraser CL, White AJ, Plant GT, Martin KR. Optic Nerve Cupping and the Neuro-Ophthalmologist. Journal of Neuro-Ophthalmology. Dez 2013, Vol 33.
9. Hanft S, Canoll P, Bruce JN. A review of malignant meningiomas: diagnosis, characteristics, andtreatment. J Neurooncol. 2010; 99:433.
10. Olivero WC, Lister R, Elwood PW. The natural history and growth rate of asymptomatic meningiomas: a review of 60 patients. J Neurosurg. 1995;83:222-224.
11. Lauretti CR, Lauretti FA. The glaucomas. Medicina, Ribeirão Preto, 30: 56-65, jan./marco 1997.
12. Allingham RR. Shields Tratado de Glaucoma- 6ª edição, Lippincott Williams & WilkinUSA, 2005, Ed.Cultura Médica, Rio de Janeiro, 2014.
13. Coleção CBO: Série Oftalmológica Brasileira. 3. ed. Rio de Janeiro: Guanabara koogan 2013.
14. Kanski JJ, Bowling B. Oftalmologia clínica: uma abordagem sistemática. 8a ed. Rio de Janeiro: Elsevier; 2016.
AUTHOR’S INFORMATION


Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
December 10, 2019.
Accepted on:
June 17, 2020.