Francyne Veiga Reis Cyrino; José Augusto Cardillo; Elizabeth Regina Negri Barbosa; Neide Aparecida de Souza Lehfeld; Eliana Mendes de Souza Teixeira Roque
DOI: 10.17545/eoftalmo/2019.0013
ABSTRACT
OBJECTIVE: To identify profiles of family health strategy (FHS) professionals and evaluate their knowledge on the correct procedure to deal with complications such as diabetic retinopathy (DR) in patients with diabetes and to recommend simple strategies to speed up the process of DR diagnosis.
METHODS: A qualitative, descriptive, cross-sectional study was conducted with FHS teams from two cities in Brazil: Ribeirão Preto (in the State of São Paulo) and Teixeira de Freitas (in the State of Bahia). The study included a total of 42 professionals, including physicians, nurses, and community agents (CAs), who participated in semi-structured interviews. Actions and strategies to speed up DR diagnosis and treatment were recommended based on the analysis of these interviews.
RESULTS: The professionals interviewed in this study demonstrated little-to-no knowledge about the management, diagnosis, treatment and follow-up of DR in patients with diabetes. Moreover, ongoing professional training programs are not appropriately conducted and protocols for chronic diseases are not strictly followed. Based on these findings, the use of informative posters, strategies for CAs, incorporation of reminders in automated service systems and a “RED PROTOCOL” are proposed.
CONCLUSION: Professionals of FHS could benefit from better training on strategies regarding diagnosis, awareness and guidance of DR besides the countless benefits for diabetic patients though the agility of diagnosis and treatment.
Keywords: Diabetic Retinopathy; Diabetes; Family Health Strategy; Health Personnel.
RESUMO
OBJETIVO: identificar o perfil de profissionais da estratégia saúde da família (ESF) e verificar o conhecimento sobre como proceder corretamente com os pacientes diabéticos quanto a complicações como a retinopatia diabética (RD). A partir disso, indicar estratégias simples para acelerar o diagnóstico da RD.
MÉTODOS: foi realizado um estudo qualitativo-descritivo de delineamento transversal com equipes da Estratégia Saúde da Família (ESF) de dois estados brasileiros distintos: Ribeirão Preto/SP e Teixeira de Freitas/BA. Foram envolvidos médicos, enfermeiros e agentes comunitários (AC) (42 profissionais), que participaram de entrevistas semiestruturadas. A partir desta análise, foram indicadas ações e estratégias para acelerar o diagnóstico da RD e o tratamento.
RESULTADOS: os profissionais ouvidos nesta pesquisa demonstram pouco ou nenhum conhecimento sobre como proceder com pacientes diabéticos em relação à RD, seu diagnóstico, tratamento e seguimento. Ainda, os programas de atualização não são devidamente cumpridos e nem os protocolos de doenças crônicas são seguidos à risca. Com isso, é proposta a utilização de cartazes informativos, estratégias para ACs, agregação de lembretes nos sistemas automatizados de atendimento e um protocolo vermelho.
CONCLUSÃO: os profissionais poderiam receber uma maior capacitação sobre a RD, com disponibilidade de estratégias para alertar, orientar e realizar o diagnóstico dos pacientes.
Palavras-chave: Retinopatia Diabética; Diabetes; Estratégia Saúde da Família; Profissionais de saúde.
RESUMEN
OBJETIVO: Identificar el perfil de profesionales de la Estratégia Saúde da Família (ESF- Estrategia Salud de la Familia) y verificar el conocimiento sobre cómo proceder correctamente con los pacientes diabéticos en caso de complicaciones como la retinopatía diabética (RD). A partir de ello, indicar estrategias simples para acelerar el diagnóstico de la RD.
MÉTODOS: se ha realizado un estudio cualitativodescriptivo de delineamiento transversal con equipos de Estrategia Salud de la Familia (ESF) en dos Estados brasileños distintos: São Paulo, en la ciudad de Ribeirão Preto; y Bahia, en la ciudad de Teixeira de Freitas. Se han sumado médicos, enfermeros y agentes comunitarios (AC) (42 profesionales), quienes participaron en entrevistas semiestructuradas. Desde ese análisis, se recomendaron acciones y estrategias para acelerar el diagnóstico de la RD y el tratamiento.
RESULTADOS: los profesionales que se han escuchado en dicha investigación demuestran poco o ningún conocimiento sobre cómo proceder con pacientes diabéticos con relación a la RD, su diagnóstico, tratamiento y seguimiento. Además, los programas de actualización no son debidamente cumplidos, tampoco los protocolos de enfermedades crónicas son seguidos rigurosamente. Así, se propone la utilización de carteles informativos, estrategias para ACs, implementación de recordatorios en los sistemas automatizados de servicio y un protocolo rojo.
CONCLUSIÓN: los profesionales podrían recibir una mayor capacitación sobre la RD, con disponibilidad de estrategias para alertar, orientar y realizar el diagnóstico de los pacientes.
Palabras-clave: Retinopatía Diabética; Diabetes; Estrategia de Salud Familiar; Personal de Salud.
INTRODUCTION
There are approximately 13 million patients with diabetes mellitus (DM) among Brazilian adults aged 20–79 years, which makes Brazil the fourth largest country in terms of number of diabetic individuals1. DM is caused by defective insulin secretion or action, which results in a state of chronic hyperglycemia2. Type 2 DM (T2DM), characterized by defective secretion of insulin or resistance to it, comprises 90%–95% of all DM cases3. High plasma glucose levels lead to the development of chronic degenerative lesions associated with the failure of several organs, particularly the eyes, kidney, heart, nerves, and blood vessels4.
Thus, a patient with diabetes has a nearly 30-fold higher risk of attaining blindness than a patient without diabetes5. One of the most important microvascular complications associated with DM is diabetic retinopathy (DR), which is considered to be the leading cause of new blindness cases among USA americans aged 20–64 years6. It is estimated that 50% of patients with DM in Brazil are affected by DR at some point in their lives, and DR is the cause of 7.5% of all cases of adult disability at the workplace and 4.8% of cases of visual deficit5,7,8.
DR involves damage to the retina, the nervous layer in the fundus of the eye, owing to malfunctioning of the blood–retina barrier of capillary vessels, which is in turn caused by high glucose levels in the bloodstream as a result of inadequate diabetes control and the duration of the disease8,9. The changes in the fundus in a patient with diabetes occur gradually, starting with mild, nonproliferative DR, characterized by increased vessel permeability, and reaching the stage of severe, proliferative DR with neovascularization10.
Visual loss from diabetes can be avoided or minimized with appropriate clinical control and local or systemic treatment11. A study conducted in the city of Ribeirão Preto, State of São Paulo, reported that there was little regular preventive ophthalmologic follow-up of patients with diabetes, who reported that their most recent evaluation had been conducted more than 2 years prior, and 14% of patients stated that they had never visited an ophthalmologist9. Therefore, health professionals play a key role in referring these patients to specialized ophthalmological consultations in a timely manner, thereby promoting earlier and more efficient diagnosis9. However, it is possible that primary healthcare professionals are to some extent unaware of DR and of the appropriate procedures to be followed in the management of patients with diabetes.
Thus, this study aimed to identify the profile of family health strategy (FHS) professionals and evaluate their knowledge on the appropriate management of complications such as DR in patients with DM and recommend simple strategies to speed up the process of DR diagnosis.
METHODS
This study is part of a larger research program and was approved by the Committee of Ethics in Research and meets the requirements resolutions no. 466 of December 12, 2012 and no. 510 of April 7, 2016 of the Brazilian National Health Council. The professionals involved in this study had the requisite specialization and therefore had knowledge about the appropriate follow-up of patients with diabetes in terms of fundoscopy changes.
A qualitative, descriptive, cross-sectional study was conducted with FHS teams from two cities in different Brazilian states: Ribeirão Preto (State of São Paulo) and Teixeira de Freitas (State of Bahia), in 2016.
The study participants were FHS professionals: physicians, nurses, and community agents (CAs). In Ribeirão Preto, 25 participants (5 physicians, 5 nurses, and 15 CAs) participated in the study; in Teixeira de Freitas, 17 professionals (4 physicians, 3 nurses, and 12 CAs) participated. The cities were selected randomly in states with a high prevalence of DM but were also based on the Human Development Index, which is considered high in Ribeirão Preto (0.79) and medium in Teixeira de Freitas (0.68). In terms of sampling design, in a qualitative social study, the sample composition does not represent size but rather the complexity of the object of the study12.
Data collection was divided into two phases. First, professionals were asked to fill an identification form with questions about their age, gender, professional background, and extent of ongoing training on diabetes. The second phase comprised a semi-structured oral interview composed of both free-text and multiple-choice questions on the advice and follow-up they provided to patients with diabetes. The interviews were recorded after obtaining the interviewee’s consent through a Free and Informed Consent form.
Data were analyzed using the content analysis technique. This technique involves finding clusters of sense that comprise a message, using multiple communication analysis techniques through systematic and objective procedures to describe the content of messages, analyzing the content of figures of speech, incomplete and implied statements, as well as explicit ones13. Theme analysis started with a pre-analysis step, which was followed by exploration of the material, processing of the obtained results, and finally interpretation of the results14.
The findings from the interviews were used as a basis for the proposal of strategies that health professionals can use to diagnose DR at an early stage and treat it efficiently.
RESULTS AND DISCUSSION
Profile and academic background of the professionals
Of the physicians interviewed in both cities, three (33.3%) were female and six (66.6%) were male, aged 28–61 years. Time since graduation varied from 6 months to 36 years. Three physicians were specialized in family medicine, two in family and community medicine, and one had a graduate degree in comprehensive women’s healthcare. Of these professionals, seven (77.7%) had attended an update program on diabetes in the previous 3 years.
All eight nurses of both states interviewed were females aged 28–55 years and had graduated 3–15 years back. Time of work in FHS varied from 6 months to 15 years. Additionally, three in five nurses from Ribeirão Preto had a postgraduate degree (60%). Only five nurses (62.5%)from both states had attended an update course on diabetes in the previous 3 years.
The 27 CAs interviewed were aged 24–57 years and were predominantly female (85.2%). Time of work as a CA ranged between 3 months and 20 years. Thirteen CAs (48.1%) had completed high school, 3 (11.1%) had incomplete high school education, and 11 (40.7%) completed university studies in various fields. Only 16 (59.2%) reported having attended an update program on diabetes in the previous 3 years.
A previous study assessed the knowledge of primary healthcare professionals (physicians, nurses, social workers, dentists, psychologists, nursing technicians, and nursing assistants) about diabetes and reported that a large percentage of professionals had deficient knowledge of the concept of the disease (64%); symptoms (66%); classification (54%); pathophysiology (36%); risk factors (58%); and complementary tests (42%)15. These results indicate a need for continuous education of healthcare teams. However, in the present study, some professionals did not attend update courses, particularly CAs who have more direct contact with families in the community16.
Knowledge of professionals about the management of diabetic patients
When the professionals were asked about the diagnosis, treatment, and referral of patients with diabetes (Table 1), it was noted that there were knowledge gaps. The physicians’ statements about the need to perform fundoscopy examinations were associated with the patient’s complaints of visual difficulties and the duration of diabetes. Indeed, the percentage of patients with diabetes with DR increased with time since the onset of disease. It is estimated that after 25 years, 80% of patients with DM patients will present some degree of DR5. However, the physicians who participated in this study were unaware that ophthalmological evaluation of patients with DMT1 should be first performed 5 years after diagnosis and subsequently every year and that screening of patients with DMT2 should be performed annually since diagnosis17. These data reiterate the importance of update training on this subject to allow proper advice to be given to patients.
DR control and follow-up are performed primarily by fundoscopy, as well as by using a retinal fundus camera, which takes photographs of the retina and is considered the method with the most adequate sensitivity and specificity18. Yet when the professionals’ statements were correlated to clinical practice, severe cases that could have been treated earlier if diagnosis and referral had been properly performed were identified. If fundoscopy was performed by FHS physicians, as determined by the Competence-Based Curriculum for Family and Community Medicine19, earlier detection of fundus changes could have been possible, although training is required for that. In the era of information technology, installing retinal fundus cameras in healthcare units and creating remote reading centers by retina specialists for telemedicine could also be a good alternative for DR screening, facilitating earlier diagnoses and referrals to the most qualified professional in DR treatment, i.e., the ophthalmologist specialized in retina and vitreous, a retina specialist.
In the present study, it was observed that nurses and CAs are unaware of the diagnostic methods for DR diagnosis and treatment or how often patients with diabetes should be referred to the ophthalmologist (Table 1). In addition to the answers shown in Table 1, the professionals made statements as follows:
Nurse 3: We do not treat or refer anyone. The doctor does that. What we do is advise patients if they complain of any difficulty. If they wear glasses and complain that their vision is bad, we advise them to see an ophthalmologist.
CA 9: What we do is advise the patients. When someone says that their vision is bad or they are not seeing much, we advise them to go and check that. There is a diabetic boy in my area who can barely see anything.
CA 10: We healthcare agents do not refer anyone as that is not our role, but if we detect anything when they visit us, we inform the doctor.
According to the attributions delegated to nurses and CAs, these professionals should, in general, contribute to the promotion of health and prevention of complications16. Thus, both can be provided tools to aid their work and advice to patients with diabetes. We believe that nurses and CAs need more autonomy because they are closest to the patients and their families and know their surroundings, needs, and difficulties.
A study in 2016 reported that the leading concerns among patients with diabetes were limb amputation (32%) and blindness (32%). The same study reported that 18% did not know the type of diabetes that they had20. It should be emphasized that factors associated with the knowledge and attitude of patients with diabetes must be especially considered by public healthcare professionals21 and that professionals must create awareness and provide the necessary information on self-care, treatment, and prevention of DMT2 to reduce health complications.
Therefore, there is a need to develop new public health policies targeting a multidisciplinary approach toward the awareness, not only of patients with diabetes but also healthcare professionals21. Moreover, members of the multidisciplinary FSH team should discuss among themselves to determine if their interventions lead to positive results or require further actions, changes or the addition of new drugs. The presence, absence, or progression of DR can guide the choice of drugs that favor glycemic control. Because the main form of prevention of microvascular complications is their early detection, the current situation is unfavorable because referrals to fundoscopic examination are primarily based on visual loss complaints. Moreover, another factor that delays DR diagnosis and treatment is the long waiting time between the referral by the primary-care physician and the specialized medical consultation, which occurs because of the slowness of the Brazilian Unified Health System22.
Therefore, there is a need to use tools to complement the advice and information on DM and contribute to earlier DR diagnosis and, consequently, earlier treatment. Additionally, these tools should not only promote the ability of healthcare agents to identify DR but also increase awareness and educate the diabetic population and other FHS users regarding their responsibility and the prevention of their illness and efforts for early diagnosis.
Proposed strategies to speed up DR diagnosis
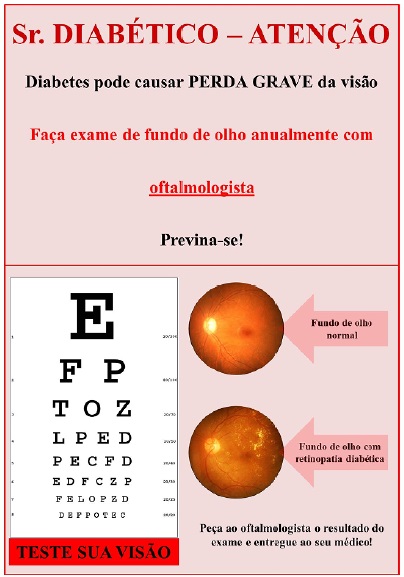
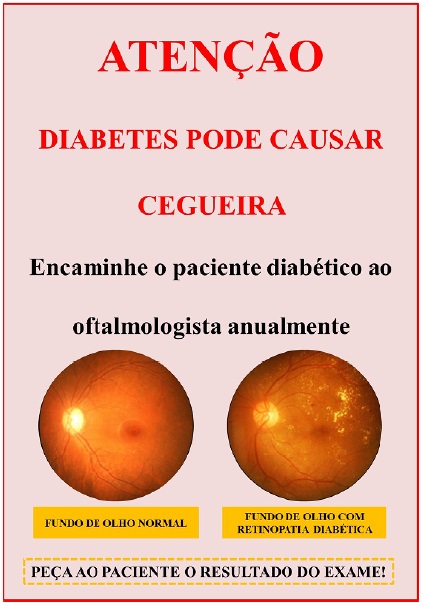
In view of the above, it is considered necessary for patients with diabetes and those in their care to be aware that the disease may affect the eyes, leading to loss of vision, and that treatment exists, which when initiated in a timely manner, allows sequelae to be minimal and vision to be preserved. From this premise, instruments with high visibility are proposed to promote DR awareness in an easy and simple manner. For this purpose, posters with awareness messages for patients with diabetes can be displayed, as shown in Figure 1. These posters can also contain the classic Snellen chart with instructions to perform self-examination, making it possible for the patient to identify any existing visual difficulty. These posters can be placed in the waiting rooms of primary healthcare centers in a suitable location and at the correct height to perform the test. However, this should not replace an ophthalmological examination. A different poster targeting physicians and nurses can be displayed in consultation rooms with an awareness message on the need to annually refer patients with diabetes to an ophthalmologist (Figure 2).
Additionally, we propose that CAs incorporate a simple test into their work routine, as suggested by a previous study23, with modifications. We suggest that CAs add to their work bag an “E”-shaped optotype (LogMar 0.3 or Snellen 20/40 size) and a one-meter long cord to perform a visual acuity screening test at the patient’s homes. For this, the patient should hold one extremity of the cord and the CA the other one; the CA should then stand 1 meter away and present the optotype, asking the patient to identify it, covering one eye at a time. If the patient cannot identify the optotype, then he or she has reduced visual acuity and should be referred to an ophthalmologist.
Additionally, because services are presently computerized, city administrations and FHS facilities are able to include a reminder in the system in the form of a “pop-up box” that appears on the screen whenever a patient with diabetes is seen. This box could have the following text: “Alert! Diabetic patient: request an ophthalmological fundus examination.” This alert pop-up box can also include other important reminders, e.g., assessment of the risk of diabetic foot.
Furthermore, physicians of FSH can be trained in fundoscopy using a direct ophthalmoscope and attend further training classes taught by a retina specialist in which simple language and clear illustrations are used, so that everyone can become familiarized with the fundoscopic findings of DR. Expository activities on DR could even be extended to patients with diabetes as to other users of healthcare units and other people from the community to increase the awareness of self-care and promote debates to clarify questions and provide advice.
Regarding the treatment, we suggest that an emergency protocol should be created after diagnosis, the “RED PROTOCOL” for agility in the treatment of the most advanced and urgent DR cases - in the current system, the patient is referred by the healthcare network to an ophthalmologist, who then may diagnosis or not the DR. Once diagnosis is performed, the patient returns to the healthcare network to be referred to a retina specialist and subsequently be treated. The waiting time involved is often very long because of the system being overburdened by a largely unmet demand. In many cases, when the patient finally visits the retina specialist, the is condition worst then before, sometimes complicated with tractional retinal detachment and surgical indication and unfavorable prognosis, risking permanent loss of vision. The “RED PROTOCOL” would facilitate quicker and direct referral to the retina specialist (without first visiting the general ophthalmologist), making it possible for treatment to start earlier and a better final prognosis to be achieved, with less impact social, financial and welfare subsequent.
Final considerations
The professionals interviewed in this study demonstrated little knowledge about the management, diagnosis, treatment and follow-up of DR in patients with diabetes. Moreover, ongoing professional training programs are not adequately attended and protocols for chronic diseases are not strictly followed.
It is extremely important to identify these issues to increase the ability of the FHS network to resolve DR cases. Healthcare professionals should be able to prevent complications by thoroughly addressing aggravating factors. For this reason, the strategies proposed in this study can be essential for the early diagnosis of visual changes in individuals with diabetes because these tools are targeted not only at healthcare professionals but also the community, thus allowing greater dissemination of information and timely diagnosis, treatment, and most importantly, prevention of blindness.
REFERENCES
1. International Diabetes Federation. IDF Diabetes Atlas. 8th ed. Bruxelas, Bélgica: International Diabetes Federation. 2017; [citado 2018 ago 14]. Disponível em: http://diabetesatlas.org/IDF_Diabetes_Atlas_8e_interactive_EN/
2. Rossaneis MA, Gvozd R, Andrade SM, Pissinati PSC, Haddad MCL. Fatores associados ao controle glicêmico de pessoas com diabetes mellitus. Cien Saude Colet [periódico na internet]. 2017 mai; [citado 2018 ago 24]; 24(03):997-1005. Disponível em: http://www.cienciaesaudecoletiva.com.br/artigos/fatores-associados-ao-controle-glicemico-de-pessoas-com-diabetes-mellitus/16223A\
3. American Diabetes Association (ADA). Standards of medical care in diabetes - 2016. Diabetes Care. 2016 jan;39(Suppl 1):1-112.
4. Barbosa JHP, Oliveira SL, Seara LT. Produtos da glicação avançada dietéticos e as complicações crônicas do diabetes. Rev Nutr. 2009 jan/fev;22(1):113- 24.
5. Ávila M, Alves MR, Nishi M. As condições de saúde ocular no Brasil. 1ª ed. São Paulo: Conselho Brasileiro de Oftalmologia; 2015.
6. Schubert HD. 2013-2014 Basic and Clinical Science Course, Section 12: Retina and Vitreous. San Francisco, USA: American Academy of Ophthalmology. 2012; [citado 2018 Ago 27]. Disponível em: https://yyyt9gl01.storage.googleapis.com/MTYxNTI1Mzg4Mg==01.pdf
7. Caird FI, Burditt AF, Draper GJ. Diabetic retinopathy: a further study of prognosis for vision. Diabetes. 1968 mar;17(3):121-3.
8. Boelter MC, Azevedo MJD, Gross JL, Lavinsky J. Fatores de risco para retinopatia diabética. Arq Bras Oftalmol. 2003;66(2):239-47.
9. Alves PA, Santos RWV, Sobrinho EFA, Rocha SPL, Loch ACN. Retinopatia em pacientes hipertensos e/ou diabéticos em uma unidade de saúde da família. Rev Bras Oftalmol. 2014;73(2):108-11.
10. Engerman RL. Pathogenesis of diabetic retinopathy. Diabetes. 1989 oct;38(10):1203-6.
11. Motta MMS, Coblentz J, Melo LGN. Aspectos atuais na fisiopatologia do edema macular diabético. Rev Bras Oftalmol. 2008 feb;67(1):45-9.
12. Minayo MCS. O desafio do conhecimento: pesquisa qualitativa em saúde. 4ª ed. São Paulo: HUCITEC; 1996.
13. Bardin L. Análise de conteúdo. Lisboa: Edições 70; 1977.
14. Minayo MCS, Deslandes SF, Gomes R. Pesquisa Social: teoria, método e criatividade. Minayo MCS, organizadora. 29ª ed. Petrópolis (RJ): Vozes; 2010.
15. Torres HC, Amaral MA, Amorim MM, Cyrino AP, Bodstein R. Capacitação de profissionais da atenção primária à saúde para educação em Diabetes Mellitus. Acta Paul Enferm. 2010;23(6):751-6.
16. Junqueira SR. Competências profissionais na estratégia Saúde da Família e o trabalho em equipe. Módulo Político Gestor. 2008; [citado 2018 ago 14]. Disponível em: http://www.unasus.unifesp.br/biblioteca_virtual/esf/1/modulo_politico_gestor/Unidade_9.pdf
17. American Diabetes Association (ADA). Standards of Medical Care in Diabetes – 2013. Diabetes Care. 2013 jan;36(Suppl 1):11-66.
18. Scottish Intercollegiate Guidelines Network. Management of diabetes: a national clinical guideline. Healthcare Improvement Scotland [online]. 2010 mar; [citado 2016 mar 13]. Disponível em: https://www.sign.ac.uk/assets/sign116.pdf
19. Lermen Junior N, organizador. Currículo Baseado em Competências para a Medicina de Família e Comunidade. Sociedade Brasileira de Medicina de Família e Comunidade (SBMFC); 2015.
20. Almeida-Pititto B, Dias ML, Moraes ACF, Ferreira SR, Franco DR, Eliaschewitz FG. Type 2 diabetes in Brazil: epidemiology and management. Diabetes Metab Syndr Obes. 2015 jan;2015(8):17-28.
21. Lima AP, Benedetti TRB, Rech CR, Cardoso FB, Portella M. Conhecimento e atitude sobre a diabetes tipo 2 em idosos: Estudo de base populacional. Cien Saude Colet [periódico na internet]. 2018 jul; [citado 2018 ago 26]. Disponível em: http://www.cienciaesaudecoletiva.com.br/artigos/conhecimentoe-atitude-sobre-a-diabetes-tipo-2-em-idosos-estudo-de-base-populacional/16894
22. Vieira EWR, Lima TMN, Gazzinelli A. Tempo de espera por consulta médica especializada em um município de pequeno porte de Minas Gerais, Brasil. Rev Min Enferm. 2015 jan/mar;19(1):65-71.
23. Kuper H, Polack S, Limburg H. Avaliação rápida da cegueira evitável. Community Eye Health. 2006 dez;19(60):68-9.





Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
October 24, 2018.
Accepted on:
May 25, 2019.