Carlos Henrique Camara de Souza1; Lorena Aparecida Alves Pedroso2; Luciene Barbosa Sousa3
DOI: 10.17545/eoftalmo/2018.0026
ABSTRACT
The sclera is of extreme importance for the optical system comprising the outer layer of the eyeball. Several etiologies have been described for scleral thinning (ST), but this report highlights iatrogenesis through surgery with mitomycin C. Although many ST therapies have been reported, there is still no general consensus on the best treatment. The use of oral mucosa is described in the literature mainly for treating symblepharon, and to date, no study has reported its use for treating ST.
Keywords: Sclera; Mouth Mucosa; Pterigium; Transplantation.
RESUMO
A esclera é de extrema importância para o sistema óptico constituindo camada externa do globo ocular. Afinamento escleral (AE) possui diversas etiologias descritas, porém este relato traz uma importante e comum causa, as iatrogenias pelas cirurgias com aplicação de mitomicina. Muitas terapias de AE têm sido relatadas, não havendo ainda um consenso geral. A utilização de mucosa oral (MO) é descrita na literatura para tratamento de simbléfaro, principalmente, sendo que até o presente momento não há nenhum estudo relacionado ao seu uso para tratamento de AE.
Palavras-chave: Esclera; Mucosa Bucal; Pterígio; Transplante.
RESUMEN
La esclera tiene extrema importancia para el sistema óptico, ya que constituye la camada externa del globo ocular. El afinamiento escleral (AE) presenta diferentes etiologías descriptas, sin embargo este relato pone de relieve la iatrogenía por la cirugía con aplicación de mitomicina C (MMC). Muchas terapias de AE se han relatado, pero todavía no se ha llegado a un consenso general. La utilización de mucosa oral (MO) se describe en la literatura, sobretodo, para la terapia de simbléfaron, pero hasta este momento no se ha hecho ningún estudio acerca de su utilización para la terapia de AE.
Palabras-clave: Esclerótica; Mucosa Bucal; Ptegirion; Trasplante.
INTRODUCTION
The sclera plays a fundamental role in the eye because it constitutes the outer layer of the eyeball and maintains its shape and size1. Scleral thinning (ST) is considered pathological and can lead to serious risks of visual loss, depending on its severity2. The main causes of ST are autoimmune, infectious, traumatic, secondary to iatrogenesis, and surgery3, and adequate treatment is necessary to avoid worsening of this condition2. Several therapies have been described for surface disorders affecting the sclera, but there is still no general consensus2. The use of buccal/oral mucosa (OM) has been reported in the literature for treating symblepharon4, 5, and to date, no study has reported its use for specifically treating ST.
CASE REPORT
A 52-year-old male patient was admitted to the clinic of the Fundação de Banco de Olhos de Goiás (FUBOG) with pain in the left eye (LE) that had progressed after pterygium exertion surgery with mitomycin C (MMC) application. A 2-month postoperative follow-up was conducted at another hospital.
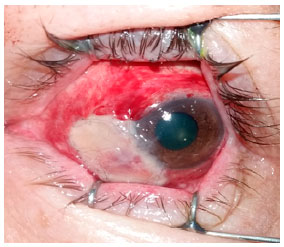
On examination, the patient presented with uncorrected visual acuity: 20/30 partial in both eyes, and biomicroscopy of the right eye showed no alterations. In the LE, the patient presented with 2+/4+ bulbar conjunctival hyperemia, an area of ST in the nasal region with a blackened base of the lesion, which was characterized as severe thinning.
The other findings were normal, including eye fundus.
The patient was indicated for correction surgery of ST with an autologous OM graft obtained from the internal region of the lower lip. The region affected by ST was measured, and an OM graft 30% larger than that measurement was marked and removed. The conjunctiva was dissected around the ST, leaving only the naked sclera, and the OM graft was placed over the region; a suture was then made using 8.0 and 10.0 nylon thread, with some interrupted and continuous stitches around the entire graft. The patient was prescribed 0.12% prednisolone eye drops 4×/day in the first week, with tapering doses every 7 days, and 0.3% ofloxacin eye drops 4×/day. The patient progressed with favorable improvement of the condition, with good vascularization of the graft in the 3rd week. After 6 weeks, the patient was prescribed 0.15% sodium hyaluronate (Hyabak ®, Laboratories THÉA, Clermont-Ferrand, France) 6×/day to the present day and 0.12% prednisolone acetate eye drops 1×/day until the 3rd month. There were no adverse/side effects of the medications used.
At 6 weeks postoperatively, the OM transplant was well vascularized and bonded, exhibiting a pinkish color, with the hyperbaric bulbar conjunctiva only at the margins of the graft.
We present the images in a chronological order: preoperative and 1st day, 8th day, 3rd week, 6th week, 3rd month, 10th month, and 18th month postoperatively, shown in Figures 1, 2, 3, 4, 5, 6, and 7, respectively.





DISCUSSION
The use of OM for ocular pathologies has attracted attention since the report of its use in rabbits6. Human studies of ocular surface reconstructions7,4,8 and complications of Stevens–Johnson syndrome have begun to emerge5. Approximately 80%–100% of cases of symblepharon treated by transplantation with OM showed positive results5.
Cases of severe ST should be treated because they present a risk of complications, such as endophthalmitis and perforation9. ST is clinically classified according to its depth into mild or superficial, when the ST is less than 1/3 of the scleral thickness; moderate, when the ST is up to 2/3 of the thickness of the sclera but the base remains white; and severe, when the ST has a darkened base and the thinning is greater than 2/3 of the scleral thickness3. Currently, ultrasound biomicroscopy (UBM), a high-resolution imaging test used to evaluate the structures of the anterior segment of the eye10, is a very effective imaging modality to measure ST; however, an experienced examiner is required for a correct evaluation2.
It is known that rabbit OM shows a positivity of p63 and Beta-1 integrin molecules, confirming the presence of stem cells in this epithelium6, and since then, studies on its use have shown 80%–100% positive results for treating complications of Stevens–Johnson Syndrome and symblepharon4,5.
Kheirkhah et al, in their study of the treatment of symblepharon grades III and IV in 32 eyes using MMC, showed that the use of OM grafts in fornices and amniotic membrane overlapping the surface of naked sclera after excision of the symblepharon resulted in improvement in all eyes that had restricted mobility, with a success rate of 84.5%, being higher in the group of lower severity (grade III symblepharon)4. In another study by Nakamura et al with 19 eyes, OM and amniotic membrane were also used for treating severe ocular surface disorders such as Stevens–Johnson syndrome and ocular cicatricial pemphigoid. Some success parameters were analyzed, such as AV improvement, conjunctivalization, and inhibition of recurrence of the symblepharon during follow-up, with positive results in 95% of cases with regard to best corrected visual acuity8. Sant’Anna et al also showed good results, such as increased lacrimal production evaluated by the Schirmer I test (73.7%), improved transparency (72.2%), and increased local vascularity (29.4%), when grafts of OM and salivary glands were used for treating severe dry eye and Stevens–Johnson Syndrome. The increase in lacrimal production was more frequent in patients who received OM graft with 10 or more salivary glands. In addition, there was an improvement of complaints such as foreign body sensation, pain, and photophobia5. Other findings such as the appearance of neovessels in the transplanted surgical site suggest the presence of a certain level of angiogenic activity7.
To the best of our knowledge, no studies in the literature to date have reported the use of OM in cases of mild, moderate, and severe ST.
Our report presents an unprecedented case of the use of OM in severe ST, secondary to the use of MMC during pterygium excision. Our patient showed clinical improvement, with resolution of the condition and satisfaction. Further studies on its application are needed to prove a good result with a higher level of evidence.
REFERENCES
1. Vurgese S, Panda-Jonas S, Jonas JB. Scleral thickness in human eyes. PLoS One. 2012;7(1):e29692.
2. de Farias CC, Sterlenich T, de Sousa LB, Vieira LA, Gomes JÁ. Randomized trial comparing multilayer amniotic membrane transplantation with scleral and corneal grafts for the treatment of scleral thinning after pterygium surgery associated with beta therapy. Cornea. 2014; 33(11):1197-204.
3. Tarr KH, Constable IJ. Late complications of pterygium treatment. Br J Ophthalmol. 1980;64(7):496-505.
4. Kheirkhah A, Ghaffari R, Kaghazkanani R, Hashemi H, Behrouz MJ, Raju VK. A combined approach of amniotic membrane and oral mucosa transplantation for fornix reconstruction in severe symblepharon. Cornea. 2013;32(2):155-60.
5. Sant’Anna AE, Hazarbassanov RM, de Freitas D, Gomes JÁ. Minor salivary glands and labial mucous membrane graft in the treatment of severe symblepharon and dry eye in patients with Stevens-Johnson syndrome. Br J Ophthalmol. 2012;96(2):234-9.
6. Hayashida Y, Nishida K, Yamato M, Watanabe K, Maeda N, Watanabe H, et al. Ocular surface reconstruction using autologous rabbit oral mucosal epithelial sheets fabricated ex vivo on a temperature-responsive culture surface. Invest Ophthalmol Vis Sci. 2005;46(5):1632-9.
7. Inatomi T, Nakamura T, Koizumi N, Sotozono C, Yokoi N, Kinoshita S. Midterm results on ocular surface reconstruction using cultivated autologous oral mucosal epithelial transplantation. Am J Ophthalmol. 2006;141(2):267-75.
8. Nakamura T, Takeda K, Inatomi T, Sotozono C, Kinoshita S. Long-term results of autologous cultivated oral mucosal epithelial transplantation in the scar phase of severe ocular surface disorders. Br J Ophthalmol. 2011;95(7):942-6.
9. Cho CH, Lee SB. Biodegradable collagen matrix (OlogenTM) implant and conjunctival autograft for scleral necrosis after pterygium excision: two case reports. BMC Ophthalmol. 2015;15:140.
10. Souza Filho ECD, Marigo Fde A, Oliveira C, Cronemberger S, Calixto N. Intraobserver reproducibility in anterior segment morphometry of normal eyes using ultrasound biomicroscopy (UBM). Arq Bras Oftalmol. 2005;68(2):177-83.

Funding: No specific financial support was available for this study
CEP Approval: Not applicable
Disclosure of potential conflicts of interes: None of the authors have any potential conflict of interest to disclose
Received on:
February 7, 2018.
Accepted on:
July 25, 2018.