Patrícia Vieira Paiva1; Amanda Wiviane Pereira1; Leandro de Mattos Fonseca Vieira2; Renata Cavanellas Fraga1
DOI: 10.17545/eOftalmo/2019.0023
ABSTRACT
We report the case of a patient with systemic lupus erythematosus who used 10 years of chloroquine and a further 6 years of hydroxychloroquine, evolving with retinopathy due to drug deposition, presenting all the classical changes of this pathology in the complementary exams and an unequal correlation between the visual computerized campimetry and the appearance of the lesion in the fundus of the eye. We did a research of the subject in the literature focusing on the screening of the patient to avoid the clinical picture that will be reported.
Keywords: Chloroquine; Hydroxychloroquine; Lupus.
RESUMO
Relatamos o caso de uma paciente portadora de lúpus eritematoso sistêmico que fez uso por 10 anos de cloroquina e mais 6 anos de hidroxicloroquina, evoluindo com retinopatia por depósito da medicação, apresentando todas as alterações clássicas dessa patologia nos exames complementares e uma correlação ímpar entre a campimetria visual computadorizada e o aspecto da lesão no fundo de olho.
Palavras-chave: Cloroquina; Hidroxicloroquina; Lúpus.
RESUMEN
Relatamos el caso de una paciente con lupus eritematoso sistémico que utilizó por 10 años cloroquina y más 6 años de hidroxicloroquina, evolucionando con retinopatía por depósito de la medicación, presentando todas las alteraciones clásicas de dicha patología en los exámenes complementarios y una correlación impar entre la campimetría visual computadorizada y el aspecto de la lesión en el fondo de ojo.
Palabras-clave: Cloroquina; Hidroxicloroquina; Lupus.
INTRODUCTION
Chloroquine and hydroxychloroquine, 4-aminoquinilone derivatives, are used in the treatment of malaria, systemic lupus erythematosus, rheumatoid arthritis, porphyria cutanea tarda, giardiasis, and amebic hepatitis. In addition, chloroquine is used to treat osteoarthrosis in association with analgesics and nonsteroidal anti-inflammatory drugs. They are melanotropic and therefore concentrate on ocular structures containing melanin [retinal pigment epithelium (RPE), choroid, and iris] and are very slowly eliminated from the body1.
Over time, the use of these drugs may cause maculopathy due to their deposition in the macular area; this can be diagnosed using fundoscopy. However, this exam only changes when there is already injury in the RPE. There are presently various methods that aid in early diagnosis, such as optical coherence tomography (OCT) and 10-2 computerized campimetry.
CASE REPORT
A female patient, V.L.S.S., 67-years-old, white, born in Rio de Janeiro, visited the Ophthalmology Department of the Federal Civil Servants' Hospital (HFSE) in Rio de Janeiro, Brazil, in March 2015, complaining that chloroquine had diminished her vision. On the first visit, the patient diagnosed with systemic lupus erythematosus; therefore took chloroquine for 10 years and hydroxychloroquine for another 6; she could not remember the doses. The latter drug was discontinued since 2013. Furthermore, she had photophobia and did not show the symptoms of burning, itching, or ocular pain. In addition, she denied any previous eye surgery, ocular trauma, or the use of eye drops.
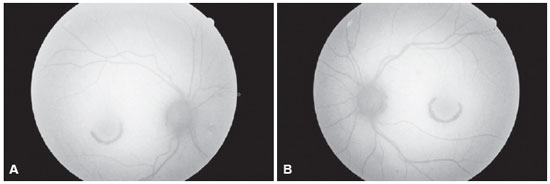
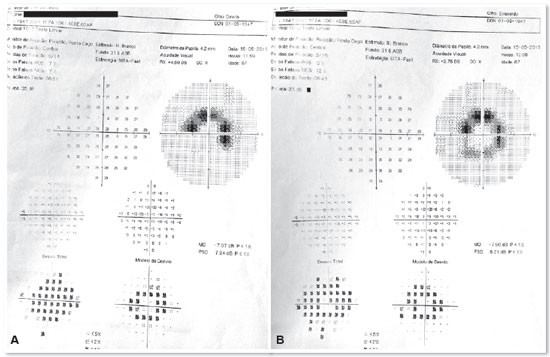
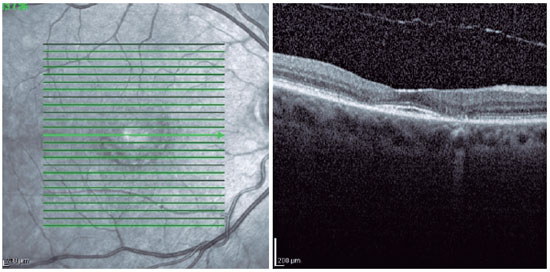
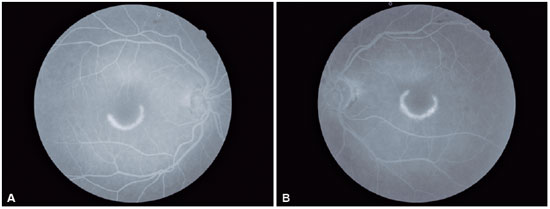
Ophthalmologic examination revealed a 20/30 visual acuity for the right eye (refraction: +1.25 SPH -0.75 CYL 45º) and 20/25 for the left eye (refraction: +0.50 SPH -0.75 CYL 10º). Biomicroscopy revealed the presence of 2+/4+ nuclear cataract in both the eyes. No further changes were observed. Fundoscopy revealed an optic disk of normal color, sharp edges, vessels with preserved caliber and path, and semicircular hypopigmented macular lesions in both the eyes, which were larger and more evident in the left eye, with a typical bull's eye maculopathy pattern (Figures 1A and 1B). Fundus autofluorescence showed semicircular hypoautofluorescent macular lesions in both the eyes (Figures 2A and 2B). Furthermore, 10-2 computerized campimetry indicated semicircular paracentral scotomas in both the eyes, larger in the left eye (Figures 3A and 3B). In addition, OCT of both the eyes revealed a flattened foveal profile, with loss of the photoreceptor inner segment/outer segment (IS/OS) junction in the perifovea and perifoveal thinning of the outer retina. Below the center of the fovea, the outer retina remained intact, resulting in an ovoid appearance. This OCT finding was is known as "the flying saucer sign" (Figures 4 and 5). Moreover, fluorescein angiography of both the eyes revealed ring hyperfluorescence, representing a circular window defect, which corresponded to the bull's eye lesion (Figures 6A and 6B).
DISCUSSION
The retinotoxicity of chloroquine and hydroxychloroquine is linked to the total cumulative dose1. In case of chloroquine, the risk of toxicity increases with a daily dose of >3mg/kg2. Moreover, hydroxychloroquine is much safer than chloroquine, and the risk is insignificant if the daily dose does not exceed 400mg. The risk of hydroxychloroquine increases with a daily dose of >6.5mg/kg2 for a duration of >5 years1. The maximum recommended daily doses for hydroxychloroquine and chloroquine are ≤5.0 and ≤2.3mg/kg real weight3. With these recommended doses, the risk of toxicity is <1% in 5 years and <2% in 10 years; however, it increases to almost 20% after 20 years3.
The macular damage caused by the use of chloroquine or hydroxychloroquine can be categorized into stages. The first one is known as premaculopathy, in which visual acuity is still preserved, and there may be a scotoma between 4 and 9 degrees in relation to fixation. At this stage, if the use of these drugs is discontinued, the visual function is normalized. In the second stage, known as early maculopathy, there is a slight reduction in visual acuity (20/30 to 20/40), with the presence of a bull's eye macular lesion. This may progress even if the use of drugs is discontinued. The third stage is known as established maculopathy, in which the decrease in visual acuity is moderate (20/60 to 20/80). The fourth stage is severe maculopathy, with a sharp reduction in visual acuity (20/120 to 20/200). The fifth and last stage is known as end-stage maculopathy and presents severe reduction in visual acuity, with marked atrophy of the RPE, unmasking of choroid vessels, arteriolar attenuation, and pigment aggregation in the periphery of the retina1.
Furthermore, chloroquine and hydroxychloroquine retinotoxicity may cause the following symptoms: central and paracentral scotoma, nyctalopia, dyschromatopsia, photophobia, photopsia, visual field constriction, and low visual acuity. Retinal changes begin with loss of the foveal reflex and abnormal pigmentation of the macula. At this point, it is reversible. As it progresses, the bull's eye lesion appears which is irreversible, in addition to bone spicule formation in the periphery of the retina, vascular attenuation, and optic disk pallor. The final stage may be similar to end-stage retinitis pigmentosa. In addition to retinal lesions, the patient may present poliosis and subepithelial corneal deposits, known as cornea verticillata4.
The most important methods for the diagnosis of patients and their follow-up are 10-2 computerized campimetry and OCT3. The patient may present paracentral scotoma as an early change in the visual field; this finding may precede the visual acuity decrease and the eye fundus changes. In Asian patients, a 30-2 visual field should ideally be used because they may have extramacular involvement3. The first change in spectral-domain OCT is in the ellipsoid zone, with a diminished number and thickness of the parafoveal photoreceptors. At this stage, there is no classic bull's eye lesion in the fundus, which means this finding can precede fundoscopic changes. If the use of drug is discontinued at this stage, the condition may cease to progress; however, if there is RPE involvement, it will progress. Another possible OCT finding is the flying saucer sign, which indicates the loss of the photoreceptor inner segment/outer segment (IS/OS) junction in the perifovea and perifoveal thinning of the outer retina5. Below the center of the fovea, the outer retina remains intact, resulting in an ovoid appearance.
Other optional methods for assessment are as follows: Amsler grid presenting scotoma6, although it is inconsistent for screening3; fluorescein angiography indicating hypofluorescence, with a hyperfluorescence ring corresponding to a bull's eye lesion4 (circular window defect), a finding from a later stage because it indicates RPE involvement, which occurs after photoreceptor impairment; electrooculogram showing late reduced Arden index (<1,6)4; electroretinogram (ERG) with an abnormal pattern, with multifocal ERG being better for detection because it shows early changes with loss of the foveal peak7 as well as a sensitivity similar to that of visual field; and fundus autofluorescence showing early photoreceptor involvement with hyperautofluorescent areas and RPE involvement later with hypoautofluorescent areas3.
The risk factors for toxicity are as follows: doses of >6.5mg/kg/day for hydroxychloroquine and >3mg/kg/day for chloroquine (the main risk factor), liver and kidney diseases, age >60 years, use of these drugs for >5 years8, tamoxifen use, and previous macular degeneration or dystrophy3. In addition, patients with kidney failure require lower doses3.
The follow-up of patients taking chloroquine or hydroxychloroquine should be done by an ophthalmologist. It should start with fundoscopy within the first year of the administration of the drug to rule out pre-existing maculopathies and have a baseline examination. If the patient presents previous maculopathy, it should be documented with computerized campimetry and OCT3.
The annual screening should be initiated after the fifth year of drug use in patients without risk factors and those taking acceptable doses. If the patient presents any risk factor, an early screening should be considered as well as reassessing the patient more frequently in a year3.
Whenever a sign of toxicity is observed, the drug should be discontinued in conjunction with a rheumatologist's opinion because it may lead to worsening of the autoimmune condition. Moreover, ceasing the use of the drug does not guarantee that the toxic effects will not progress because the clearance of the drug is slow9.
CONCLUSION
Patients taking chloroquine or hydroxychloroquine should be followed-up by an ophthalmologist. In addition to visual acuity assessment, biomicroscopy, and fundoscopy, it is important to perform a visual field examination and OCT because they show early changes. The typical bull's eye maculopathy occurs when there is a lesion in the RPE, after the damage to the photoreceptors. The patient in the present report continues to be monitored in the HFSE Ophthalmology Department. The use of the drugs has been discontinued since 2013. Since her first visit to HFSE in March 2015, the lesion has shown no progress on fundoscopy, OCT, or campimetry. In addition, her visual acuity has not worsened.
ACKNOWLEDGMENTS
We thank Dr. Vitor Barbosa Cerqueira for his guidance and support in conducting this case report.
REFERENCES
1. Kanski JJ, Bowling B. Oftalmologia clínica: uma abordagem sistemática. 7ª ed. Rio de Janeiro: Elsevier; 2012.
2. Yannuzzi LA. The Retinal Atlas. 1st ed. New York: Elsevier Saunders; 2010.
3. Marmor MF, Kellner U, Lai TY, Melles RB, Mieler WF. Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revision). Ophthalmology. 2016 Jun;123:(6):1386-1394.
4. Kaiser PK, Friedman NJ, Pineda R. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 3rd ed. Rio de Janeiro: Elsevier; 2011.
5. Chen E, Brown DM, Benz MS, Fish RH, Wong TP, Kim RY, et al. Spectral domain optical coherence tomography as an effective screening test for hydroxychloroquine retinopathy (the "flying saucer" sign). Clin Ophthalmol. 2010 Oct;4:1151-8.
6. Almony A, Garg S, Peters RK, et al. Threshold Amsler grid as a screening tool for asymptomatic patients on hydroxychloroquine therapy. Br J Ophthalmol. 2005 Apr;89(5):569-74.
7. Gilbert ME, Savino PJ. Missing the bull's eye. Surv Ophthalmol. 2007 Jul/Aug;52(4):440-442.
8. McCannel CA. Retina and Vitreous. In: Cantor LB, Rapuano CJ, McCannel CA, editors. Basic and clinical science course (BCSC). San Francisco, CA: American Academy of Ophthalmology; 2014-2015. p.266-267.
9. Yanoff M, Duker JS. Oftalmologia. 3rd ed. Rio de Janeiro: Elsevier; 2011.


Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
February 20, 2019.
Accepted on:
August 12, 2019.