Raphael Pereira da Silva; Leonardo Dias Alencar; Carlos Augusto Moreira-Neto
DOI: 10.17545/eoftalmo/2018.0029
ABSTRACT
The clinical case presents an interesting discussion about differential diagnosis between choroidal osteoma and retinal astrocytic hamartoma. A healthy 19-year-old man presented with a dark spot on temporal field of the left eye with one month of evolution. Examination of the ocular fundus of the left eye revealed a well-circumscribed and elevated orange-yellow plaque around the optic disc and hemorrhages in the macular region. The patient was submitted to fluorescein angiography, ocular ultrasound, optical coherence tomography and optical coherence tomography angiography. The yellowish mass, the optically empty spaces and the calcifications seen in the optical coherence tomography, besides the macular hemorrhage are inherent characteristics of the two tumors, making it very difficult to reach the etiological diagnosis. An Enhanced depth imaging optical coherence tomography and a cytological evaluation through fine needle biopsy would be useful tools to clarify the diagnosis.
Keywords: Tomography Optical Coherence; Retina; Hamartoma; Osteoma; Choroid.
RESUMO
Este estudo de caso clínico apresenta uma discussão interessante sobre o diagnóstico diferencial entre osteoma de coroide e hamartoma astrocítico da retina. Um individuo saudável do sexo masculino, de 19 anos de idade, apresentou uma mancha escura no campo temporal do olho esquerdo com 1 mês de evolução. O exame de fundo ocular do olho esquerdo revelou uma placa laranja-amarelada bem circunscrita e elevada ao redor do disco óptico e hemorragias na região macular. O paciente foi submetido a angiografia com fluoresceína, ultrassonografia ocular, tomografia de coerência óptica (OCT) e angiotomografia de coerência óptica (OCTA). Uma massa amarelada, espaços opticamente vazios e calcificações foram detectados na OCT, além das hemorragias maculares que são características inerentes aos dois tumores, dificultando enormemente o diagnóstico etiológico. Uma tomografia de coerência óptica com profundidade de imagem aprimorada e uma avaliação citológica por biópsia por agulha fina podem ser ferramentas úteis para esclarecer o diagnóstico.
Palavras-chave: Tomografia de Coerência Óptica; Retina; Hamartoma; Osteoma; Coroide.
RESUMEN
Un individuo saludable del sexo masculino, de 19 años de edad, presentó una mancha oscura en el campo temporal del ojo izquierdo con 1 mes de evolución. El examen de fundo ocular del ojo izquierdo reveló una placa naranja-amarillada bastante incrustada y elevada alrededor del disco óptico y hemorragias en la región macular. Se sometió el paciente a angiografía con fluoresceína, ultrasonografía ocular, tomografía de coherencia óptica (OCT) y angiotomografía de coherencia óptica (OCTA). Se detectaron en la OCT una masa amarilla, espacios ópticamente vacíos y calcificaciones, además de las hemorragias maculares que son características propias a los dos tumores, lo que hace muy difícil el diagnóstico etiológico. Una tomografía de coherencia óptica con profundidad de imagen primoreada y una evaluación citológica por biopsia con aguja delgada pueden ser herramientas útiles al aclaramiento del diagnóstico.
Palabras-clave: Tomografía de Coherencia Óptica; Retina; Hamartoma; Osteoma; Coroides.
INTRODUCTION
Choroidal osteoma (CO) is a benign and rare tumor that is composed of mature bone cells and is more prevalent in females1. CO is often located in the juxtapapillary or macular region and is unilateral in the majority of cases2. The most common complication of CO is choroidal neovascularization (CNV), an important cause of visual loss, occurring in up to 31% of cases3.
Retinal astrocytic hamartoma (RAH) is a benign glial tumor arising from the retinal nerve fiber layer. This lesion represents the most common ophthalmoscopic finding in patients with tuberous sclerosis complex; however, this mass can also manifest as a sporadic condition that appears as a yellow–gray mass, often with minimally dilated retinal vessels, fine retinal traction, and glistening intrinsic calcification4.
CASE REPORT
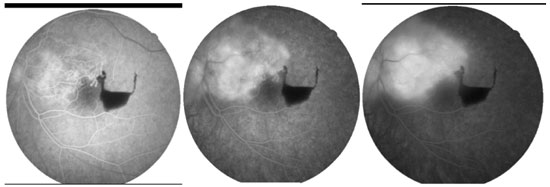
A 19-year-old Caucasian male presented with a dark spot on the temporal field of the left eye with 1 month of evolution. He had no other relevant past ocular, medical, or family history. His best corrected visual acuity was 20/20 in the right eye and 20/20 in the left eye. Examination of his anterior segment was unremarkable, in addition to a normal ocular fundus examination of the right eye. Fundoscopy of the left eye revealed a well-circumscribed and elevated peripapillary orange-yellow plaque and hemorrhage in the macular region (Figure 1A). Fundus autofluorescence (FAF) revealed a hyperautofluorescent lesion throughout the tumor extension and a fluorescent hypoauthor in the hemorrhage area (Figure 1B).

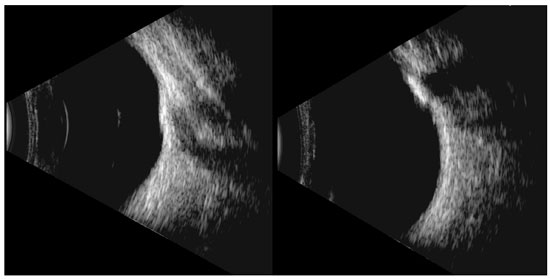
Color fundus photography, B-scan ultrasound, fundus fluorescent angiography (FFA), spectral domain optical coherence tomography (SD-OCT) (Heidelberg Engineering, Heidelberg, Germany), and optical coherence tomography angiography (OCTA) (Optovue, Inc., Fremont, CA, USA) were performed. FFA of the left eye revealed early hyperfluorescence and intense staining of the lesion associated with areas of blockage corresponding to the hemorrhage (Figure 2). The B-scan ultrasonography revealed a highly echogenic lesion with posterior acoustic shadowing (Figure 3).
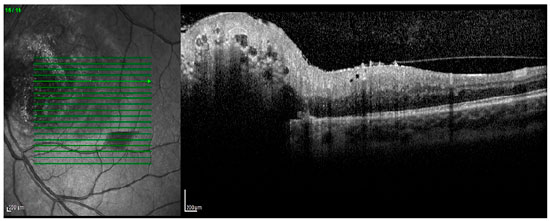
The SD-OCT revealed a well-defined retinal lesion with optically empty spaces (OESs) and the presence of hyperreflective dots (Figure 4).
The OCTA demonstrated tumor vessels in the superficial vascular plexuses, and the preretinal hemorrhage was observed in the en-face OCT (Figure 5).

The patient received three consecutive monthly intravitreal injections of aflibercept (2.0 mg). After 1 month of the final intravitreal aflibercept injections, the OCTA revealed a reduction in the bleeding area.
In addition, yellow laser photocoagulation was performed at the temporal margin of the tumor (Figure 6). The final visual acuity of the patient was 20/20, and there was improvement in the visual field defect in the left eye after 2 months of treatment.

DISCUSSION
The unique, peripapillary, yellowish lesion associated with the macular hemorrhage led us to differentiate two tumors that could be calcified, which, in this topography, are CO and RAH5.
The patient did not present systemic alterations such as tuberous sclerosis complex. Ocular ultrasound revealed a calcified lesion and a macular hemorrhage that could be caused due to a neovascular membrane secondary to CO. However, in the OCT, the lesion was located in the retina, and it was not possible to evaluate the choroid due to the shadowing caused by the tumor.
Analysis of the CO using magnified EDI-OCT images reveals a typical sponge-like pattern comprising dense hyperreflective dots spread into the hyporeflective matrix and a multilayer structure, probably because of the presence of different degrees of calcification within the tumor. It is believed that SD-OCT scanning of eyes with an amelanotic lesion in the fundus can facilitate clinicians to differentiate COs from other conditions such as sclerochoroidal calcifications, choroidal melanomas, choroidal metastasis, and choroidal lymphoma6-8.
Regarding EDI-OCT, Pichi et al. described type I as flat and generally in the nerve fiber layer, type II with slight elevation of the nerve fiber layer and retinal traction, type III with “moth-eaten” lucent areas suggestive of calcification involving the inner and outer retina, and type IV with optically empty intralesional cavities9.
RAH manifests characteristic features on an OCT, including a gradual transition from a normal retina to an optically hyperreflective mass with retinal disorganization, characteristic moth-eaten spaces, and posterior shadowing10-11.
RAH is associated with tuberous sclerosis but may appear as a sporadic tumor, and intralesional calcification occurs in about half of the cases, in addition to hemorrhages and subretinal fluid that are more common in acquired astrocytomas12.
The complications related to the presence of retinal hamartomas include vitreous hemorrhage, retinal vascular abnormalities (including telangiectasia, neovascularization, and exudation), and vitreous seeding, which is characteristically described in association with optic nerve head or epipapillary astrocytic hamartomas. According to a clinicopathologic report, vitreous hemorrhage may arise from the substance of retinal or optic nerve astrocytomas. A myriad of small vascular channels is confirmed to be pathologic13.
EDI-OCT and a cytological evaluation through fine needle biopsy could be useful tools to clarify the etiological diagnosis of this case.
REFERENCES
1. Gass JD, Guerry RK, Jack RL, Harris G. Choroidal osteoma. Arch Ophthalmol. 1978;96(3):428-35.
2. Aylward GW, Chang TS, Pautler SE, Gass JD. A long-term follow-up of choroidal osteoma. Arch Ophthalmol. 1998;116(10):1337-41.
3. Shields CL, Sun H, Demirci H, Shields JA. Factors predictive of tumor growth, tumor decalcification, choroidal neovascularization, and visual outcome in 74 eyes with choroidal osteoma. Arch Ophthalmol. 2005;123(12):1658-66.
4. Shields CL, Benevides R, Materin MA, Shields JA. Optical coherence tomography of retinal astrocytic hamartoma in 15 cases. Ophthalmology. 2006;113(9):1553-7.
5. Shields CL, Perez B, Materin MA, Mehta S, Shields JA. Optical coherence tomography of choroidal osteoma in 22 cases: evidence for photoreceptor atrophy over the decalcified portion of the tumor. Ophthalmology. 2007;114(12):e53-8.
6. Mello PC, Berensztejn P, Brasil OF. Enhanced depth imaging optical coherence tomography of choroidal osteoma with secondary neovascular membranes: report of two cases. Arq Bras Oftalmol. 2016;79(3):197-9.
7. Alameddine RM, Mansour AM, Kahtani E. Review of choroidal osteomas. Middle East Afr J Ophthalmol. 2014;21(3):244-50.
8. Yadav NK, Jayadev C, Rajendran A, Nagpal M. Recent developments in retinal lasers and delivery systems. Indian J Ophthalmol. 2014;62(1):50-4.
9. Pichi F, Massaro D, Serafino M, Carrai P, Giuliari GP, Shields CL, et al. RETINAL ASTROCYTIC HAMARTOMA: Optical Coherence Tomography Classification and Correlation With Tuberous Sclerosis Complex. Retina. 2016;36(6):1199-208.
10. Shields CL, Say EAT, Fuller T, Arora S, Samara WA, Shields JA. Retinal Astrocytic Hamartoma Arises in Nerve Fiber Layer and Shows “Moth-Eaten” Optically Empty Spaces on Optical Coherence Tomography. Ophthalmology. 2016;123(8):1809-16.
11. Mellen PL, Sioufi K, Shields JA, Shields CL. Invisible, honeycomb-like, cavitary retinal astrocytic hamartoma. Retin Cases Brief Rep. 2017. DOI: 10.1097/ ICB.0000000000000697
12. Shields JA, Shields CL, Ehya H, Buckley E, De Potter P. Atypical retinal astrocytic hamartoma diagnosed by fine-needle biopsy. Ophthalmology. 1996;103(6):949-52.
13. Kroll AJ, Ricker DP, Robb RM, Albert DM. Vitreous hemorrhage complicating retinal astrocytic hamartoma. Surv Ophthalmol. 1981;26(1):31-8.



Funding: No specific financial support was available for this study
CEP Approval: Not applicable
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
May 30, 2018.
Accepted on:
July 25, 2018.