Adriana Geremias Toni1,2 ; Nathalia Perussi Garcia1,2; Bruno De Amicis Zanchetta1,2; Priscilla Fernandes Nogueira1,2; Guilherme Novoa Colombo Barboza1,2; Marcello Novoa Colombo Barboza1,2
DOI: 10.17545/eOftalmo/2020.0007
ABSTRACT
Occlusion of the central retinal artery (CRA) is a cause of irreversible blindness. The visual prognosis is poor and is considered an ophthalmological emergency. The objective of this study is to document the importance of thrombophilia as a risk factor for CRA occlusion and to emphasize that ophthalmologists should investigate thrombophilia, which also makes it possible to prevent thrombosis in other organs. The patient in this case was followed before and after an episode of sudden visual loss with clinical and complementary examination, evidencing the difficulty of previous diagnosis.
Keywords: Retina; Retinal artery; Retinal vasculitis; Fluorescein angiography; Thrombophilia
RESUMO
A oclusão da artéria central da retina (ACR) é uma causa de cegueira irreversível. O prognóstico visual é pobre e é considerada uma emergência oftalmológica. O objetivo do estudo é documentar a importância da trombofillia como um fator de risco para oclusão da ACR e enfatizar que os oftalmologistas devem investigar trombofilia, o que torna possível a prevenção de trombose em outros órgãos. A paciente do caso foi acompanhada antes e após o episódio de perda visual súbita com exame clínico e complementar, evidenciando a dificuldade de diagnóstico prévio.
Palavras-chave: Retina; Artéria retiniana; Vasculite retiniana; Angiofluoresceinografia; Trombofilia
INTRODUCTION
Central retinal artery (CRA) occlusion is a cause of irreversible blindness that mainly affects female individuals after 60 years of age, with an incidence of 1 per 10,000 inhabitants.1,2 The retina is nourished by the vessels of the choroid and the branches of the CRA. On an average, 15%-30% individuals have a cilioretinal artery that flows in the direction of the macular region.3
Its clinical picture is characterized by sudden and painless unilateral loss of visual acuity, which may follow transient episodes of visual loss. Clinical ophthalmological examination evidences retinal pallor and opacity, and a reddish coloration in the foveal region owing to the persistence of circulation through the choroid.2
In case of suspected CRA occlusion, a complete ophthalmological examination should be performed, along with assessment of the visual acuity, intraocular pressure (IOP), eye reflexes, biomicroscopy, and fundoscopy. Diagnosis is often clinical and no complementary examinations are required.
The visual prognosis depends on the immediate therapeutic measures taken, but it is still poor. Most patients develop permanent poor vision, but they may have a better prognosis if the cilioretinal artery is patent.4 CRA occlusion is considered an ophthalmological emergency, with a discouraging prognosis.
This study aimed to document the importance of thrombophilia as a risk factor for CRA occlusion, particularly in young patients and those without other risk factors, which also makes it possible to prevent thrombosis in other organs. The ophthalmologist plays a critical role in the investigation and prognosis of these patients, particularly when this is the first thrombotic event. The patient in this case was followed before and after an episode of sudden visual loss with clinical and complementary examination, evidencing the difficulty of previous diagnosis.
CASE REPORT
The patient was a 55-year-old female of mixed African and Caucasian ethnicity, a post-office cashier. Personal background: arterial hypertension, two previous cesarean sections, and a smoker (45 packs/year). She reported no significant eye and family diseases. Complaint and duration: amaurosis fugax in both eyes (AO) 2 months ago. The patient reported the condition to be sporadic, with spontaneous improvement within a few minutes. She denied fever, trauma, or use any medication other than losartan.
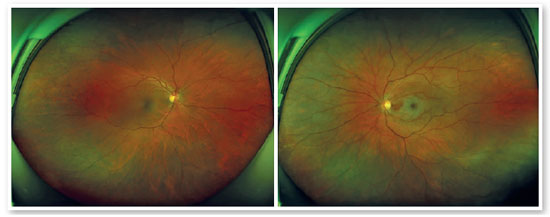
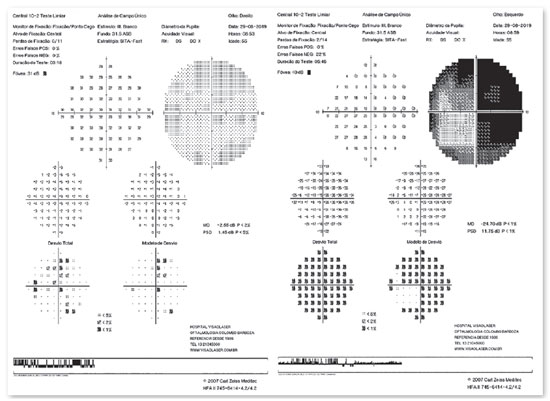
On ophthalmological examination, she had best corrected visual acuity (BCVA) of 20/25 OU; IOP measured by the applanation method was 14 and 12mmHg. Biomicroscopy showed no changes in OU. Eye reflexes showed preserved OU. Retinal mapping indicated physiological excavation, well delimited and rosy papillae, free macula, preserved vascular arches, retina applied to the posterior pole (Figure 1).
The patient was oriented to seek cardiological, vascular, and hematological evaluation, to stop smoking, and to make lifestyle changes. She should return quarterly or earlier if new symptoms or alarming signs appeared.
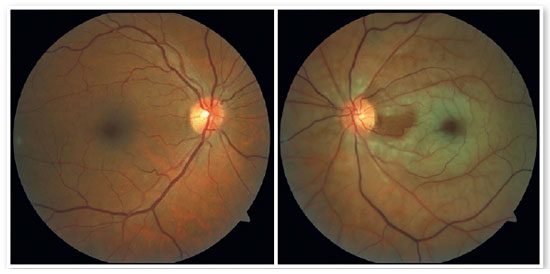
After 2 months, she returned with complaint of sudden low visual acuity (LVA) in the left eye (OS) that persisted for 6 hours. She reported normal vision on the previous day; however, when she woke up, she noticed LVA in OS, with a small region of inferior temporal vision. Ophthalmological examination: BCVA: 20/25 and hand movement, IOP: 14 and 16mmHg. Confrontation field: impaired in OS. Eye reflexes: preserved in OD, OS: decreased consensual reflex 2+, decreased direct reflex 1+, with a relative afferent pupillary defect. Pupils: anisocoric, moderate mydriasis in OS. Retinal mapping: OD: no changes. OS: physiological excavation, rosy papilla, and retinal pallor in the perimacular region.
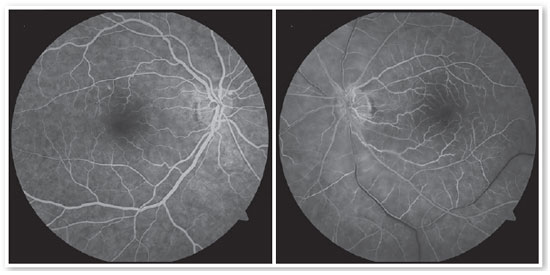
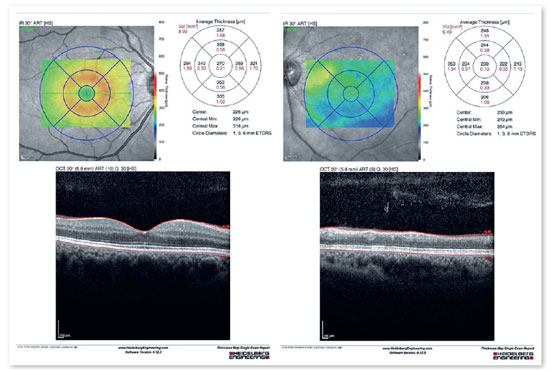
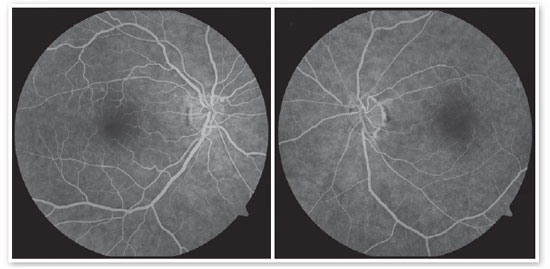
Retinography and Optomap showed perimacular pallor (Figures 2 and 3), visual field with a tubular scotoma in OS (Figure 4), macula OCT with edema of the superficial layers (Figure 5), and fluorescein angiography with delayed filling and slight hyperfluorescence in the peripapillary and inferior nasal regions (Figure 6). Based on the examinations, CRA occlusion was diagnosed with a patent cilioretinal artery.
Mannitol 20% IV and eye massage were applied at the time of the consultation, and topical timolol 0.5% was prescribed, with no therapeutic success.
She was referred for cardiological, vascular, and hematological evaluation and oriented to stop smoking and make lifestyle changes, with a strict control of arterial pressure.
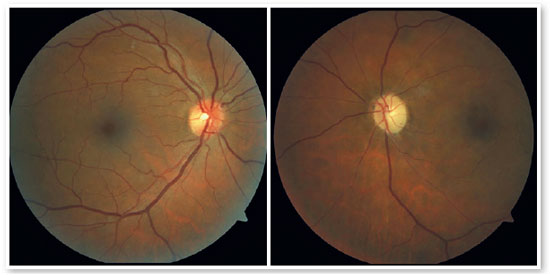
She returned after 2 months reporting a persistence of LVA in OS, with no further complaints. New examinations were performed (Figures 7-10). Blood profile was evaluated, and she was diagnosed with thrombophilia, with the presence of a G20210A mutation in the prothrombin gene (GPT) in heterozygosis and absence of factor V Leiden (FVL) mutation. The coagulation factors VII and VIII, proteins C and S, anticardiolipin antibodies, antithrombin III activity, and serum homocysteine dosage were all within reference values. The patient is undergoing follow-up with a hematologist, cardiologist, and ophthalmologist every 6 month
DISCUSSION
The case presented was followed before and after the occurrence of sudden visual loss. The patient underwent complete ophthalmological evaluation, and complementary examinations were performed due to a complaint of amaurosis fugax, but with no evidence of any changes.
CRA blockade is sudden and evolves with retinal hypoperfusion and rapidly progressive cell damage. The survival of the retina depends on the degree of collateralization and the duration of retinal ischemia. It is believed that permanent damage occurs in just >90 min.4.5 Patients with the cilioretinal artery have a better prognosis in the long term; however, our patient evolved with hand-movement visual acuity, which is possibly related to the duration and degree of ischemia.1-3
CRA occlusion can be classified into four clinical entities: non-arteritic, non-arteritic with a cilioretinal artery, arteritic associated with giant-cell arteritis, and transient non-arteritic. Arteritic CRA occlusion occurs in <5% of patients and is most commonly related to giant-cell arteritis. Although infrequent, such cases should be suspected and referenced as soon as possible, owing to their high potential for visual loss or irreversible neurological damage.6
One of the differential diagnoses of giant-cell arteritis is Susac Syndrome. Although rare, this syndrome exhibits a progressive neurological dysfunction associated with psychosis, hypoacusis, and occlusions of multiple branches of the retinal artery. Its pathophysiology remains unclear; however, early diagnosis and treatment make it possible to minimize neurological, ophthalmological, and auditory sequelae.7
Ischemia in CRA occlusion may occur owing to arterial atherosclerosis, embolism, vascular diseases, inflammatory diseases, or hypercoagulability. The main causes are carotid obstruction, valvular disease, and arterial fibrillation.8 In patients with no history of stroke, the risk after CRA occlusion increases between 4.8% and 35.5% within 3 years of eye diagnosis.
The most recognized cardiovascular risk factors for CRA occlusion include age, smoking, hypertension, hyperlipidemia, diabetes mellitus, and atherosclerosis. However, more recently, there has been a greater focus on the etiological role of thrombophilia.9
In the absence of a cardioembolic etiology, thrombophilia is a common and important cause. Types of thrombophilia include hyperhomocysteinemia, factor V Leiden (FVL) mutation, prothrombin gene (PTG) mutation G20210A, antithrombin III deficiency, protein C or S deficiency, and antiphospholipid syndrome. Among these, hyperhomocysteinemia is the most common.10 PTG mutation is a G-A transition in the nucleotide 20210 of the factor II gene, and it is associated with increased plasma prothrombin, resulting in a procoagulant state. It has a prevalence of 1%–4%, and it is more common among individuals of Caucasian ancestry. In addition, it is associated with venous thromboembolism (VTE), and recent literature has evidenced its significant role in the mediation of ocular vascular occlusion.9
Previous investigations on the role of thrombophilia in occlusive retinal vascular diseases have indicated that screening for thrombophilia in affected subjects should be selective. In particular, a remarkable personal or family history of thromboembolism and young age at the time of the first thromboembolic event appear to be strong indicators of an underlying thrombophilia disorder in CRA occlusion.10
Examinations to be requested in suspected thrombophilia include FVL, PTB G20210A gene mutation, dosage of protein C, protein S, antithrombin, coagulation factors VIII, VII, IX, and XI, and antiphospholipid and anticardiolipin antibodies.11
After the episode of sudden vision loss, our study patient underwent a hematological evaluation that confirmed the diagnosis of thrombophilia. She pre-arterial occlusion (arterial hypertension, smoking, sented three major risk factors for the occurrence of and thrombophilia).
In a prospective study of patients diagnosed with CRA occlusion, 32.3% had evidence of a previous stroke. Of these, 4.8% presented uncertain embolic etiology within 3 years of the diagnosis of CRA occlusion. The course of vision loss was ipsilateral to the occlusion diagnosis. Based on the known epidemiology of stroke, this study showed that patients may be at an increased risk of cerebral infarction when compared with healthy age-compatible controls.12
There is no consensus on the optimal treatment for CRA occlusion at the time of diagnosis, although some therapies have been proposed, such as the early administration of intravenous thrombolitics, eye massage to induce oscillation of IOP and thrombus clearance, reduction of IOP with oral acetazolamide, intravenous mannitol, topical timolol, or even anterior chamber paracentesis, hyperventilation to induce respiratory acidosis, vasodilation, and supplementary oxygen therapy.4 Even with the proposed therapies, the visual prognosis is poor and uncertain. Therapies such as topical antihypertensive drugs and eye massage were attempted in our patient even after the immediate period, but without positive results.
Treatment for thrombophilia is at the physician’s discretion, with options such as aspirin, aspirin plus clopidogrel, warfarin, and low-molecular-weight heparin. More recently, a study by Napal Lecumberri suggested that aspirin is the preferred option for treatment.11
Visual prognosis depends on how quickly therapeutic measures are taken; however, in general, it is poor. Only 17% individuals recover a functional visual acuity of the affected eye without treatment.8 In cases where the patient has a cilioretinal artery, the final visual acuity is generally better, ranging from 20/20 to 20/50 in 80% cases.13 Regarding systemic prognosis, in 5 years, mortality is approximately 40% and is usually related to myocardial infarction.
For the patient mentioned above, the hematologist chose to prescribe aspirin. The patient remains in semi-annual follow-up with a hematologist, a cardiologist, and an ophthalmologist.
Considering that most cases of OACR cause severe and irreversible visual loss, it is essential to determine the etiology of the disease and try to prevent contralateral eye and systemic involvement. Therefore, a multidisciplinary evaluation of patients and regular follow-up are recommended considering the systemic prognosis.
REFERENCES
1. Hayreh SS. Central retinal artery occlusion. Indian J Ophthalmol. 2018;66(12):1684-94.
2. Munro M, Andrews R, Hamilton RD, Palakkamanil M, Adatia FA. Unravelling the mechanism of combined cilioretinal artery and retinal vein occlusion: documentation of the oscillating blood flow column and a review of the literature. Can J Ophthalmol. 2019;54(5):e251-e254.
3. Tobalem S, Schutz JS, Chronopoulos A. Central retinal artery occlusion - rethinking retinal survival time. BMC Ophthalmol. 2018;18(1):101.
4. Mehta N, Marco RD, Goldhardt R, Modi Y. Central Retinal Artery Occlusion: Acute Management and Treatment. Curr Ophthalmol Rep. 2017;5(2):149-59.
5. Benjankar M, Sitaula S, Karki P. Ocular ischemic syndrome; A case report. Nepal J Ophthalmol. 2019 Jan;11(21):86-90.
6. Kim YH, Park KH, Woo SJ. Clinical Manifestations and Visual Prognosis of Cilioretinal Artery Sparing Central Retinal Artery Occlusion. Korean J Ophthalmol. 2020;34(1):27-34.
7. Macedo M, Furtado MJ, Barbosa I, Araujo M, Gomes M, Lume M, et al. Síndrome de Susac. Rev Sociedade Portuguesa de Oftalmologia. 2012;36:307-14.
8. Grory BM, Lavin P, Kirshner H, Scharag M. Thrombolytic Therapy for Acute Central Retinal Artery Occlusion. Stroke. 2020;51(2):687-95.
9. Schochman S, Gluech CJ, Hutchins RK, Patel J, Shah P, Wang P. Diagnostic ramifications of ocular vascular occlusion as a first thrombotic event associated with factor V Leiden and prothrombin gene heterozygosity. Clin Ophthalmol. 2015 Apr 3; 9:591-600.
10. Dixon SG, Bruce CT, Glueck CJ, Sisk RA, Hutchins RK, Jetty V, et al. Retinal vascular occlusion: a window to diagnosis of familial and acquired thrombophilia and hypofibrinolysis, with important ramifications for pregnancy outcomes. Clin Ophthalmol. 2016 Aug 9;10:1479-86.
11. Chapin J, Carlson K, Christos PJ, DeSancho MT. Risk Factors and Treatment Strategies in Patients With Retinal Vascular Occlusions. Clin Appl Thromb Hemost. 2015 Oct;21(7):672-7.
12. very MB, Magal I, Kherani A, Mitha AP. Risk of Stroke in Patients with Ocular Arterial Occlusive Disorders: A Retrospective Canadian Study. J Am Heart Assoc. 2019;8(3):e010509.
13. Brown GC, Shields JA. Cilioretinal arteries and retinal artery occlusion. Arch Ophthalmol. 1979;97(1):84-92.
AUTHOR’S INFORMATION




Financing: The authors declare that there is none.
Conflicts of interest: The authors declare that there are none.
Received on:
October 21, 2019.
Accepted on:
June 16, 2020.