Daniela Vaz Ferreira Gómez1; Maria de Fátima Costa Lopes2; Norma Helen Medina3; Expedito José de Albuquerque Luna4
DOI: 10.17545/eoftalmo/2018.0032
ABSTRACT
OBJECTIVE: This study aims to inform the ophthalmological community regarding the elimination of trachoma as a public health problem in Brazil by 2020. The following criteria defined by the World Health Organization should be met for the elimination of trachoma: the prevalence of trachomatous inflammation–follicular (TF) in children aged 1–9 years should be <5% and the prevalence of trachomatous trichiasis (TT) should be <2 per 1,000 inhabitants in population aged ≥15 years.
METHOD: The Ambulatory Information System of the Unified Health System (Sistema de Informação Ambulatorial do Sistema Único de Saúde; SIA/SUS) and Hospital Information System of the SUS (Sistema de Informação Hospitalar do SUS) databases were analyzed. Assessing TT indicators required an adequate reporting of procedures whose available data did not allow an accurate evaluation of the disease status.
RESULTS: It is necessary to standardize reports of the procedures related to “the surgical treatment of trichiasis with or without graft” and “the surgical correction of entropion and ectropium,” among ophthalmologists, using the main code B-94.0 (sequelae of trachoma) and secondary code H-0.20 (eyelid entropion and trichiasis).
CONCLUSION: The participation of the ophthalmological community is essential to ensure the reporting of cases to support the elimination of trachoma as a public health problem in Brazil.
Keywords: Trachoma; Epidemiological Monitoring; prevention & control; Blindness; Neglected Diseases.
RESUMO
OBJETIVO: Informar a comunidade oftalmológica sobre a eliminação do tracoma como problema de saúde pública até o ano 2020. A Organização Mundial de Saúde definiu indicadores de eliminação: prevalência do tracoma inflamatório folicular - TF em crianças de 1 a 9 anos de idade < 5% e de triquíase tracomatosa - TT inferior a 2 por 1.000 habitantes, na população ≥ 15 anos de idade.
MÉTODO: Foi realizada uma análise das bases de dados do “Sistema de Informação Ambulatorial - SIA/SUS” e do “Sistema de Informação Hospitalar - SIH/SUS”. Para cálculo do indicador relativo à TT é necessário o registro adequado dos procedimentos cujos dados disponibilizados apresentam limitações para análise de situação.
RESULTADOS: É necessário uniformizar o registro entre os oftalmologistas dos Procedimentos “Tratamento cirúrgico de triquíase com ou sem enxerto” e “Correção Cirúrgica de Entrópio e Ectrópio”, utilizando-se o Código Principal - B 94.0 - Sequelas de tracoma e Código Secundário - H 0.20 - Entrópio e triquíase da pálpebra.
CONCLUSÃO: A participação da comunidade oftalmológica é fundamental para subsidiar a documentação necessária para validar a eliminação do tracoma como problema de saúde pública no país.
Palavras-chave: tracoma; vigilância epidemiológica; prevenção e controle; cegueira; doenças negligenciadas.
RESUMEN
OBJETIVO: Informar a la comunidad oftalmológica sobre la eliminación del tracoma como problema de salud pública hasta el año 2020. La Organización Mundial de Salud ha definido indicadores de eliminación: prevalencia del tracoma inflamatorio folicular - TF en niños de 1 a 9 años de edad < 5% y de triquíasis tracomatosa - TT inferior a 2 por 1000 habitantes, en la población ≥ 15 años de edad.
MÉTODO: Se ha realizado un análisis de las bases de datos del “Sistema de Información Ambulatoria - SIA/SUS” y del “Sistema de Información Hospitalaria - SIH/SUS”. Para cálculo del indicador relativo a la TT, es necesario el registro adecuado de los procedimientos cuyos datos disponibles presentan limitaciones para análisis de situación.
RESULTADOS: Es necesario uniformizar el registro entre los oftalmólogos de los Procedimientos “Tratamiento quirúrgico de triquíasis con o sin injerto” y “Corrección Quirúrgica de Entropión y Ectropión”, utilizándose el Código Principal - B 94.0 - Secuelas de tracoma y Código Secundario - H 0.20 - Entropión y triquíasis del párpado.
CONCLUSIÓN: La participación de la comunidad oftalmológica es fundamental para subvencionar la documentación necesaria para validar la eliminación del tracoma como problema de salud pública en el país.
Palabras-clave: Tracoma; Monitoreo Epidemiológico; prevención & control; Ceguera; Enfermedades Desatendidas.
INTRODUCTION
Recently, trachoma has been estimated to cause visual impairment in 1.6 million people, of whom 400,000 developed irreversible blindness1. In addition, it is estimated that 192 million people live in endemic areas that require action to control trachoma. Trachoma is a public health problem in many poor countries and in remote areas of 42 countries in Africa, Asia, Latin America, and the South and the Middle East.
The 51st World Health Assembly [the World Health Organization’s (WHO) highest decision-making body, which annually convenes health ministers from all member countries] adopted Resolution WHA 51.11 in 1998 for globally eliminating blinding trachoma; moreover, it recommended member countries to adopt innovative approaches, particularly the intervention strategy known as SAFE, i.e., surgery for TT, antibiotics against Chlamydia trachomatis, facial cleanliness education, and environmental improvement3.
The commitment to the elimination of blinding trachoma in the Americas was reaffirmed by the member countries of the Pan American Health Organization (PAHO/WHO) in 2009 by adopting Resolution CD49.R19, which recommended eliminating blinding trachoma as part of the goals of controlling neglected infectious diseases and other poverty-related infections. This commitment was reaffirmed by the World Health Assembly in Resolution WHA 66.12 in 2013 for intensifying efforts to control the neglected infectious diseases4, 5.
For the elimination of trachoma, WHO defined the criteria that the prevalence of trachomatous inflammation–follicular (TF) in children aged 1–9 years should be <5% in endemic districts and the prevalence of trachomatous trichiasis (TT) unknown by the health systems should be <2 per 1,000 individuals in the population aged ≥15 years in endemic countries6.
In 2015, the WHO Strategic Technical Advisory Group on Neglected Tropical Diseases adopted standardized procedures to confirm and recognize the success of disease eradication, the elimination of transmission, or the elimination as a public health problem for all neglected tropical diseases.
To evaluate whether the criteria for the elimination of trachoma as a public health problem have been met in Brazil according to the indicators proposed by WHO, it is essential to analyze the epidemiological situation of TF in the evaluation units proposed and described in WHO guidelines and to assess the situation of TT along with identifying and reporting all cases. Moreover, the need of surgical interventions, immediate post-surgical follow-up, late post-surgical follow-up (1 and 2 years), and the recurrences of all surgical procedures performed in Brazil to correct cicatricial entropion should be evaluated7,8.
EPIDEMIOLOGICAL ASPECTS
Trachoma is a chronic, recurrent, inflammatory ocular disease caused by the bacterium Chlamydia trachomatis serotypes A, B, Ba, and C, which produce scars on the palpebral conjunctiva after repeated infections and may lead to the formation of entropion and trichiasis. Lesions resulting from friction may cause changes in the cornea, possibly leading to decreased visual acuity and blindness2.
In Brazil, the first region in which trachoma was detected was the Northeast (Vale do Cariri), possibly due to the deportation of gypsies from Portugal in the 18th century. Later, trachoma was introduced in São Paulo and Rio Grande do Sul, due to the arrival of immigrants from endemic European countries (especially the Mediterranean region) and Asian countries in the late nineteenth and early twentieth centuries9,10.
By the mid-twentieth century, trachoma had become a serious public health problem. Around the 1970 decade, it was assumed to have been eradicated in the state of São Paulo in the 1970s, with a residual prevalence of 0.06%. From this period, the surveillance and control of trachoma in health services in Brazil were reduced to a point that in 1999, control actions were developed in only six Brazilian states11.
The Ministry of Health conducted a study on the prevalence of trachoma among schoolchildren during 2002–2008 to determine the distribution and occurrence of trachoma in Brazil. For this study, students living in municipalities with a Municipal Human Development Index lower than the national average were selected12,13. Thus, a total of 171,973 schoolchildren were enrolled in the study. The prevalence of TF in Brazil was found to be 5.0% (95% CI, 4.7–5.3), ranging from 1.5% in the Federal District to 9.0% in the state of Amazonas13. This survey included schools from 1,514 municipalities across all five Brazilian regions. The study indicated that the prevalence of TF was ≥10% in 15.5% of the evaluated municipalities11 (Table 1).
Trachoma surveillance and control actions have been developed by municipal health surveillance teams using an active searching strategy to identify cases and promote control interventions. The affected individuals and their immediate contacts are treated with medications provided by the Unified Health System. Reportedly, the entire community should be treated when the positivity rate of TF is ≥10%11.
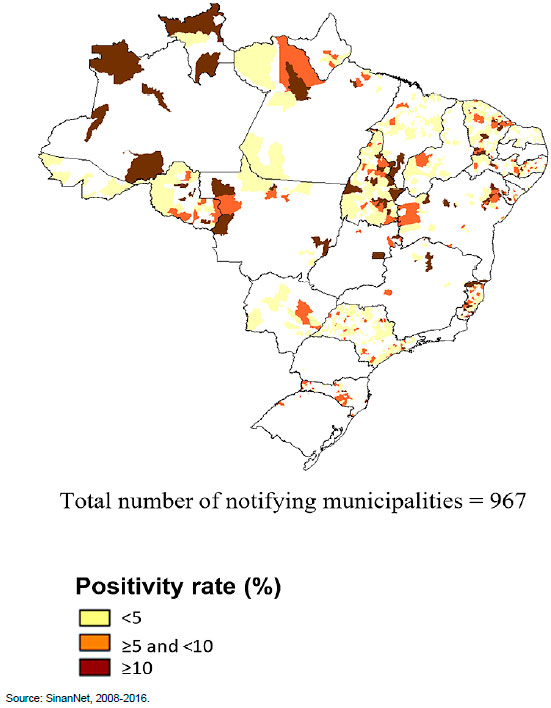
During 2008–2016, 3,908,921 examined people were registered in the National Information System for Notification Diseases (Sistema de Informação Nacional de Doenças de Notificação–SinanNet) in Brazil. Of these, 149,752 trachoma cases were identified in 967 participating municipalities, including 687, 176, and 104 municipalities with a positivity rate of <5%, between >5% and ≤10%, and ≥10%, respectively. The average positivity rate of trachoma in Brazil during this period was 3.8% (range, 2.2%–4.9%) (Table 2 and Figure 1).
A study on disease prevalence in endemic areas (epidemiological risk) and regions with high precariousness of living conditions and sanitation (social risk) will be developed during 2018–2019 to evaluate the compliance with the goals of the elimination of trachoma as a public health problem in Brazil.
With regard to the TT status in Brazil, the databases of the Department of Informatics of the Unified Health System that registers the procedures of trichiasis surgeries include the Ambulatory Information System of the Unified Health System (SIA/SUS) [“the surgical treatment of trichiasis with or without graft” (No. 04.05.01.019-2) and “the surgical correction of entropion and ectropium” (No. 04.05.01.001-0)] and Hospital Information System of SUS (SIH/SUS) [“the surgical correction of entropion and ectropion” (No. 04.05.01.001-0)].
These databases present limitations for registering procedures related to the treatment of trichiasis and surgical correction of entropion because they do not have specific fields to report the cases of trachomatous entropion and TT. Therefore, the data on TT in Brazil present limitations for assessing disease status in recent years.
From January 2015 to April 2018, 2,956 reports related to “the surgical treatment of trichiasis with or without graft” and 2,819 reports related to “the surgical correction of entropion and ectropium” were registered in the SIA/SUS with International Classification of Diseases (ICD) codes H02.0, B94.0, A71.0, and A71.9. During the same period, 784 reports on “the surgical correction of entropion and ectropium” were registered in the SIH/SUS (Table 3).
RESULTS AND CONCLUSION
A national household survey on the prevalence of TF in a sample of children aged 1–9 years, 11 months, and 29 days using the global mapping methodology of WHO is ongiong8. The areas with highest social vulnerability and epidemiological risk were identified. All of them are located in the North and Norteast regions of the country. The results of this study may help to guide the implementation of disease control actions and confirm whether Brazil has archived the indicators of elimination of trachoma as a public health problem.
It is necessary to improve the reporting of surgical procedures registered in the SIA/SUS and SIH/SUS databases because of the limitations in assessing the epidemiological status of TT.
A group of specialists in oculoplastic surgery from the Brazilian Council of Ophthalmology consensually proposed that surgical procedures should be reported with the specification of the cause of TT using the codes defined in the International Statistical Classification of Diseases and Related Health Problems, i.e., indicating the main code (B94.0, “sequelae of trachoma”) and the secondary code (H0.20, “eyelid entropium and trichiasis”) of the disease, and that these data should be filled in a specific field in the of the SIA/SUS and SIH/SUS databases.
RECOMMENDATIONS
In order to confirm the need for the elimination of trachoma as a public health problem in Brazil, all TT-related procedures, along with ICD codes, in outpatient and hospital settings should be uniformly reported by all ophthalmologists who perform surgical corrections for TT in Brazil. These guidelines should be made accessible to training centers, university hospitals, ophthalmological centers, and other ophthalmological institutions affiliated to the Ophthalmology Councils and the Brazilian Society of Ocular Plastic Surgery, among other entities.
The participation of states and municipalities in this process is fundamental, with the support to develop the actions of surveillance and control of trachoma by the intensification of treatment strategies using antibiotics in regions with a positivity rate of ≥10%, facial cleanliness education for children, and logistic support in executing and monitoring TT surgeries.
Several actions are necessary for elaborating the Dossier of Validation of Elimination of Trachoma as a Public Health Problem in Brazil, including monitoring the epidemiological situation of active diseases and sequelae, adoption of intervention measures to meet the technical indicators of elimination, and participation of health professionals.
REFERENCES
1. Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, Das A, Jonas JB, Keeffe J, Kempen JH, et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017 Dec; 5(12):e1221-e1234. doi: https://doi. org/10.1016/S2214-109X(17)30393-5.
2. WHO. World Health Organization. WHO Alliance for the Global elimination of trachoma by 2020: progress report on elimination of trachoma, 2014-2016. Geneve: Weekly Epidemiological Record. 2017; 92(26):357-68.
3. WHO. World Health Organization. 51st World Health Assembly. WHA51.11. Global elimination of blinding trachoma. Geneva; 1998. Acessado em: 27/08/2018. Disponível em: http://www.who.int/blindness/causes/WHA51.11/en/.
4. OPAS. Organização Pan-Americana da Saúde. Organização Mundial da Saúde (OMS). 49o Conselho Diretor. 61a Sessão do Comitê Regional. Resolução CD49. R19: Eliminação de doenças negligenciadas e outras infecções relacionada à pobreza. Washington, D.C., EUA, 2009. Acessado em: 27/08/2018.Disponível em: https://www.paho.org/bra/index.php?option=com_docman&view=document&category_slug=doencas-negligenciadas-975&alias=900-resolucao-cd49-r19-out-2009-0&Itemid=965.
5. World Health Organization. 66th World Health Assembly. Resolution WHA 66.12 on Neglected Tropical Diseases. 2013. Disponível: http://www.who.int/neglected_diseases/mediacentre/WHA_66.12_Eng.pdf acessado em 27 de agosto de 2018.
6. WHO. World Health Organization. Report of the 2nd Global Scientific Meeting on Trachoma. Geneva; 25-27 August, 2003. WHO/PBD/GET/03.1
7. WHO. World Health Organization. Validation of elimination of Trachoma as a Public Health Problem. Geneva; 2016. WHO/HTM/NTD/2016.8.
8. Solomon AW, Pavluck A, Courtright P, Aboe A, Adamu L, Alemayehu W, et al. The trachoma mapping project global: metodologia de um estudo de base populacional de 34 país. Ophthalmic Epidemiol. 2015; 22:214-25.
9. Freitas CA. Prevalência do Tracoma no Brasil. Rev Bras Malariol D Trop. 1976; 28:227-80.
10. Freitas CA. Bolsões hiperendêmicos de tracoma – situação atual. Brasília: Rev Bras Malariol D Trop. 1977; 29:33-76.
11. BRASIL. Ministério da Saúde (MS). Secretaria de Vigilância em Saúde. Departamento de Vigilância das Doenças Transmissíveis. Manual de vigilância do tracoma e sua eliminação como causa de cegueira. 2 ed. Brasília: Ministério da Saúde. 2014; 52 p.
12. Lopes MFC, Luna EJA, Medina NH, et al. Prevalência de Tracoma entre escolares brasileiros. Rev Saúde Pública. 2013; 47(3):451-9.
13. Luna EJA, Lopes MFC, Medina NH, Favacho J, Cardoso MRA. Prevalence of Trachoma in schoolchildren in Brazil. Ophthalmic Epidem. 2016; 23(6):360-5.



Funding: No specific financial support was available for this study
CEP Approval: Not applicable
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
November 8, 2018.
Accepted on:
November 21, 2018.