Harley E. A. Bicas**
DOI: 10.17545/eoftalmo/2018.0038
ABSTRACT
Revision of changes in diagnostic and therapeutic methods, clinical and surgical of strabismus, mainly related to studies carried out by the author.
Keywords: Cycloplegia; Diagnostic methods; Viscosity; Magnetic Fields; Strabismus Surgery.
RESUMO
Revisão de mudanças de métodos diagnósticos e terapêuticos, clínicos e cirúrgicos dos estrabismos, principalmente relacionados a estudos protagonizados pelo autor.
Palavras-chave: Cicloplegia; Métodos diagnósticos; Viscosidade; Campos magnéticos; Cirurgias dos estrabismos.
RESUMEN
Revisión de cambios de métodos diagnósticos y terapéuticos, clínicos y quirúrgicos de los estrabismos, principalmente relacionados a estudios protagonizados por el autor.
Palabras-clave: Cycloplegy; Métodos Diagnósticos; Viscosidad; Campos Magnéticos; Cirurgía de Estrabismo.
Vision, the sense on which ophthalmology and all ophthalmological care is founded, is one of the most fascinating subjects in human knowledge. The eyes, the organs at the start of vision, require a huge and complex set of variables to function, including coordination of their positions. It is, therefore, not surprising that the study of strabismus — the field of knowledge on eye coordination, which enables proper binocular vision — raises so many passions and embarrassment, either for the number of influencing factors or for the nature of its subtleties. Indeed, twelve external eye muscles innervated by three of the twelve pairs of cranial nerves and receiving commands from multiple structures of the central nervous system do not make this a simple subject. Although “each case is different” is a proverbial concept in Medicine as a whole, this maxim is particularly important for strabismus.
My academic life has aimed at analyzing the characteristics of strabismus thoroughly. Upon being invited to discuss this topic, I revisit what I consider the main considerations from my academic life.
BACKGROUND
As a result of the continued accumulation and renewal of scientific knowledge in its several fields, ophthalmology has also been divided into “subspecialties” to allow the necessary further developments to be reached to a greater extent. Strabismus was one of the first to become a separate field of study. Indeed, while in some ophthalmology fields interest groups dedicated to debate their topics were only beginning to be formed, there were already organizations being consolidated to study strabismus and its correlations: the Consilium Europaeum Strabismi Studio Deditum (CESSD, 1961) — which became the European Strabismological Association in 19821 ---, the Japanese Association of Strabismus and Amblyopia (1964)2 and the International Strabismological Association (1966)2,3. In the USA, an informal “Squint Club” (with meetings since 1955) preceded the American Association for Pediatric Ophthalmology (1974)3. In Latin America (preceded only by CESSD and JASA), the Latin American Council on Strabismus was formed (1966)4 and inspired the formation of the Brazilian Strabismus Center (1967), the CBE, the first “specialty society” within Brazilian ophthalmology. The second one, the Brazilian Society of Contact Lenses and Cornea, would arise only in 1971, and the third one, the Brazilian Society of Ocular Plastic Surgery, in 1974 — when CBE was already in its ninth scientific conference.
All this association effervescence may have been influenced by the development of orthoptics, an area dedicated to strabismus diagnostic tests and non-surgical treatments. Indeed, as diagnostic procedures related to strabismus demanded a lot of time and became increasingly complex, they started being delegated to paramedical professionals in 1930, becoming particularly relevant after World War II (1939-45). In the 1960s, orthoptics reached a peak in quality (extensive and diversified methods and techniques for examination and clinical treatment) and quantity (a large number of professionals prepared to use these methods and techniques). To exemplify the prominence of orthoptics in topics related to strabismus, it is enough to mention that, of the founders of the Brazilian Strabismus Center, ten were ophthalmologists and eleven were orthoptists.
That was what might be called the “sensorial period” of strabismus studies, that is, the time of the emphasis on sensory (visual) processes and disorders related to positional inaccuracies of the visual axes (oculomotor deviations), either as causes or as consequences. Even in academic circles of basic science, the attention given to the studies of the physiology of vision at the time can be illustrated by the Nobel prizes in Physiology or Medicine in 1967 (Ragnar Granit, Haldan K. Hartline, and George Wald, “for their discoveries concerning the primary physiological and chemical visual processes in the eye”) and 1981 (David H. Hubel and Torsten N. Wiesel, “for their discoveries concerning information processing in the visual system,” published mainly between 1963 and 1967).
Thus, a good ophthalmology facility should have among its education and health care personnel at least one orthoptist and several instruments of orthoptics (the most used being the synoptophore) and pleoptics (stimulation techniques for the recovery of mono- and binocular vision). These were the conditions of the Department of Ophthalmology of the Ribeirão Preto Medical School of the University of São Paulo when I began my residency in ophthalmology, in 1963. Gilda Baptista Soares De Sordi was the orthoptist in charge of the examinations and treatment follow-up of strabismic patients. Doctors were responsible for surgeries. And, precisely in that year, Gilda got pregnant and had to go on maternity leave. To calm down the head of Department, enraged by the perspective of loss of quality in strabismic patient care, Gilda decided to teach the first-year residents (me and one other colleague) the science and art of orthoptics, initiating us in the handling of the essential (at the time) but obscure synoptophore. Maybe without Guy, the blessed fruit of that pregnancy, my academic path would have been different: my first paper (still as a sixth-year student and department monitor) was on intraocular pressure; my first studies in the (biochemistry) laboratory discussed the composition of vitreous humor; and my doctoral thesis was on keratometry. The fact is that I was soon (in October 1964) hired as a lecturer (“instructor”) at the department from which I had graduated and assigned to coordinate the activities of the Strabismus Division because of both my engagement in the subject (nobody else wanted it) and my inclination and pleasure in performing these activities. And I appreciate that this has been my academic history.
THE SENSORIAL PERIOD
Suppression used to be measured by a synoptophore according to its extent (different figures presented to each eye, to assess the resulting simultaneous binocular perception) as foveal if simultaneous binocular perception was present even when images were very small; as macular, if there was cortical neutralization of only one of them in very limited central areas, corresponding to the fovea of one of the eyes; peripheral when they were larger; or, finally, absent when the patient reported no simultaneous binocular visual perception. Suppression depth also used to be measured by a colored transparent filter used in front one of the eyes to reveal diplopia, while the patients fixed their gaze to a light, being greater (more intense suppression, worse binocularity) when the color of this transparent filter used was denser. In this simultaneous perception condition, the magnitude of the angle formed by the respective visual axes during fixation — that is, the deviation between them — was the “basic” measure of strabismus (or heterophoria). “Retinal correspondence” was considered normal (N.R.C.) if the “objective” measurement of the deviation coincided with the “subjective” measurement (the angle between the visual axes in which the patient reported simultaneous perception), or abnormal (A.R.C.), if these measures were different from each other. When detected, A.R.C. was classified by type (harmonious, unharmonious) and intensity (“depth”). Orthoptic and pleoptic therapies were then indicated to recover from those abnormal states of binocularity.
Once simultaneous (binocular) perception (considered the most elementary degree of binocularity) had been detected, binocular fusion was measured, especially its amplitude, i.e., fusional convergence and the several types of fusional divergence (horizontal, vertical, and torsional).
Finally, and still using a synoptophore, the “third” (highest) degree of binocularly, stereopsis, was assessed by using binocularly fusible images with slight differences.
The arsenal of devices necessary to an ophthalmology office included an equipment to examine visual behavior through Worth’s four-dot test. Using two filters, one red (on the right eye) and one green (on the left eye), patients were asked what they saw on a panel with four lights arranged around an imaginary center: a left and a right red light (of the complementary color to the green filter, so they would not be seen by the left eye), a top green light (of the complementary color to the red filter, so it would not be seen by the right eye), and a bottom white light, visible only by the right eye (if the left was suppressed), only by the left eye (if the right was suppressed), or alternately. Finally, the bottom light (white) was perceived as red if the right eye was the “dominant” or “fixing” eye, or green if these conditions fit the left eye. (See comments on the “Arthur Jampolsky” section.)
Regarding treatment, the synoptophore had what were called Haidinger’s brushes, the image of a “shadow” (produced by polarized light seen through polarizing filters) going through a circle at the frontal plane — a technique used to stimulate the fovea to treat eccentric fixation and amblyopia. With the same purpose, euthyscopy was used, which was a form of direct ophthalmoscopy with intense peripheral lighting, except for the central area, preserving it so this region would then be the only one functionally “available” to fixate optotypes in front of the eye that underwent this treatment. A variant with a similar principle was pleoptic therapy with after-images, using a bright flashing light to “blind” (ephemerally) the peripheral retina, but preserving the central regions of the retina. The type and magnitude of deviations (in the absence of binocular suppression) were assessed by Hess-Lancaster screens.
Although it was not a strict rule, for deviations of relatively large angles, surgeons preferred to operate one of the eyes and later complement the correction of the remaining deviation by operating the other eye. That was also the routine for associated horizontal and vertical deviations: one of the deviations was corrected first and the other was corrected on another date. Conjunctival openings were semilunar, distant from the limbus; muscles were sutured to the sclera using catgut 4-0 (later chromic catgut, and then 5-0). Scarring granulomas were common. After surgery, occlusion lenses with central holes were used to “induce” centralized fixation binocularly.
Reflecting the close relationship between strabismus care and the exercise of orthoptics, the USP Ribeirão Preto Medical School Orthoptics Course was created in 1967, but it was short-lived, being extinct shortly after my return from studies at the Institute of Ophthalmology of the University of London (1969-71).
In any case, and despite the massive influence of sensory aspects on the examination and treatment of strabismus, my study interests were aimed at the influence of accommodative stimuli on the horizontal oculomotor balance (leading to convergence). Thus, my early studies were on accommodation5, convergence6-8, and on the synkinetic relationship between these two functions9-18. These more specialized studies resulted in the proposal for a new clinical trial19 and in the annual award from the Brazilian Society of Ophthalmology (the Adaga “August Lohnstein” Prize, 1970) to one of the articles20.
The intimate influence of accommodation on the oculomotor balance required — as it still requires —knowing refractometry absolute values. In fact, it was a “golden rule” to prescribe total correction of hyperopia, mainly for esotropia, since some cases could be completely resolved by this procedure (“purely accommodative” esotropia); others could be resolved by additional correction lenses “to see near” (bifocals, for “hypo-accommodative” esotropia, with high AC/A ratios); and, finally, in cases in which these optical corrections failed to neutralize far and near deviations, surgery was indicated, but exclusively to fix the “nonaccommodative” component, that is, what remained after total hyperopia correction. Therefore, in order to assess total (or absolute) refractometry values, cycloplegia was induced by 1% atropine eyedrops three times a day (morning, afternoon, and evening) for three consecutive days prior to the exam. A curious note is that this usage was very well accepted, although it required a second visit to complete the (refractometry) examination and even though the induced cycloplegia persisted for about two weeks, hindering school and visual performance of the children (and adults) examined; and, lastly, although this practice could be dangerous, since patients or their caregivers were handed a bottle of eyedrops (5 ml) with a total content of atropine (50 mg) equivalent to four times the potentially lethal dose for a 10 kg child21. However, a more interesting fact is that, despite all these inconveniences, this procedure could be considered insufficient to produce total cycloplegia. Actually, in subsequent refractometry for control a few months after the total correction of hyperopia, it was not uncommon to find greater hyperopia values, justifying the belief that an even more rigorous cycloplegic procedure was necessary. For this reason, even an eight-day atropinization was proposed22 (although, in this study, only five of 41 cases presented an additional difference of 0.75 D in hyperopia with eight-day atropinization, compared with three-day atropinization).
With this hypothesis of insufficiency of three-day atropinization to achieve total cycloplegia, I invited a Bolivian ophthalmologist who had already completed his specialization in Colombia, but wished to broaden it in Brazil, and had proven to be excellent in refractometry measurements, to participate in a study about this procedure. In this study, each of us independently registered the value of the refractometry conducted by the other (who was blinded to this value). Patients should use 1% atropine eyedrops, one drop in each eye three times a day for ten days, being re-examined in the 3rd, 5th, 7th, and 10th days. They were divided randomly into three groups and had a refractometry on day zero (before the atropin onset) about 60 to 90 minutes after instillation of an eyedrop. Group I received five drops of 1% cyclopentolate [2-(dimethylamino) ethyl 2-(1-hydroxycyclopentyl)-2-phenylacetate] in each eye (one every three minutes) + 0.05% hyoscine; Group II received three drops of 2% homatropine (bromide), one every three minutes; and Group III received two drops of 1% atropine (sulfate), one every five minutes. In data analysis, at the end of the study, the refractometries conducted by both examiners had significantly similar “double” measurements. And, to a certain disappointment regarding the hypothesis to be proved, the measurements made on the 3rd, 5th, 7th, and 10th days were also very similar to each other; the effect was not potentialized nor accumulated with continued doses. And, for an even greater surprise, the initial measurements in any of the groups were virtually “identical” to those after extended atropinization. That is, regardless of the drug used, the same cycloplegia was achieved, not increasing with classical atropinization (three days) nor with continued doses22,23. These results led to the proposed change from the classical method of cycloplegia for strabismus to an immediate (in-office) method, but still suggesting the preferred use of atropine23 and that, on this day, it be instilled three times24. Cyclopentolate would only replace atropine in cycloplegia later. A young man from a South American country could not dare more than this.
ARTHUR JAMPOLSKY
He was not the only one to influence the development of strabismology in Latin America, but he is the one who developed it the most in mode, quality, and intensity, and is rightly recognized for it.
Jampolsky created and modeled the Smith-Kettlewell Institute of Visual Sciences (now Smith-Kettlewell Eye Research Institute) in San Francisco, a center for advanced research in the field of ocular motility that soon became the reference for whoever wished to delve into the science (more than in the art) related to strabismus. With a great ability to explain and convince, Jampolsky transformed practices and ways of thinking and acting. With brief, logical, and even tautological arguments, he taught: “If someone plans a single surgical correction, he (or she) may have to perform a second one. But if the initial plan is to perform two, he (or she) will perform at least two; and perhaps will have to perform three (or more).” “If someone plans a correction of the horizontal deviation and not of the vertical one, the remaining (and expected) vertical deviation will help decompensate the horizontal one again.” And there are other quotes as these ones, to conceptualize that strabismus surgical planning should contemplate full correction of quantity and type at once. The “end of orthoptics” in Latin America is attributed to him due to quotes such as: “Why use Worth’s four-dot test? The type of strabismus presented already predicts the result of the exam” (an obvious conclusion, after a simple reflection on the purpose of the test). “The doctor should examine the patient, and not delegate it to others” (learning by doing). “It is unfair to say we do not have a synoptophore in the Smith-Kettlewell Institute of Visual Sciences (SKIVS); we do, in the museum” (to demystify the importance of this instrument and emphasize the teaching that tests should be performed with eye fixations to objects in the “real” space, in front of the patient). Two quotes from Argentinian physician Alberto Ciancia, who later became president of the International Strabismological Association, illustrate the situation back then quite well: “If Jampolsky is right, we will advance twenty years; if he is wrong, we will go back twenty years.” And later: “Before Jampolsky, the study of strabismus was simply dreadful; after Jampolsky, it became dreadfully simple.”
In the strabismology practiced at the time, a field in which technological advances were not prevalent, the famous Latin American ingenuity (to some extent stimulated by the lack of strict control standards for innovations and paradigm breaking) could be showing its merits and need for incentive. And it was precisely Jampolsky — who always held the studies presented in the Latin American Council on Strabismus (CLADE) conferences in high regard — who was one of the first to value studies conducted here and show respect for them. His mentions of Latin American strabismus studies in his superb conferences, and his participation in round tables of other world conferences, as well as the emphasis he gave to their latinamerican authors, were a gift to their self-esteem and confidence.
I particularly owe Jampolsky one of the highest honors I ever received. In 1972, A. Edward Maumenee (1913-98), head of the Wilmer Institute of the famous Johns Hopkins University (Baltimore, MD), asked Jampolsky whom should he invite to replace the very respected Gunter K. von Noorden (1928-2017), who had been the head of the Strabismus Division and was leaving for the Baylor College of Medicine (Houston, TX)3. Jampolsky referred me. I was then asked to teach a course on strabismus, so the faculty at the Wilmer Institute could give their opinion. After the course was over, Maumenee proposed a six-year contract to me (which I found too long, unsure whether my family would adapt to Baltimore) and mentioned that I should dedicate the first years to reorganizing the outpatient and surgical services, without a lot of time for research. I would have to resign from the university and be far from my family and affective roots in Brazil, which scared me because it seemed like a point of no return. I asked him some time to decide. From Baltimore, I headed to San Francisco to get to know the Smith-Kettlewell Institute of Visual Sciences and personally thank Jampolsky for this almost unbelievable referral. While we talked, he noticed my indecision and was generous: “Come to Smith-Kettlewell.” I was surprised at this distinguished invitation: “To do what?” “Whatever you want.” “For how long?” “As long as you want.” “When?” “Whenever you want.” There could not be a more enticing proposition, and that was how I made my decision. I went to SKIVS (1974-75). And I appreciate that this has been my history.
Thus began a new phase of my academic life, which coincided with a major shift in the way strabismology developed.
THE MECHANISTIC PERIOD
At the time when orthoptics was at its peak, studies regarding “forces,” “elasticities,” “tensions,” “velocities,” “accelerations,” “work,” “energy,” “vectors,” and “matrices” were being designed, influenced by orthoptics itself, with greater association to topics of dynamics and physics than to psychobiology25-29 for which a mathematical language was required. These topics became preponderant in strabismology and shed a new light on it. More knowledge was being accrued regarding eye mechanics, in particular studies on forces acting on the oculomotor system and their effects. These forces will be presented separately herein although the dissociation of these component forces of the oculomotor balance is artificial and even contradictory because there is a close interaction between the so-called “active” forces (related to the innervational control of the system that, in turn, controls the position and movement of the eye) and “passive” forces (caused by the components of the periocular structures). For example, a specific muscle relaxation “allows” the eye to rotate in one direction, while its contraction rotates the eye in the opposite direction; however, because the muscle distends with relaxation, this “allowed” rotation is simultaneously restricted. But the fact that studies focus on either one of these forces than on both justifies the convenience of describing them separately.
A) Active forces
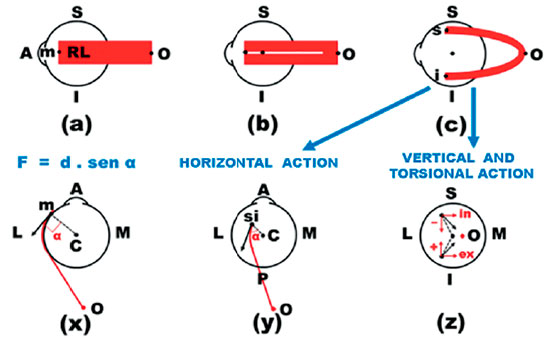
Jampolsky first visited Brazil in September 1971 (16th Brazilian Congress of Ophthalmology, Campinas). I recall his flattering comments about my presentation during a symposium on “vertical deviations,” when I spoke about “Investigation and diagnosis of vertical deviations”. It is possible that, on that occasion, I referred to my previous observations about the inconsistency of the classical Parks test, the gold standard for the diagnosis of the “muscle responsible” for a vertical deviation. But the praises were for a concept that introduced the presentation: that there were four eye elevator muscles (and not just the superior rectus muscle and the inferior oblique muscle) and four eye depressor muscles (and not just the inferior rectus muscle and the superior oblique muscle). The two additional muscles, in both cases, were the horizontal rectus muscles (medial and lateral). The observation did in fact confront the notions that prevailed regarding the actions of the extraocular muscles because they had been defined by the well-known diagrams of Márquez and Van der Hoeve30,31 (Figure 1) and explicitly reinforced by the teachings of one of the most studied text books, which attributed a single horizontal action to the horizontal recti muscles: “Droit externe. Il est abducteur et c’est là sa seule action.” “Droit interne. Il est adducteur et c’est là sa seule action.”30
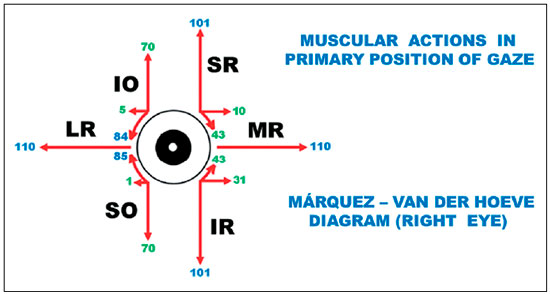
The idea was not original; it revisited the dynamic approach to muscle actions of Castanera Pueyo31 (as opposed to the static approach that prevailed at the time). This notion that the actions of an extraocular muscle vary according to the direction in which the main visual axis is pulled (in fixation) was based on the vectorial distribution of the force applied to the eye, originating from the contraction Krewson27 had analyzed the vector components of the force of an extraocular muscle (E0M) at different points of fixation, but he limited his study to a single (horizontal) gaze direction. Boeder28,29 took into consideration the total work performed by an EOM in different gaze positions, but he did not investigate the components in the fundamental planes. Therefore, I decided to cover all aspects, i.e., the different actions of each EOM (horizontal, vertical, and torsional) represented in a frontal plane, and how they could vary depending on the eye movement itself. This meant starting by studying the various systems that could define the ocular rotations32 (it is interesting that a consensus on which a referential system should be adopted as standard has not yet been reached), and by performing a generic mathematical analysis of the eye rotations33 to finally study the vector components of the force for each EOM in the different eye positions, represented in a frontal plane, with values up to 50 degrees in each cardinal direction, from the primary position of gaze34. The next step was the calculation of the length of each muscle (to determine the state of its contraction or relaxation) and of the work it performed (from the primary position of gaze at each position in space)35; the relationships between the arc of contact (between the muscle and the sclera), and the resulting rotation36. The last step was the study of the variation of the force exerted by an EOM for the visual axis to locate a given direction in space (starting from the primary position), which corresponds to an integration of the vectorial components of its action in each of the three fundamental planes of analysis (horizontal, vertical, and frontal, for the torsional actions)37, and the respective performed work38. The publication of this series was preceded by a paper with a synthesis of such studies39.
Concomitant to this study of active forces, which are the result of muscle action mediated by the oculomotor innervation, a concept of passive forces (relative to movement restriction)40 and how they relate to each other to form a self-regulated system41 was addressed (a study that was awarded the Barbosa da Luz Prize at the 19th Brazilian Congress of Ophthalmology in 1977) was also developed. The result of this study was a holistic concept about the complete integration of EOM functioning. In fact, on reexamination of Sherrington’s law of reciprocal innervation, it became obvious that the action of a muscle, such as adduction through the contraction of the medial rectus, was only possible with the simultaneous relaxation of its antagonist, the lateral rectus muscle; in fact, in Type-I Duane syndrome, eye adduction is significantly decreased by the simultaneous contraction of the lateral rectus. Hence, it was postulated that the lateral rectus muscle was also an acting muscle (through relaxation) in adduction, i.e., adduction was primarily initiated by the medial rectus muscle, aided by synergistic muscles (the superior and inferior recti), and allowed by the relaxation of the respective opponents (the direct antagonist, lateral rectus muscle; and the indirect antagonists, obliques). Similarly, elevation was initiated by the superior rectus muscle and the inferior oblique muscle (being irrelevant for the concept whether the inferior oblique muscle has a primary or an adjuvant role in elevation), aided by the horizontal recti muscles (medial and lateral), and allowed by the relaxation of the respective antagonists (the inferior rectus and the superior oblique muscles). Thus, the EOMs involved in elevation are neither only the two classically accepted muscles (the superior rectus and the inferior oblique muscles), nor four (when including the horizontal recti muscles), but all the six muscles (now including the role of the inferior rectus and the superior oblique muscles in relaxation).
Another argument for this conception is that this interaction among the EOMs is not only casual but also indispensable for a pure rotation (in a single plane) to occur. Indeed, for a pure elevation, the superior rectus, the main elevator muscle, must be activated. However, this muscle produces, also, adduction and an incycloduction. The simultaneous relaxation of the inferior rectus, --- a depressor muscle, which contraction produces also, adduction and excycloduction --- would favor elevation, but it would be accompanied by abduction, which could eventually counteract adduction by the superior rectus, and by incycloduction, which is also promoted by the superior rectus. Conversely, participation of the obliques (contraction of the inferior oblique leading to elevation, abduction, and excycloduction and relaxation of the superior oblique leading to elevation, adduction, and excycloduction) would provide a combination of elevation and excycloduction (to counteract the incycloduction brought about by the vertical rectus muscles). The horizontal effect (abduction by the contraction of the inferior oblique muscle and adduction by the relaxation of the superior oblique muscle) would eventually be compensated by a supposed symmetry of action of such antagonist muscles. In any case, under circumstances wherein this supposed symmetry of the opposed horizontal actions (of the vertical recti and obliques) has to be admited (for example, in tertiary positions of gaze), horizontal imbalances (adduction or abduction) would also occur. Thus, as an example, the prevailing participation of the horizontal action muscles is necessary to ensure that a rotation (for example, upwards and to the right) occurs. In other words, one muscle group would produce one type of action (the vertical rectus muscles generating vertical action but accompanied by unwanted horizontal and torsional actions, the annulment of which requires the active participation of the oblique muscles (to compensate for the undesired torsion associated) and of the horizontal recti muscles (to compensate for the undesired horizontal action asssociated).
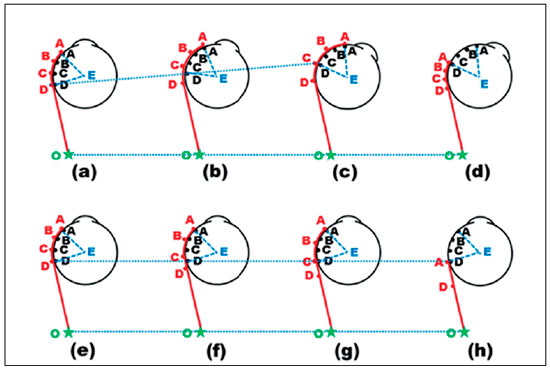
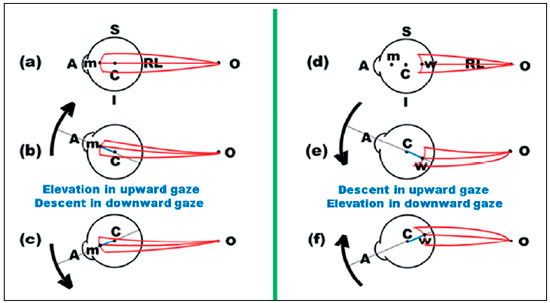
Each pair of directly antagonistic muscles (vertical recti, horizontal recti, and oblique muscles) exhibits main actions in the primary position of gaze, which are respectively opposed, each action being favored by the contraction of one muscle and relaxation of the other according to Sherrington’s law. Hence, the horizontal action is potentiated by the horizontal recti, the vertical action by the vertical recti, and the torsional action by the obliques. In the case of the vertical recti and oblique muscles, the torsional action of the former and the vertical action of the latter, although significantly reduced relatively to the main actions (vertical and torsional actions, respectively), are also potentiated by Sherrington’s law, and this is the reason why these four muscles are called “cyclovertical” muscles. For example, the stimulation of the vertical recti generates elevation and small incycloduction, or depression and small excycloduction. Conversely, the stimulation of the oblique muscles produces small elevation and excycloduction or small depression and incycloduction. These combinations suggest the possibility of distinct nerve stimulations for the activation of these muscles as diagnostic elements of their functions. For example, elevation causes the activation (contraction) of the superior rectus and of the inferior oblique (and the relaxation of their antagonists), whereas the stimulation for the incycloduction of that eye through a reflex pathway by tilting the head toward the ipsilateral shoulder causes the activation (contraction) of the superior rectus and of the superior oblique (and the relaxation of their antagonists). Elevation in abduction, with tilting of the head toward the ipsilateral shoulder (i.e., an eye movement made in a direction that corresponds to the horizontal) would therefore lead to greater stimulation of the contraction of the superior rectus specifically. Thus, the diagnostic ocular rotations corresponding to the maximum innervation for the other underactive muscles in cases of vertical deviations would be in horizontal directions (on head tilting) (Figures 3 and 4).
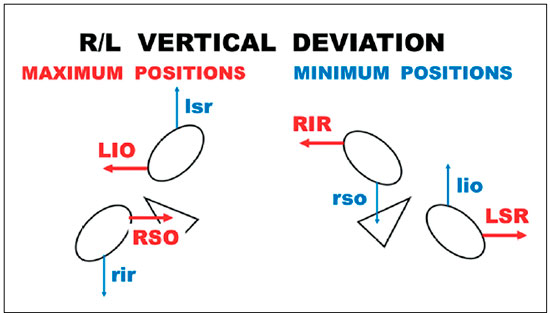
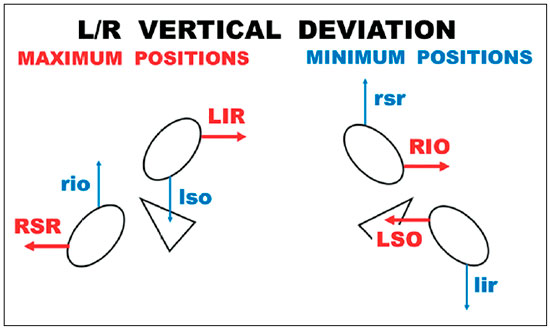
A1) Application of the concepts of active forces
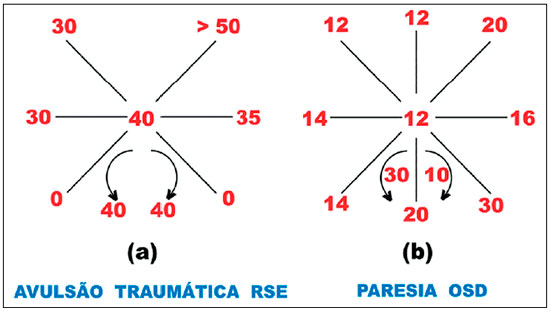
It is precisely the possibility of potential activations of the cyclovertical muscles in different positions of the gaze that generated Parks’ proposal42 for the differential diagnosis of which of them could be used to demonstrate the predominant muscle underaction in cyclovertical strabismus. It is unequivocally an elegant and simple test based on three steps. The first step corresponds to the simple determination of the type of deviation (L/R or R/L) to begin the reasoning based on only four (potentially underactive) muscles among the eight cyclovertical muscles under study. For example, in a R/L deviation, EOMs considered as potentially underactive are the right inferior rectus (RIR), the right superior oblique (RSO), the left inferior oblique (LIO), and the left superior rectus (LSR). The second step is measuring the deviation in the lateroversions (to the right and to the left). If, for example, the deviation is greater in levoversion, the predominant underaction must be ascribed to the RSO or to the LSR. Then, there is the third and last step, with head tilting to the right (greater stimulation of the RSO) or to the left (greater stimulation of the LSR), known as Bielschowsky’s maneuver43. However, it should be noted that Bielschowsky proposed the maneuver specifically and only for the diagnosis of a superior oblique muscle palsy.
Notwithstanding, there are conceptual flaws in (a) studying diagnostic positions of cyclovertical muscles by testing their functions through ocular movements in the horizontal plane (second step of Parks’ maneuver) and not through their classical diagnostic positions, wherein the innervation supplied to them is substantially greater; (b) considering the function of these muscles in Bielschowsky’s maneuver but with fixation oriented by straight ahead gaze (third step of Parks’ maneuver), i.e., with “attenuated” stimulations rather than “accentuated” stimulations, in both cases (second and third steps of the maneuver); and finally, (c) not specifying which eye should be fixating in each condition. Thus, there is no logical basis for this widespread test (Parks’ test). However, its greatest flaw will discussed below (“diagnostic pairings”).
Indeed, it was by the disciplined and constant use of this test in the diagnosis of cyclovertical deviations that illustrative examples of the gross errors in its conception and application were found44-46, which was confirmed by other authors47-48. But to show the shortcomings of Parks’ test in the diagnosis of vertical deviations, the examples presented by his own group to the American Academy of Ophthalmology49 (Figure 2) may suffice, which, by the way, support the alternative proposal suggested by me (see Figures 3 and 4).
A2) Diagnostic pairings
Two practical conclusions emerge from Hering’s and Sherrington’ laws, which have been completely accepted, for the diagnosis of an underactive muscle in strabismus (due to paresis or action restricted by opposite forces), which are as follows:
a) Deviation is more marked when the fixing eye contains the (most) underactive muscle.
b) Deviation is greater in the direction of the action of the (most) underactive muscle.
Therefore, in paresis of the right lateral rectus, deviation is more marked with right-eye fixing and in right gaze (abduction of the right eye).
In fact, these two “golden” rules for the diagnosis of strabismus do not stipulate that the deviation only exists in these conditions but, rather, that it is most pronounced in them; nor do they state that only one muscle is underactive. It follows that, in this specific case, the deviation should be less marked under opposite conditions, i.e., two other complementary “golden” rules are valid:
c) The deviation is less marked when the fixing eye does not contain the (most) underactive muscle.
d) The deviation is less marked in the direction opposite to that of the action of the (most) underactive muscle.
This means that in paresis of the right lateral rectus, the deviation is less marked with left eye fixing and in left gaze. However, this condition is precisely that wherein a deviation caused by the paresis of the left lateral rectus would be more pronounced. On the other side, in paresis of the left lateral rectus, the deviation is less marked (in right gaze and with right-eye fixing) precisely in the conditions wherein paresis of the right lateral rectus would cause more pronounced deviation. In other words, these two muscles (RLR and LLR) form a diagnostic pair wherein the conditions under which they should be maximally and minimally stimulated are antagonistic.
In fact, in an esodeviation, the underactive muscle(s) (due to paresis or restriction) should be RLR, LLR, or both. Thus, only two diagnostic conditions need to be studied, i.e., that of the RLR (deviation in right gaze, with the right-eye fixing) and that of the LLR (deviation in left gaze, with the left eye fixing). If there is a clinically significant difference between them, the greater deviation indicates the muscle whose action is more deficient. If they are relatively similar, it cannot be concluded that one of the muscle’s underaction predominates the other.
Similarly, for an exodeviation, the underactive muscle(s) (due to paresis or restriction) should be RMR, LMR, or both. Thus, only two diagnostic conditions need to be studied, i.e., that of the RMR (deviation in left gaze with the right-eye fixing) and that of the LMR (deviation in right gaze with the left eye fixing). If there is a clinically significant difference between them, the greater deviation indicates the muscle whose action is more deficient. If they are relatively similar, it cannot be concluded that one of the muscle’s undercation predominates the other.
An identical procedure can be performed with regard to vertical deviations, wherein the action of the vertical recti predominates. In a R/L deviation, the test conditions would be those of RIR (deviation in downward gaze with the right-eye fixing) and those of LSR (deviation in upward gaze with the left eye fixing). In a L/R deviation, the test conditions would be those of LIR (deviation in downward gaze with the left eye fixing) and those of RSR (deviation in upward gaze with the right-eye fixing).
But what about the oblique muscles? The best condition to study them is through ocular torsions, which are difficult to provoke (they are not voluntarily engaged and their magnitudes are small through reflex pathways), difficult to observe (rotation around the longitudinal ocular axis), and to measure (prisms do not apply to them). Therefore, the procedure in clinical practice includes assessing the function of the oblique muscles using their horizontal components (e.g., the variation of the horizontal deviation in the sagittal plane; the so-called horizontal variations in “A” or “V”) or, primarily, their vertical components. Vertical deviations caused by the oblique muscles are not very pronounced but are greater in adduction than in abduction (wherein the predominant action of the vertical recti is even greater), and this is therefore an option to study these muscles. Thus, a vertical deviation caused by the underaction of the the RSO, i.e., a R/L deviation, is greater in downward gaze and to the left with the right eye fixing, and is less marked in upward gaze and to the right with the left eye fixing, a condition that is related to the greatest deviation originated by an underaction of the LIO. These two antagonistic conditions correspond, therefore, to the diagnostic pair RSO-LIO in the R/L deviation. In this deviation the pair of vertical recti (RIR and LSR), is also involved, whereas in the L/R deviation two diagnostic pairs (pair of obliques and pair of vertical recti) should be assessed (Table 1).
However, the maximum stimulation can be even further accentuated if the labyrinthine stimulation of ocular torsion is triggered by adequate head tilting. Indeed, on right head tilting, the incycloductors of the right eye (RSO and RSR) and the excycloductors of the left eye (LIO and LIR) are stimulated. On left head tilting, the incycloductors of the left eye (LSO and LSR) and the excycloductors of the right eye (RIO and RIR) are stimulated. The combination of the stimulation of a muscle through ocular rotation to its classical “diagnostic position” with an adequate head tilt resulted in the proposal of studying the diagnostic positions with the head tilted 50-54 (Figures 3 and 4).
As the author of this concept of diagnostic methods in strabismus, especially that of diagnostic pairs, I was distinguished with an invitation to present them at the I.S.A.-C.L.A.D.E. conference in the joint congress of these two entities55.
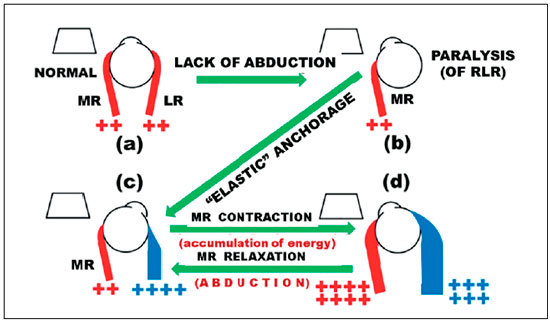
A3) Rotations in the opposite direction relative to the original
Another simple and direct application of the concept that all muscles can “produce” all (any) actions is the use of forces of the medial rectus muscle (i.e., a muscle ascribed as purely concerned to adduction) to produce abduction. In fact, assuming a complete loss of action of the lateral rectus muscle due to its anatomic absence or to an innervational palsy, the principle of recovering its action is to “anchor” the eye to the orbit in a position of abduction (the desired position to which the eye may reach) through an extendable device like a spring or an elastic. Through the innervational stimulation of the medial rectus muscle the eye can be brought to the primary position by a centripetal rotation (and can even surpass it in a greater adduction). This movement of centripetal adduction leads to the accumulation of potential energy (originated from the medial rectus muscle) in the expandable elastic device, and that energy can be recovered later when the medial rectus muscle relaxes, promoting abduction (centripetal and/or centrifugal depending on the point from where it starts). The theoretical foundation of this idea was developed in a sequence of publications56-62, and its application was explored in studies conducted by me in Ribeirão Preto63, 64 and by Collins et al. in San Francisco65-67, with the difference being solely the orientation of the traction. In fact, a “direct” traction of the device was preferred at the Smith-Kettlewell Eye Research Institute (S.K.E.R.I.) to produce abduction: the agent for pulling the eye was attached to the temporal sclera in front of the center of ocular rotation, and it was attached to the orbit behind this center of rotation, on the temporal side, a technique with which I started (four patients operated in 1982 and one patient operated in 1983 with the implantation of helicoidal steel springs)63 (Figure 5). Subsequently, I used a “reverse” double traction: the agents for pulling the eye (silicone threads) were fixed to the sclera on the medial side in front of the center of ocular rotation, and to the orbit in front of the center of ocular rotation on the temporal side, by two fascicles (a superior fascicle and an inferior fascicle)64.
It is interesting how in the excitement of rescuing ductions, the monocular results, which, by the way, were satisfactory and confirmed the principles, blinded us all for so long, to the extent that we did not pay attention to another basic principle. We (Scott, Miller, and Collins from the S.K.E.R.I, and myself) were invited to participate in a closed and very high-level meeting in San Francisco, focusing on the engineering of ocular movements. Because we were the only speakers in the section of “ocular prostheses,” I felt obliged to present an in-depth theoretical insight into the topic to befit the attending scholars, and therefore, I talked about binocular movements, or versions68. To my constraint, I realized, through theory and not through a simple observation, that while the adduction movement of the treated eye is hampered (by the elastic restriction), Hering’s and Sherrington’s laws apply to the normal eye, as intended by nature, and cause it a wider movement. Hence, there is no possibility of obtaining conjugated binocular movements, unless (but this is unthinkable) one creates a “conjugated” defect in the “good” eye to hinder its adduction, i.e., paralyzing the corresponding adduction of the normal eye and “correcting” it by using an elastic device. My consolation was that I realized this before the researchers of S.K.E.R.I., who, at the start of their presentation (which was scheduled following mine), were already deeming it outdated69. This line of research has then been shut, but the idea that a muscle could provide a rotation in the direction opposite to that which is normally expected remained.
B) Passive forces
With the exception of the examination of a possible rotational restriction of the ocular movements by the “test of passive ductions” to confirm it or rule it out, passive forces were not considered to have an important role in oculomotor balance. But by the study with which the accumulated forces during such passive ductions could produce ocular movements in the absence of muscle tones (active forces) --- for example under general anesthesia during surgery to correct strabismus, i.e., the study of centripetal rotations or (passive) spring-back rotations70 --- allowed the development of a new method to study the forces involved in oculomotor balance. Therefore, analysis of the centripetal movement was now being performed instead of (or complementary to) the simple assessment of “resistance” to centrifugal ocular rotation. While, previously, surgery was only seen as a therapeutic procedure, from that time it also gained a diagnostic value due to the improving knowledge of the problems that caused visual axis deviation and planning of their correction. It is very likely that the term “passive forces” was used for the first time in the rationale for this method71.
The point of passive balance, or the measure of the deviation under general anesthesia, is determined by the mean of the final positions of the centripetal movements in opposite directions (for example, from symmetrical points of passive abduction and passive adduction). Thus, for a deviation measuring +20° (in the waking state), a distinction can be made between a “purely tonic” deviation (when, under anesthesia, the measure of the deviation is 0°), a “mechanical” deviation (when, under anesthesia, the deviation remains identical, i.e., +20°), and a “mixed” deviation (when, under anesthesia, the deviation is between 0° and +20°). In addition, the observation of the amplitude and/or the velocity of the spring-back “centripetal” movements (which may vary, but, usually, are directly proportional to each other), could allow collecting information regarding the contraction capacity of the muscles (related to their elasticity). For instance, if the point of passive balance was 0° but resulted from centripetal rotations ending in +10° (from the centrifugal adduction) and −10° (from the centrifugal abduction), the condition should be deemed as different from another measure with the same point of passive balance (0°), but obtained from the mean of centripetal rotations ending in +20° and −20°. In the former case (greater centripetal rotations), this would mean more “elastic” or tense muscles, which would therefore respond more to procedures that debilitate or strengthen their actions and, therefore, bring about greater surgical results than those obtained with identical procedures in the latter case (less elastic or looser muscles). The unquestionable prognostic improvement provided by the results of these surgical (but diagnostic) procedures altered the conduct of performing the surgery based solely on a previously established plan and going forward with it, without any modifications. In summary, peroperative data based on the acting “passive” forces guided not only the selection of the muscles that should undergo intervention but also the extent of these interventions.
B1) Muscle elasticity as an explanation of surgical results
An interesting surgery introduced at that time was the Faden operation72 (German for “thread operation”), wherein the eye was fixed to the sclera, far from its anatomic insertion, without actually detaching it. The surgery was theoretically equivalent to a recession of the insertion (a “new” insertion, relative to the original one) but with a “magnitude” equal to that of a resection of the same value (muscle tension should not be altered with the procedure). The aim was to reduce the arc of functional contact by correcting, for example, an esodeviation in near fixation, without changing the oculomotor balance in far fixation. An unexpected problem was that the modification of deviation in far fixation also occurred. Moreover, the values of correction of deviations were, apparently, not related to the “magnitude” of the operation (that is, the distance between the original insertion and the new muscle-scleral suture).
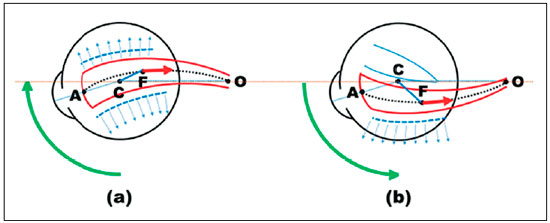
In 1981, I was invited to discuss a presentation of De Decker (probably the most renowned about the subject and with its greatest casuistry) at the Wenner-Gren Center Symposium (Stockholm)73, and I suggested that the explanation for the apparent incongruities should probably lay in the manner the surgery was performed. In fact, the suture was not made with the eye in the primary position, which in effect would not change muscle tension, but rather by pulling it to bring forward the region where the muscle would be sutured to the sclera, to ease the procedure. Therefore, the muscle was distended in a manner that the site of its insertion into the sclera corresponded to a recession that was effectively greater than it appeared. This difference basically depended both on the extent to which the eye was rotated and on the elasticity of muscle (Figure 6)74.
B2) Influence of other periocular structures on eye rotations
The influence of the structures surrounding the EOMs and between them (fasciae and intermuscular membranes) on muscle actions was an additional object of analysis. The theoretical calculations with regard to each of them (corresponding to the eye rotation from the primary position of gaze to a specific direction in space)34-39 implied that in the desired ocular movement, the muscle could slide freely over the sclera, always occupying the arc of a maximum circle (the smallest distance between two points on the surface of a sphere). However, this displacement is limited by the fasciae and intermuscular membranes to a greater or lesser degree. The concept that is currently discussed as muscle pulleys was already foreseen back in 1978, when “the effect of structures of restriction on the direction of the force of application of a muscle” was shown pictorially (Figure 8, p.15)7. The conclusion was that “the sectioning of intermuscular membranes would allow the muscle to slide more freely over the eyeball during its rotations, thereby modifying the distribution of forces between the distinct planes” (Figure 7).
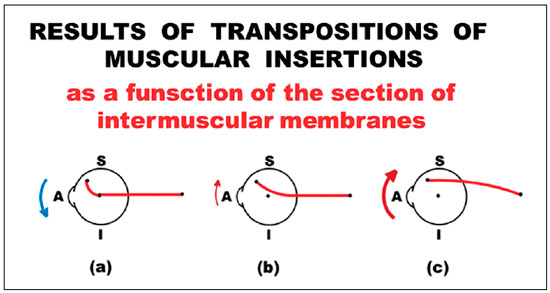
This notion of the point of application of force on the eye was reintroduced in a more generic presentation on ocular kinetics (in another Wenner-Gren International Symposium in Stockholm, in 1987). Depending on whether the sectioning of the intermuscular membranes is performed (or not) and how it is performed, the direction of a muscle’s action may be inverted76. At the Master Conference of the Congress of the 25th Anniversary of the Spanish Strabismological Association (Madrid, 1996), although this made up a minor part of the presentation, new graphical elements were added to show how the status of integrity of these membranes that act as “pulleys” influences the positioning of a muscle on the eye, both by altering its action in the various gaze directions and by having an effect on its potential transpositions77,78 (Figure 8).
However, the presentation of 1987 in Stockholm76 also included discussions about concepts, such as the “arc of rotation” which had also been foreseen61 to replace the concept of “arc of contact,” that still prevailed; as well as the influence that ocular translations, even if small, have on ocular rotations, namely by limiting them.
C) Clinical applications
A summary of the mechanisms of action of various surgical procedures for the correction of strabismus was presented in a lecture at the XII CLADE Congress (Buenos Aires, 1996). The different methods and their fundamentals were assessed with respect to the following:
A) Changes in the plane of muscular action
1) Changes in the relative position of the muscle and eye;
2) Changes in muscle length;
3) Rigid spacer;
4) Myoscleropexias (faden operations);
5) Association of resection and hang loose sutures;
6) New combinations.
B) Changes of the plane of muscular action
1) Transpositions;
2) Relative transpositions;
3) Oblique insertions.
C) Rotational moment changes
1) Changes in contractile force;
2) Changes in the moment arm;
3) Changes in the angle of force application.
D) Effects of non-muscular structures
1) Influence of connections between muscle and eye (foot-plates);
2) Influence of connections between muscles (intermuscular membranes);
3) Influence of connections between the orbit and eye or its muscles;
4) Restraining devices.
The difference between “changes in the plane of muscular action” and “changes of the plane of muscular action” can be determined by the amount of the insertion recession. In fact, a simple recession, with no change of the plane of muscular action (Figure 9), leads to possible changes in muscular action75.
Among several other methods (some of which are original), is noteworthy the bifid insertion of a muscle (done symmetrically with respect to its original plan of action) in order to weaken the muscular action by reducing the moment arm and the angle of application of the force79 (Figure 10).
A proposition to increase the arm with which the force is applied to the eye is also considered as a possibility of changing the moment of rotation; the possible advantages and disadvantages of this technique are discussed. In this paper, the use of “atropine in dilutions of 0.01%–0.05% to produce cycloparesis and thus increase the AC/A ratio” is also suggested in order to change the innervation command (to change the contractile force of the muscle) (Bicas et al., 1978).80 Indeed, this atropine dilution was probably used for the first time in ophthalmology clinics at that time, 40 years ago. Nowadays, it is commonly used, but for another purpose, that of the prevention of myopia progression.
Another analytical review presented at the Smith-Kettlewell Oculomotor Symposium, held during the 1996 CLADE Congress, addressed the concepts of “elasticity, stiffness, and other terms” and their corresponding clinical applications.81
D) Dissipative Forces
Ocular rotations are determined by increases or decreases in the tonicities of the extraocular muscles (during its contractions or relaxations, respectively); these rotations are always mediated by stimuli from the central nervous system. The forces from which they originate, the so-called active forces (A), would continue indefinitely if there were no other forces, the so-called passive forces (P) or reaction forces, to oppose them and determine the end of movement. Muscles and other elastic structures, which elongate during a centrifugal rotation, oppose the continuity of motion and determine its interruption, accumulating the kinetic energy of motion, without requiring a new innervational stimuli to be triggered to stop the movement. The established balance then continues as long as the command for contraction of the stimulated muscle(s) persists. During relaxation of these muscles, the passive forces produce centripetal ocular rotation (spring-back rotation), which would continue as a centrifugal rotation until, again, the elastic structures providing resistance to the continuity of rotation (promoting the end of the centrifugal rotation) determine its stasis and the beginning of a new cycle, maintaining an oscillating (pendulous), harmonic movement.
However, this is not how things happen; for abduction of a certain value, it is necessary to stimulate the lateral rectus by a certain magnitude such that the rotation is limited by passive forces. When relaxation occurs, the centrifugal movement “spontaneously” ends after the centripetal rotation, without the centrifugal rotation starting and with no new innervation stimulus being triggered for the stasis. The explanation is simple; in addition to the active and passive forces, the oculomotor system has dissipative forces (D), which consume kinetic energy and transform it into heat (during friction between the moving surfaces and by distension of elastic tissues) and inelastic deformations. The equation is even simple: the energy accumulated by the passive forces is the difference between that of the active and dissipated forces (P = A − D), while the energy of the spring-back rotation equals the dissipated energy (P = D). Thus, the magnitude of the dissipative forces is usually about of the original force imparted by the muscle triggered by the innervation stimulus (A = 2 D).
In addition to the quantitative aspect, the qualitative importance of the dissipative forces (D) is obvious; they “clear” the oculomotor system of the forces generated by a given innervation stimulus (A), allowing a new one to occur, without the need for any other renewing order. These forces are “destructive” and hence “renovating.” The idea that they can be harnessed to “destroy” (unwanted) rotations, such as those of nystagmus, is evident. This was hypothesized,82 and experiments that could substantiate this hypothesis were initiated. The proposition on which André A. H. Jorge’s doctoral thesis was based, which has subsequently been expanded82,83 and of which I had the honor of being the advisor, was justly awarded the annual Oftam–CBE Prize in 2001. New studies were published84-87 (two other doctoral theses I advised)85,87 and later awarded the Waldemar and Rubens Belfort Mattos Prize in 2010 for best paper published in the Arquivos Brasileiros de Oftalmologia (Brazilian Archives of Ophthalmology) in the previous year86.
E) Forces of Magnetic Fields
In short, one can consider strabismus as being produced by two elementary causes: mechanical restraints to ocular rotation (e.g., those produced by orbital floor fracture and Brown’s syndrome, among others) and functional deficiencies in innervation (e.g., paresis and oculomotor paralysis) and/or in muscular reaction (e.g., myopathies, muscle avulsions). In the former case, it is necessary to try to eliminate the restrictive forces. In the latter case (innervation or muscular response), the oculomotor balance may be eventually restored by weakening opposed muscular actions (insertion recessions, botulinum toxin applications, myotomies, or myectomies) or by increasing pre-existing rotational forces (muscle shortening, scleral reinsertion of detached muscles, greater convergence by stimulating accommodation). The principles of muscular transpositions to “restore” a lost rotation (for example, Hummelschein’s surgery88 or its variants) cannot withstand arguments that the response sought is only mechanical and “passive” (which, then, could be achieved by traditional procedures such as shortening the paralytic muscle), and have to admit that there are no re-learning commands (such as for abduction by the vertical recti muscles, which are synergists of adduction) so that greater oculomotor imbalances would have to be produced (e.g., unwanted vertical deviations in ocular rotations in the horizontal plane)89,90.
Procedures by which new forces might be introduced into the oculomotor system (e.g., electrical stimulation of paretic or paralytic muscles with signals picked up by rotations of the “normal” eye) have already been considered; however, these procedures present enormous technical difficulties, with possible tissue damage caused by the electric stimulation of the affected muscle, and do not present practical solutions that would encourage further studies. A theoretically possible alternative would be to make use of sufficiently strong “natural” forces (such as those of magnetic fields). This approach would have the advantage that such magnetic forces can be “ regulated” by signals from the other eye or, simply, generated by small magnets. Speculations about this subject were initially made in 198562 and later retaken due to the theoretical failure of the application of elastic artifacts to replace lost ocular rotations.68 New studies were conducted91-97, and the first interventions in humans were reported98,99, winning the Oftam–CBE prize in 199798. Experimental improvements have been described100-103, and two PhD theses on the subject have been completed under my advice104,105.
Owing to my retirement from FMRPUSP and the conviction that my vitality to work would not allow me to reach the quantities and qualities of the academic production “required” by the evaluation criteria of post-graduate courses, I chose to conclude my formal teaching activities despite the remarkable and generous invitations from my colleagues to continue working at the Department, which immensely honored me. Therefore, I interrupted my research that, I still believe, have a promising solution not only for the stabilization of nystagmus but also for the stabilization of achieved results of strabismus surgeries. This hypothesis was debated at an international symposium at the Smith-Kettlewell Eye Research Institute (2012)106, leading to a discussion on a possible wider clinical application107. (This article was quoted in a recent publication in the United Kingdom, which re-addresses the proposal for nystagmus correction, reproducing practically all of our original works and presenting yet another good result of the technique108.)
ADD-ONS
Naturally, studies on “the strabismology I have lived” are not limited to those mentioned here. Academic life confronts us with multiple challenges, and several other studies have been shared, mainly through my advice in PhD theses and Master’s degree dissertations, participations in books etc. Each of these experiences added to my learning. It is interesting to note that one subject that received particular attention (the objective register of eye movements by electro-oculography), --- which was my focus for our (academically) most important Thesis109, which was applied to the first observations of spring-back rotations, when they began to be researched at the Smith-Kettlewell Institute of Visual Sciences (1974); which led to several presentations at international congresses110-115 and publications116,117; which was the theme of the first PhD thesis under my advice118; and the subject of various courses and lectures --- have been later less valued, although did not lose its importance. Meanwhile, Master’s degree dissertations and PhD theses have studied other subjects through different approaches (in addition to those previously mentioned) such as diagnostic methods during surgery119-123, monocular and binocular sensorial studies124,125, psychophysical studies126,127, clinical methods for the diagnosis of strabismus128-133, use of botulinum toxin134,135, readjustable sutures136, tissue adhesives137, other surgical techniques138-142, study of satellite cells143and, fortunately, some others, with distinguished colleagues. The diversity of these topics testifies to the evolution of the study of strabismus throughout the years.
Proverbially, “the practice of medicine is both science and art.” Actually and specifically for strabismus practice, without losing focus on science, the art aspect possibly prevails. Indeed, for the same problems, different solutions have been proposed, each of them presenting reasonable amounts of good results, confusing the best explanations on why this might happen.
In fact, the conclusions of the Symposium on Strabismus of the XXI Brazilian Congress of Ophthalmology (Recife, 1981), which I had the honor of organizing and coordinating and for which I was awarded the Carmem Caldeira Prize by the Brazilian Center for Strabismus (CBE), was paradigmatic. I gave it the title “Knowledge and procedures on ocular motility and related functions considered indisputable,” aiming to catalog what would be considered as “certainties” by 17 Brazilian strabismologists who were then recognized as the most experienced and successful in the field. They were asked by mail to list the statements that they considered to be absolutely correct and that could not be amended. The number of “certainties” then stated was large, exceeding five hundred (although many of them had the same essence). Subsequently, these “indisputable” statements were grouped into topics and were anonymized; the total list was redistributed to all the survey participants, who were asked to attribute values to each one, ranging from “ten” (when the statement was considered to be completely true) to “zero” (when it was considered to be absolutely wrong). It was expected that the authors would (naturally) assign “ten” to their own statements but also to some of those made by other colleagues, so that statements unanimously accepted with the maximum mark could represent the set of “certainties” of the CBE. Surprisingly, only one was unanimously accepted, and it basically stated that it was preferable to prevent amblyopia than to treat it, which was practically obvious. Evidently, the method for obtaining these truths is in itself vulnerable to criticism, because one might state, for example, that “the medial rectus is an adductor muscle,” believing that this is an indisputable truth, while another might consider it questionable because this muscle also has a sagittal (vertical) action when the eye is outside the horizontal plane (and, therefore, may be attributed a sub-maximal evaluation to such statement). Nonetheless, this was a fair representation of the lack of consensus, if not in the concepts, at least in the language in which they are put.
In fact, the very definition of “strabismus” is not even consensual, giving rise to interesting controversies. For example, strabismus is often defined as the misalignment of the main visual axes (“foveal axes”) relatively to the point of space over which they should intersect. This seems to be the most usual yet insufficient conception; the visual axes can intersect over the referential point in space but with inclinations between the respective horizontal (or sagittal) planes of the eye (i.e., of vision), therefore without “horizontal and/or vertical deviations”, but with torsional deviations. Furthermore, a good binocular positioning may be observed for one (or more) point(s) in space, but not for any (which imposes a spatial condition to the concept). Moreover, visual axes may be missing (blindness) and nonetheless the patient might be referred as “with strabismus” (because of deviations between other eye axes taken as a reference). In summary, “visual axis” is a convenient and probably necessary, but insufficient and sometimes inadequate, reference to define strabismus.
Perhaps it is a purism to claim that the practicality of strabismus diagnosis and therapy be subordinated to concepts. However, at the Keynote Lecture of the XXV Brazilian Congress of Ophthalmology144 (Belo Horizonte, 2009), --- a privilege granted to the President of Brazilian Council of Ophthalmology in the previous year --- I commented, in an almost philosophical way, on the distance between theory (the “how it should be”) and practice (the “how it is”) in such an area of study. I discussed topics such as “the lack of formal rigor (that) should clearly delimit the extent and meaning of the term,” “the lack of a common understanding of which factors should prevail in the construction of this elementary requirement,” and the lack of “absolute limits between strabismus and normality.” I analyzed the conceptual aspects of the characterization of strabismus (its definition and elements, the precision of measurements and their limits, the referential coordinate systems, the primary position of the eye, the ocular movements in space, the “normal” positional asymmetries of the eye in space), and the operational aspects of these characterizations (the difficulties for the practical establishment of the so-called “primary position of gaze”—a concept that I assume to be only theoretical—and the methods of quantifying strabismus measurements). I ended up with ten “conclusions” for the pragmatic coexistence with such “epistemic dissonances.”
Evidently, being able to monitor how the muscles are positioned over the eye during eye movements (by nuclear magnetic resonance imaging); directly injecting into them substances that reduce or increase their actions; stimulating or depressing neuronal (motor and sensory) functions; and develop further knowledge from experimental work, will all bring enormous progress to the practice of strabismus diagnosis and treatment. But, concomitantly, for “strabismology” to become more and more a science, its basic concepts must be revisited. For my part, this is what (I think) I can do: in one of my most recent articles145, I addressed, in depth, one of these “dissonances” which were already previously referred146 — the imprecision of our basic unit of angular measurements (the prism-diopter) — to make it more tolerable.
REFERENCES
1. Lang J. History of European Strabismology. In von Noorden GK. The History of Strabismology. Oostende: J.P. Wayenborgh; 2002, p. 71-116.
2. Awaya S, Watanabe Y. The History of Strabismology in Japan. In von Noorden GK. The History of Strabismology. Oostende: J.P. Wayenborgh; 2002, p. 233-51.
3. Helveston EM. The History of Strabismology in The United States of America. In von Noorden GK. The History of Strabismology. Oostende: J.P. Wayenborgh; 2002, p. 119-71.
4. Almeida HC, Ribeiro GB. The History of Strabismology in South America. In von Noorden GK. The History of Strabismology. Oostende: J.P. Wayenborgh; 2002, p. 193-208.
5. Bicas HEA. Perturbações da acomodação nas heteroforias. Arq Bras Oftalmol. 1968; 31(3):75-85.
6. Bicas HEA. Avaliação da convergência total por diferentes métodos clínicos. In Livro Jubilar do Prof. Hilton Rocha. Rio de Janeiro: Pongetti; 1971, p. 219-35.
7. Bicas HEA, De Sordi GB. Estudo do P.P.C. e sua importância em diferentes posições do olhar. In Estrabismo. Consejo Latinoamericano de Estrabismo. II Reunión General; 1968, p. 130-7.
8. Bicas HEA. Contribuição ao estudo da convergência assimétrica. Rev Bras Oftalmol. 1969; 28(3):219-39.
9. Bicas HEA. Relação CA/A e ametropias. In Estrabismo. Consejo Latinoamericano de Estrabismo. II Reunión General; 1968, pp. 7-8.
10. Bicas HEA. Relação CA/A e heteroforias. In Estrabismo. Consejo Latinoamericano de Estrabismo. II Reunión General; 1968, p. 8-11.
11. Bicas HEA. Estudo da relação CA/A em diferentes situações horizontais do olhar. In Estrabismo. Consejo Latinoamericano de Estrabismo. II Reunión General; 1968, p. 11-15.
12. Bicas HEA, Younam I. Análise dos componentes não fusionais da convergência. I) Considerações gerais e fatores de correção para a convergência e a acomodação. In Estrabismo. Consejo Latinoamericano de Estrabismo. II Reunión General; 1968, p. 25-28.
13. Bicas HEA, Younam I. Análise dos componentes não fusionais da convergência. II) Resposta convergencial total. In Estrabismo. Consejo Latinoamericano de Estrabismo. II Reunión General; 1968, p. 29-39.
14. Bicas HEA, Younam I. Análise dos componentes não fusionais da convergência. III) Relação CA/A. In Estrabismo. Consejo Latinoamericano de Estrabismo. II Reunión General; 1968, p. 40-50.
15. Bicas HEA, Younam I. Análise dos componentes não fusionais da convergência. IV) Relação CP/D. In Estrabismo. Consejo Latinoamericano de Estrabismo. II Reunión General; 1968, p. 51-59.
16. Bicas HEA, Younam I. Análise dos componentes não fusionais da convergência. V) Variações conjugadas das relações CA/A e CP/D. In Estrabismo. Consejo Latinoamericano de Estrabismo. II Reunión General; 1968, p. 60-61.
17. Bicas HEA. Apreciação de diferentes métodos clínicos na avaliação das heteroforias e da relação CA/A. Rev Bras Oftalmol. 1969; 28(2):119-39.
18. Bicas HEA. Acomodação, Convergência e Relação CA/A. Bol Assoc Bras Ortopt. 1970; 2:18-100.
19. Bicas HEA, De Sordi GB. Novo método semiológico da oculomotricidade em não-estrábicos para avaliação de discretos desequilíbrios e incomitâncias. In Anais do XV Congresso Brasileiro de Estrabismo. Porto Alegre; 1969, p. 445-55.
20. Bicas HEA. Comparação entre o P.P.C. e o P.P.A. em várias situações horizontais do olhar. Rev Bras Oftalmol. 1969; 28(4):303-16.
21. Olson KR. Manual de Toxicologia Clínica, 6ª ed. Porto Alegre: AMGH Ed. Ltda.; 2014, p. 59.
22. Zeniquel JA, Ham O. Algunas consideraciones sobre el examen de la refracción com cicloplegia atropínica. A. Soc Oftalmol Hisp Amer. 1967; 27(7):624-7.
23. BicasS HEA, Zegada JA.Análise de vários esquemas de cicloplegia atropínica. . In Estrabismo. Consejo Latinoamericano de Estrabismo. II Reunión General; 1968, p. 82-87.
24. Bicas HEA, Zegada Pereira JA. Cicloplegia imediata ou atropinização de três dias? In Anais do XV Congresso Brasileiro de Estrabismo. Porto Alegre; 1969, p. 457-65.
25. Robinson DA, O’Meara DM, Scott AB, Collins CC. Mechanical components of human eye movements. J Appl Physiol. 1969;26:548-53.
26. Scott AB. Extraocular muscle forces in strabismus. In The Control of Eye Movements, Bach-y-Rita P, Collins CC, Hyde JE. New York: Academic Press; 1971, p. 327-42.
27. Krewson WE III. The action of the extra-ocuklar muscles. A method of vector-analysis with computations. Trans Am Ophthalmol Soc. 1950; 48:443-86.
28. Boeder P. The co-operation of extraocular muscles. Am J Ophthalmol. 1961; 51: 469-81.
29. Boeder P. Co-operative action of extraocular muscles. Brit J Opthalmol. 1962; 46:397-403.
30. Hugonnier R, Hugonnier S. Strabismes. Hétérophories. Paralysies Oculo-Motrices. 10ª ed. Paris: Masson; 1965, p. 98.
31. Castanera Pueyo A. Estrabismos y Heteroforias. Fisiopatología de la visión binocular. 3ª ed. Madrid: Editorial Paz Montalvo; 1968, p. 98-9.
32. Bicas HEA. Estudos da Mecânica Ocular. I – Sistemas de definição das rotações oculares. Arq Bras Oftalmol. 1981; 44(1):18-25.
33. Bicas HEA. Estudos da Mecânica Ocular. II – Análise das rotações oculares. Arq Bras Oftalmol. 1981; 44(1):26-36.
34. Bicas HEA. Estudos da Mecânica Ocular. III – Componentes vetoriais da força de cada músculo nas rotações oculares. Arq Bras Oftalmol. 1981; 44(1):37-43.
35. Bicas HEA. Estudos da Mecânica Ocular. IV – Comprimento muscular e trabalho respectivo em função das rotações oculares. Arq Bras Oftalmo. 1981; 44(1):44-49.
36. Bicas HEA. Estudos da Mecânica Ocular. V – Relação entre a variação do arco de contacto de um músculo e a rotação ocular respectiva. Arq Bras Oftalmol. 1981; 44(1):50-54.
37. Bicas HEA. Estudos da Mecânica Ocular. VI – Resultante dos componentes da ação muscular em torno de cada eixo de movimento, durante uma rotação ocular. Arq Bras Oftalmol. 1981; 44(1):55-60.
38. Bicas HEA. Estudos da Mecânica Ocular. VII – Distribuição do trabalho muscular numa rotação ocular. Arq Bras Oftalmol. 1981; 44(1):61-64.
39. Bicas HEA. Funções rotacionais dos músculos extra-oculares. Arq Bras Oftalmol. 1980; 43(4): 118-27.
40. Bicas HEA. Considerações sobre o estudo das forças passivas do olho. In Souza-Dias C, Anais do V Congresso do Conselho Latino-Americano de Estrabismo. 1976, pp. 48-61.
41. Bicas HEA. Análise da Mecânica Ocular. Arq Bras Oftalmol. 1978; 41(3):116-24.
42. Parks MM. Isolated cyclovertical muscle palsy. Arch Ophthalmol. 1958; 60(6):1027-35.
43. Bielschowsky A. Lectures on Motor Anomalies of the eyes. II. Paralysis of individual eye muscles. Arch Ophthalmol. 1935;13:33-59.
44. Bicas HEA, De Sordi GB. Contradições nos resultados de testes diagnósticos dos desequilíbrios verticais. In: Anais XVI Congresso Brasileiro de Oftalmologia, vol. I; 1971, p. 132-8.
45. Bicas HEA, Ferreira A, Silva MLM, De Sordi GB, Wehbe I. Considerações sobre um novo método de estudo dos desvios verticais. I. Comparações com diagnósticos de outros métodos. Rev Bras Oftalmol. 1974; 33(1):113-30.
46. Bicas HEA, Ferreira A, Silva MLM, De Sordi GB, Wehbe I. Considerações sobre um novo método de estudo dos desvios verticais. II. Influência das inclinações de cabeça sobre os valores dos desequilíbrios nas posições diagnósticas. Rev Bras Oftalmol. 1974; 33(1):131-48.
47. Kushner BJ. Errors in the three-step test in the diagnosis of vertical strabismus. Ophthalmology. 1989;96:127-32.
48. Kushner BJ. Diagnosis of isolated cyclovertical muscles palsies according to the method of Bicas. Binoc Vis Eye Muscle Surg. 1994; 9(4): 255-60.
49. Harley RD, Parks MM, Manley DR, Chan GH, Calhoun JH. Surgical management of the cyclovertical muscles including the A and V patterns. Manual for Course 39 – Ophthalmol. – Annual Meeting of the American Academy of Ophthalmology and Otolaryngology; 1974.
50. Bicas HEA. Nova técnica para estudo dos desequilíbrios cicloverticais. In: Actas III Congreso CLADE, Mar del Plata; 1971, p. 127-30.
51. Bicas HEA. Um método diagnóstico dos desequilíbrios verticais. In: Memórias del IV Congreso del CLADE, México; 1974, p. 234-43.
52. Bicas HEA. Estudo das diagonais diagnósticas nos desvios verticais. In: Anais V Congresso do CLADE; 1976, p. 465-73.
53. Bicas HEA. Discussion of some diagnostic tests for vertical deviations. Rev Lat Amer Estrab. 1979; 3(3): 67-76.
54. Bicas HEA. Diagnóstico de las desviaciones verticales. In Gómez de Liaño F, Ciancia AO. Encuentro Estrabologico Iberoamericano. Madrid: Once, 1992, p. 248-54.
55. Bicas HEA. The Laws and Rationales of the Oculomotor Balance. In Faber JT. Strabismus 2006. Proceed. of the Joint Congress of the International Strabismological Association ISA and the First Extraordinary Meeting of the Latinamerican Council of Strabismus CLADE. Rio de Janeiro: Cultura Médica; 2006, p. 39-68.
56. Bicas HEA. Princípios teóricos de substituição de ação rotacional de músculo extra-ocular. I – Generalidades. Arq Bras Oftalmol. 1984; 47(4):154-9.
57. Bicas HEA. Princípios teóricos de substituição de ação rotacional de músculo extra-ocular. II – Posição de equilíbrio e balanço de forças: esquemas representativos. Arq Bras Oftalmol. 1984; 47(4):164-9.
58. Bicas HEA. Princípios teóricos de substituição de ação rotacional de músculo extra-ocular. III – Amplitude de rotação facultada por um dispositivo mecânico contraposto à ação de um músculo são. Arq Bras Oftalmol. 1984; 47(5):175-81.
59. Bicas HEA. Princípios teóricos de substituição de ação rotacional de músculo extra-ocular. IV – Relações quantitativas entre forças aplicadas e rotações obtidas. Arq Bras Oftalmol. 1984; 47(6):195-200.
60. Bicas HEA. Princípios teóricos de substituição de ação rotacional de músculo extra-ocular. V – Modelos de implantação de artefatos elásticos. Arq Bras Oftalmol. 1985; 48(1):9-13.
61. Bicas HEA. Princípios teóricos de substituição de ação rotacional de músculo extra-ocular. VI – Efeitos de translação ocular e suas causas. Arq Bras Oftalmol. 1985; 48(1):14-22.
62. Bicas HEA. Princípios teóricos de substituição de ação rotacional de músculo extra-ocular. VII – Emprego de forças geradas por campos magnéticos. Arq Bras Oftalmol. 1985; 48(2):37-47.
63. Bicas HEA. Resultados de uma proposta de substituição de ação de músculo extra-ocular, por implantação de artefatos elásticos. Rev Bras Oftalmol. 1984; 43(3):85-99.
64. Bicas HEA. A surgically implanted elastic band to restore paralyzed ocular rotations. J Ped Ophthal Strab. 1991; 28:10-13.
65. Scott AB, Miller JM, Collins CC. Mechanical model applications. In Gregersen E. Transactions of the 124th Meeting of the European Strabismological Association. Copenhagen: Juncodan Tryk Aps; 1984, p. 1-8.
66. Collins CC, Jampolsky A, Scott AB. Artificial muscles for extraocular implantation. Invest Ophth Vis Sci (Suppl), 1985;26:80.
67. Collins CC. Design of artificial muscles for extraocular implantation. In Castanera de Molina A. Proceedings of the First Symposium on Advances in Strabismus Surgery. Barcelona: Instituto Castanera; 1985; p. 234-70.
68. Bicas HEA. Replacement of ocular rotational forces. In Scott AB. Mechanics of Strabismus. A Symposium on Oculomotor Engineering. San Francisco: The Smith-Kettlewell Eye Research Institute; 1992, p. 269-85.
69. Scott AB, Miller JM, Collins CC. Eye muscle prosthesis. In Scott AB. Mechanics of Strabismus. A Symposium on Oculomotor Engineering. San Francisco: The Smith-Kettlewell Eye Research Institute; 1992, p. 287-95.
70. Jampolsky A, Bicas HEA. Balancing of tonic and mechanical forces in strabismus surgery. The X Panamerican Congress of Ophthalmology. Puerto Rico; 1975.
71. Bicas HEA. Considerações sobre o estudo das forças passivas do olho. In: Souza-Dias C. Anais do V Congresso do Conselho Latino-americano de Estrabismo; 1976, p. 48-61.
72. Cuppers C. The so-called Fadenoperation. In: II Congress I.S.A. Marseille. Difff. Gen. Libr. Paris-Marseille; 1974, p. 395.
73. De Decker W. The “Faden” Operation. In Lennerstrand G, Zee DS, Keller EL. Functional Basis of Ocular Motility Disorders. Proceedings of a Wenner- Gren Center and Smith-Kettlewell Eye Research Foundation International Symposium. Stockholm: Pergamon Press; 1982, p. 173-84.
74. Bicas HEA. Comments. In Lennerstrand G, Zee DS, Keller EL. Functional Basis of Ocular Motility Disorders. Proceedings of a Wenner-Gren Center and Smith-Kettlewell Eye Research Foundation International Symposium. Stockholm: Pergamon Press; 1982, p. 207-10.
75. Bicas HEA. Fisiopatologia da motilidade ocular extrínseca. I – Sistema mecânico ou passivo. Rev Lat Amer Estrab. 1978; 2(2):7-16.
76. Bicas HEA. Kinetics of the Eye. In Strabismus and Amblyopia. In Lennerstrand G, von Noorden GK, Campos EC. Proceedings of The Wenner-Gren International Symposium “Experimental Basis for Advances in Clinical Management”. Stockholm: MacMillan Press; 1988, p. 65-75.
77. Bicas HEA. Consideraciones sobre los factores mecánicos en la acción de los músculos oculares. Acta Estrabol. 1996; 25:161-78.
78. Bicas HEA. Interpretação dos mecanismos de ação dos procedimentos cirúrgicos em estrabismo. In Prieto-Diaz J. Anales, XII Congreso del Consejo Latinoamericano de Estrabismo. Buenos Aires; 1996, p. 297-306.
79. Bicas HEA. Resultados de uma nova técnica cirúrgica para enfraquecimento da ação muscular. In: Anais, II Congresso Luso-Hispano-Brasileiro de Oftalmologia. Rio de Janeiro; 1972, p. 107-13.
80. Bicas HEA, Midoricava R, Faria-Sousa SJ. Weak cycloplegia for correction of exodeviations. Part II : Duration of partial cycloplegia and values of the AC/A ratio. In Reinecke RD. Strabismus, Proceedings Third Meeting of the International Strabismological Association. Grune & Straton; 1978, p. 271- 85.
81. Bicas HEA. Analysis of some mechanical factors influencing the action of an extraocular muscle. In: Prieto-Diaz J. Anales, XII Congreso del Consejo Latinoamericano de Estrabismo. Buenos Aires; 1996, p. 473-8.
82. Bicas HEA. Métodos alternativos na correção de transtornos oculomotores. Arq Bras Oftalmol. 2003; 66(4):453-60.
83. Jorge AHH. Viscosidade como fator frenador de rotações. Arq Bras Oftalmol. 2003;66 (4):465-72). (Tese de Doutorado, F.M.R.P.U.S.P., 2003.)
84. Jorge AAH, Bicas HEA. Viscosidade como fator frenador de rotações. II. Estudos com carboximetilcelulose. Arq Bras Oftalmol. 2006; 69(1): 63-70.
85. Simão MLH. Avaliação de índices da mecânica ocular de coelho após injeção intraorbitária de carboximetilcelulose. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2008. Tese de Doutorado.
86. Simão MLH, Bicas HEA. Efeitos da injeção intraorbitária de carboximetilcelulose 6% em coelhos: análise histológica e da mecânica ocular. Arq Bras Oftalmol. 2009; 72:799-804.
87. Lucena MAS. Estudo comparativo de substâncias viscoelásticas que promovam estabilização do equilíbrio oculomotor sem impedir rotações. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2010. Tese de Doutorado.
88. Hummelscheim E. Uber Sehnentransplantation am Auge. Ophthal. Gesellschaft. 107; 34: 248-53.
89. Bicas HEA. Métodos para restaurar as rotações oculares em paralisias oculomotoras. In: Prieto-Diaz J. . Anales, XII Congreso del Consejo Latinoamericano de Estrabismo. Buenos Aires; 1996, p. 281-4.
90. Bicas HEA. Why the muscular transpositions should not be used? Bol CLADE. 2002; 18: 5-7.
91. Bicas HEA. Fundamentos e considerações preliminares na geração de rotações binoculares conjugadas em casos de perda de ação muscular. Rev Bras Oftalmol. 1996; 55(6):431-43.
92. Bicas HEA. Geração de rotações oculares combinadas em casos de perdas de ação muscular. Mecanismos para conjugações rotacionais. Arq Bras Oftalmol. 1996; 59(2): 119-28.
93. Bicas HEA. Geração de rotações oculares combinadas em casos de perdas de ação muscular. Modelos baseados em forças produzidas por campos magnéticos. Arq Bras Oftalmol. 1996; 59(6):550-8.
94. Bicas HEA. Studies for obtaining conjugate eye movements in cases of oculomotor paralyses. In: Prieto-Diaz J. Anales, XII Congreso del CLADE. Buenos Aires: Consejo Latinoamericano de Estrabismo; 1996, p. 551-5.
95. Bicas HEA. Forças alternativas nas paralisias oculares. In: Horta-Barbosa P. Estrabismo. Rio de Janeiro: Cultura Médica; 1997, p. 236-43.
96. Bicas HEA. Posibilidad de sustituición artificial de la fuerza muscular em casos de parálisis oculomotoras. In Arroyo-Illanes ME. Actualidades del Estrabismo Latinoamericano. México: Consejo Latinoamericano de Estrabismo; 1998, p. 313-30.
97. Bicas HEA. Parálisis oculomotoras: Perspectivas em el diagnóstico y em tratamento de las parálisis oculomotoras. In Gómez de Liaño P. Parálisis Oculomotoras: Diagnóstico y Tratamiento. Madrid: Tecnimedia Editorial; 1999, p. 181-94.
98. Bicas HEA. Ajustamentops posicionais oculares e estabilizações do equilíbrio oculomotor sem impedir rotações. Arq Bras Oftalmol. 1998; 61(3):294-303.
99. Bicas HEA. Cirurgia dos Nistagmos. In: Souza-Dias C, Goldchmit M. Anais, XIV Congresso do Conselho Latino-Americano de Estrabismo. São Paulo; 2000, p.109-16.
100.Bicas HEA, Abreu SDLR. Magnetic forces of stabilization of ocular positions and movements. Experimental studies of a method. In Scott AB. Festchrift for Arthur Jampolsky. San Francisco: The Smith-Kettlewell Eye Research Foundation; 2000, p. 177-83.
101. Abreu SLDR, Bicas HEA. Estudo comparativo entre técnicas para fixação de placa metálica em esclera de coelhos. Arq Bras Oftalmol. 2002; 65:177-81.
102. Kleinpaul ER, Bicas HEA. Estudo macroscópico e dinamométrico comparativo de implantes (ímãs recobertos) e de suas técnicas de fixação em órbitas de coelhos. Arq Bras Oftalmol. 2004; 67:519-25.
103. Kleinpaul ER, Bicas HEA. Estudo histológico comparativo de implantes (ímãs) em órbitas de coelhos. Arq Bras Oftalmol, 2005; 68: 667-73.
104. Abreu SDLR. Estudo comparativo entre técnicas para fixação de placa metálica em exclera de coelhso. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2001. Tese de Doutorado
105. Kleinpaul ER. Estudo macroscópico, dinamométrico e histológico comparativo de implantes (ímãs recobertos) e de suas técnicas de fixação em órbitas de coelhas. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2003. Tese de Doutorado.
106. Bicas HEA. How to eliminate unwanted eye movements, including postoperative drift. In: Clinical Problems in Strabismus, International Symposium. San Francisco: The Smith-Kettlewell Eye Research Institute; 2012, p. 86-7.
107. Bicas HEA. A major problem in strabismus and its possible solution. Arq Bras Oftyalmol. 2014; 77(4):250-55.
108. Nachev P, Rose GE, Verity DH, Manohar SG, MacKenzie K, Adams G, Theodorou M, Pankhurst QA, Kennard C. Magnetic Oculomotor Prosthetics for Acquired Nystagmus. Ophtahlmology. 2017;124(10):1556-64.
109. Bicas HEA. Algumas bases e aplicações da eletro-oculografia na semiologia da oculomotricidade. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1972. Tese de Livre-Docência.
110. Bicas HEA. Resultados de algumas técnicas eletro-oculográficas nos desequilíbrios da oculomotricidade. In: Actas – III Congreso del C.L.A.D.E.; 1971, p. 135-9.
111. Bicas HEA. A new test for investigation of oculomotor imbalance by electro-oculography. In: Mein J, Bierlaagh JJM, Brummelkamp-Dons TEA. Proceedings of the Second International Congress. Amsterdam: Excerpta Medica; 1972, p. 322-32.
112. Bicas HEA. A technique for assessment of binocular motor function by a modification of electro-oculargram. Trans Ophtahlmol Soc U.K.; 1972, 91: 529.
113. Bicas HEA, Sacchetin WF, Marseillan RF. Eletro-oculografia de movimentos persecutórios no plano horizontal. In: Memorias del IV Congreso del C.L.A.D.E. México; 1974, p.. 387-403.
114. Nóbrega JFC, Bicas HEA, Faria-Sousa SJ. Saccadic movements in normal and strabismic patients. In Souza-Dias C. Smith-Kettlewell Symposium on Basic Sciences in Strabismus. Mechanical and Tonic Factors on Strabismus Diagnosis and Surgery. Guarujá; 1976, p.128-50.
115. Bicas HEA. Análise do método eletro-oculográfico. In: Memorias del VI Congreso del C.L.A.D.E. Medellín; 1979, p.
116. Bicas HEA. Electro-oculography in the investigation of oculomotor imbalance. I : Basic Aspects. Vis Res. 1972; 12(5):993-1010.
117. Bicas HEA. Le déséquilibre oculomoteur etudié par systéme electro-ocyulographe. Ses procedes pratiques et son analyse clinique. In: Les Cahiers de lÓrthoptie, Vol. III. Toulouse: A.F.I.M.; 1978, p.24-61.
118. Sacchetin WF. Estudo da variação do potencial eletro-oculográfico em função do ângulo de rotação ocular. Aplicações práticas no exame do paciente estrábico). Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1977. Tese de Doutorado.
119. Faria-Sousa SJ. Equilíbrio oculomotor durante a anestesia geral. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1980. Tese de Doutorado
120. Freitas MS. Avaliação do posicionamento ocular nas diferentes fases da cirurgia de recuo muscular em pacientes estrábicos sob anestesia geral. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1981. Dissertação de Mestrado.
121. Vergueiro CF. Translação ocular forçada em pessoas normais do ponto de vista óculo-motor, sob anestesia geral. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1984. Dissertação de Mestrado.
122. Azevedo AF. Medidas do desvio ocular de pacientes com estrabismo no pré-operatório e durante indução anestésica antes e após a administração de succinilcolina. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2003. Dissertação de Mestrado.
123. Krieger FTS. Estudo da força aplicada e do respectivo estiramento em músculos retos mediais em pacientes esotrópicos com e sem restrição de movimento. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2002. Tese de Doutorado.
124. Cruz AAV. Padrões de acuidade visual. Um conceito estatístico de ambliopia. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1986. Tese de Doutorado.
125. Schelb C. Tabelas de optotipos de baixo contraste. Medida de sensibilidade ao contraste com modulação quadrada. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1989. Tese de Doutorado
126. Borges PCN. Percepção de distância absoluta em pacientes estrábicos. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1989. Dissertação de Mestrado.
127. Lima LRC. Comparação interocular na bissecção espacial de sujeitos normais e amblíopes. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1994. Dissertação de Mestrado.
128. Cruz AAV. A quantificação clínica da convergência acomodativa. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1981. Dissertação de Mestrado.
129. Diniz AS. Exotropias primárias com incomitância lateral: aspectos motores. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1985. Dissertação de Mestrado.
130. Andrade HSAB. Contribuição à metodologia de estudo das variações do equilíbrio óculo-motor horizontal sobre o plano sagital. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1988. Tese de Doutorado.
131. José LSG. Estudo de métodos diagnósticos para os desvios oculares verticais pela metodologia de Bicas. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1992. Dissertação de Mestrado.
132. Kobayashi MCN. Análise de uma técnica de medida objetiva da torção ocular. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2002. Tese de Doutorado.
133. Almeida HC. Alterações oculomotoras em pacientes submetidos à cirurgia refrativa: um ensaio prospectivo. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2003. Dissertação de Mestrado.
134. Santos EA. Toxina botulínica e força muscular isométrica. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1993. Tese de Doutorado.
135. Cronemberger MF. Aplicação de toxina botulínica em crianças com deficiências cerebrais por meio de nova técnica. São Paulo: Escola Paulista de Medicina da Universidade Federal de São Paulo, 2005. Tese de Doutorado.
136. Correa BAS. Estudo de suturas reajustáveis em cirurgias de estrabismo. Rio de Janeiro: Universidade Federal do Rio de Janeiro, 1992. Dissertação de Mestrado.
137. Correa BAS. Comparação de diferentes adesivos tissulares em cirurgias de estrabismo. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2003. Tese de Doutorado.
138. Silva LH. Transplante autólogo, homotópico, livre de músculo ocular extrínsecio com e sem uso de anti-adesivo. Estudo experimental. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1983. Dissertação de Mestrado.
139. Castro ANBV. Estudo experimental do uso de fio de silicone nos estrabismos paralíticos. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1990. Dissertação de Mestrado.
140. Kobayashi MCN. Estudo da espessura dos músculos oculares extrínsecos através da luz. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 1993. Dissertação de Mestrado.
141. Sahdo PL. Ressecção ampla da cápsula de Tenon na cirurgia do estrabismo. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2003. Dissertação de Mestrado.
142. Teixeira JM. Estudos de resistência à tração de técnicas cirúrgicas de alongamentos musculares. São Paulo: Escola Paulista de Medicina da Universidade Federal de São Paulo, 2004. Tese de Doutorado.
143. Antunes-Foschini RMS. Estudo das células satélites de músculo oblíquo inferior de pacientes com hiperfunção de músculo oblíquo inferior e de pacientes sem estrabismo. Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, 2005. Tese de Doutorado.
144. Bicas HEA. Estrabismo: da teoria à prática, dos conceitos às suas operacionalizações. Arq Bras Oftalmol. 2009;72(5):585-615.
145. Bicas HEA. A new unity for angular measurements in Strabimus. Arq Bras Oftalmol. 2014; 77(5):275-9.
146. Bicas HEA. Unidades de medida. In Bicas HEA, Souza-Dias CR, Almeida HC. Estrabismo. Rio de Janeiro: Cultura Médica - Guanabara Koogan; 2007, p. 69-72.
* Adapted from the major conference delivered at the end of the training course for specialists at the Strabos Institute in São Paulo on November 22, 2017 (The strabismus I have experienced and the strabismus you will experience, a theme proposed by the organizers of the event).
** Senior Full Professor, Department of Ophthalmology, Otorhinolaryngology, and Head and Neck Surgery of the Ribeirão Preto Medical School of the University of São Paulo.
Funding: No specific financial support was available for this study
CEP Approval: Not applicable
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
August 23, 2018.
Accepted on:
September 5, 2018.